Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
A Beneficial Effect of Metformin in Improving Survival Among Obese and Diabetic Patients Affected with COVID-19: Findings of A Meta-Analysis
*Corresponding author: Mashail Abdullah Alshehri, King Saud Bin Abdulaziz University for Health Sciences, Suadi Arabia.
Received: February 06, 2023 Published: March 10, 2023
DOI: 10.34297/AJBSR.2023.18.002447
Abstract
Background: Diabetes Mellitus is one of the major non-communicable diseases among patients suffering from COVID-19, which increases the likelihood of hospital admission and leads to life-threatening complications such as mortality. While Metformin has been found effective in reducing the mortality associated with COVID-19, there is a need to update the existing meta-analyses and quantitively synthesize the findings regarding the effect of Metformin in reducing mortality. Methods: We undertook a meta-analysis of 21 studies after searching for epidemiological studies systematically in PubMed/ Medline, EMBASE, and Science Direct. We used odds ratios and their respective 95% confidence interval (CI) for a binary outcome, which was mortality, to examine the effect of Metformin on mortality. Heterogeneity was assessed using the I2 statistic and Q-test statistics. We evaluated the publication bias using a funnel plot, which was further confirmed by eager test statistics. A p-value of < 0.05 was considered statistically significant. Results: Overall, the findings revealed that Metformin reduced mortality by about 35%, and the results were statistically significant (OR= 0.66; 95% CI 0.62 to 0.69; p<0.05). This revealed that patients who took Metformin had improved survival by more than one-third than those who were not given Metformin. We found a relatively higher heterogeneity with an I2 value of 85.60% (Chisquared = 138.85. The inverted funnel plot for the findings for the effect of Metformin on mortality was asymmetrical with test statistics for an eager test of -3.64 and a P-value of 0.002. Conclusion: The present updated meta-analysis revealed a positive effect of Metformin in reducing mortality among diabetic patients suffering from COVID-19. However, before implementing Metformin at a larger scale, clinicians and endocrinologists need to assess the risks versus benefits associated with Metformin for diabetic patients of COVID-19. Also, future studies are warranted to investigate the effects of Metformin for non-diabetic patients.
Keywords: Metformin, Mortality, COVID-19, Diabetes mellitus, Meta-analysis
Abbreviations: SARS-CoV-2: Severe Acute Respiratory Syndrome Coronavirus 2; T2D: Type 2 Diabetes; DM: Diabetes Mellitus
Introduction & Literature Review
Since December 2019, the world has been in chaos due to the pandemic COVID-19, resulting from respiratory syndrome coronavirus known as SARS-CoV-2 [1,2]. As a result, there are varying morbidity and mortality rates among all kinds of patients across the countries and regions [3,4]. Since then, the virus has spread over the world, infecting 4,806,299 individuals, and causing 318,599 fatalities as of the 20th of May 2020 [5]. However, nothing is known about the SARS-CoV-2 pathophysiology. It is now well established that there is a strong relationship between the virus SARS-CoV-2 and an individual’s immune system, resulting in a variety of clinical symptoms of the disease. [6] Diabetes mellitus is a metabolic condition which is caused by a deficiency of insulin production or insulin activity. Chronic hyperglycemia and abnormalities in carbohydrate, fat, and protein metabolism follow from insulin insufficiency. [7] Diabetes mellitus is classified into various subtypes, the two most prevalent of which are type 1 and type 2. [8] Both Type 1 and Type 2 diabetes cause hyperglycemia, but the way this happens is different. T1D is usually caused by an autonomic dysfunction disease in which cells in the pancreas are damaged, resulting in less insulin production. T2D, on the other hand, is caused by the body not being able to properly absorb insulin. People with Type 2 diabetes make up more than 85%–95% of all diabetes cases [9] It has been shown that people with diabetes mellitus (DM) have a higher frequency of infection. Diabetes patients are also more prone than nondiabetic individuals to have complications from these infections [10].
Further, it has also been found that people suffering from non-communicable diseases such as chronic kidney disease, cardiovascular disease, cancers, diabetes mellitus, and obesity are both at a higher risk of morbidity and mortality related to COVID-19 [3,5,6]. For example, according to previous research, inflammation-related biomarkers and inflammation responses are somewhat higher among patients suffering from diabetes mellitus than without diabetes [7]. This implies that being diabetic is a potential risk factor that determines the prognosis and progression of COVID-19. Add more about noncommunicable diseases with covid including diabetes. Diabetes Mellitus is one of the major noncommunicable diseases among patients suffering from COVID-19, which increases the likelihood of admission to the intensive care units by 14 to 32% [8]. This could possibly be due to decreased CD-4 T-cells in diabetic patients affected with SARS-CoV-2, increased expression of interleukin-6, or upregulation of angiotensinconverting enzyme-2 [9-11]. Furthermore, the mortality rate from COVID-19 is higher in patients with uncontrolled glucose levels. This suggests that medication that can reduce glucose levels and be prescribed safely among diabetic patients can be used to decrease the mortality associated with COVID-19 among diabetic patients [12]. And Metformin is one of the most prescribed medications to be used among diabetic patients [12]. Besides the hypoglycemic activity, Metformin has anti-inflammatory properties; therefore, it can reduce the creation of reactive oxygen species [13]. Through these mechanisms, Metformin can reduce the mortality associated with COVID-19.
Recently, a series of epidemiological studies have demonstrated the positive role of Metformin in decreasing mortality among COVID-19 patients [13,14]. These findings are further supported by the subsequent reviews and meta-analyses confirming the favorable effect of Metformin in decreasing mortality due to COVID-19 [13,15,16]. However, the existing meta-analyses have either included fewer studies or have missed the large observational cohort studies from various countries that are recently published in 2019 [15,16]. Given this, there is a need to quantitatively analyze the data from recently published epidemiological studies examining the effect of Metformin in reducing mortality among diabetic patients admitted with COVID-19. Thus, we undertook this meta-analysis to quantitatively analyze the data on all studies that have been carried out since the inception of the pandemic assessing the role of Metformin in reducing mortality. This is crucial because it will help policymakers and clinicians to make evidence-based decisions to improve survival among diabetic patients affected with COVID-19.
Aim of the Study
To systematically review with meta-analysis A beneficial effect of Metformin in improving survival among obese and diabetic patients affected with COVID-19.
Research Question(s)
To assess A beneficial effect of Metformin in improving survival among obese and diabetic patients affected with COVID-19.
Objectives
i. To retrieve, critically appraise and synthesize quantitative
published research focusing on the potential causal association
between Metformin in reducing mortality among diabetic
patients with COVID-19.
ii. To statistically synthesize the results of such articles, to
calculate the pooled summary estimate of the association based
on results from these studies, by conducting a meta-analysis.
iii. Methods
We undertook a meta-analysis to quantitatively summarize the existing data from epidemiological studies that assessed the role of Metformin in reducing mortality among diabetic patients admitted with COVID-19. We used updated Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines to undertake this metaanalysis [17].
Inclusion and Exclusion Criteria
The eligibility of a research article was conditional for inclusion if an epidemiological study assessed the effect of Metformin in decreasing the mortality among diabetic or obese patients suffering from COVID-19, published in English through January 2022 across different regions of the world. Furthermore, only quantitative epidemiological studies were included, with qualitative studies and studies lacking full texts being excluded. All studies that were opinions, criticisms of previous research studies, or editorials were excluded. Furthermore, studies that looked at outcomes other than mortality were excluded because mortality was our primary focus.
Information Sources and Strategy to Examine the Appropriate Research Studies
A systematic search of research studies was initiated and finished in 2022. We searched databases like PubMed/Medline, EMBASE, and Science Direct. References of the selected articles were also screened according to the eligibility criteria for additional related publications. An independent search was undertaken to scan the results for possibly suitable studies, followed by retrieving articles of the full-text articles. We considered mortality or number of deaths among diabetic or obese COVID-19 patients as the main outcome of interest. We identified a blend of Medical Subject Heading (MeSH) keywords and text words. The most prevalent search terms found in abstracts and titles comprised “metformin,” “hypoglycemic agents,” “role of metformin in COVI-19”, “metformin and COVID-19”, “effect of metformin in reducing mortality among diabetic and COVID-19”, “metformin and deaths in COVID-19”, “metformin and mortality rate in COVD-19”. This was followed by merging these major concepts using combinations (AND, OR) appropriate to the aim of the meta-analysis. The keywords included “Metformin” OR “hypoglycemic agents” OR “Biguanides” OR AND “mortality in diabetic patients COVID-19” AND “diabetic” And “Obese” AND “COVID-19” AND “Death”. In addition, to find more research articles, we used truncation (*) with the same root word. We used truncation to ensure that all possible search term variants were retrieved. To include eligible studies in the search, we also employed screens on the language (English) and the period of publication.
Data Abstraction
We imported all relevant research studies into the reference manager software (EndnoteTM) file, where every research study was evaluated, and we also used this software to screen titles for duplicates. Abstracts that did not explicitly address the study aim were not considered for full-text publication. In the end, we acquired and assessed the full-text articles of the leftover pertinent research papers. The articles that met the eligibility criteria were then abstracted and summarized using a standardized proforma. As a result, after eliminating repeats, screening titles, and abstracts, and removing papers that were outside the scope of this review as guided by inclusion criteria, we removed papers. Furthermore, the bibliography of the remaining studies was verified and examined to ensure that no valuable research articles were overlooked. The reviewers conducted the search for the articles independently, and their judgments and extracted summaries were compared to recognize and solve disagreements. Independent reviewers extracted study characteristics from eligible research articles using a standard data extraction sheet. Before beginning the data extraction process, the reviewers assessed the data extraction tables to ensure that the essential findings of the eligible studies were included. In addition, to describe the objects of the data extraction proforma, current research articles on the chosen topic were reviewed. Any disagreements between the two reviewers were resolved through mutual agreement. The abstracted data included the study title, publication year, sample size or population, country or study setting, average age with age range, gender, and study participant characteristics.
Statistical Analysis
We used odds ratios and their respective 95% Confidence Interval (CI) for a binary outcome, which was mortality, to examine the effect of Metformin on mortality. Since the outcome was dichotomous, percentages were used to compute ORs and their 95% CI. We carried out this meta-analysis using Open Meta[analyst] software. Heterogeneity was assessed using the I2 statistic and Q-test statistics [18]. The cutoffs for I2 statistics were utilized to categorize the heterogeneity as very low (0 to 25%), low (25 to 50%), moderate (50 to 75%), and high (>75%). An inverted variance statistical method and random effect model were used for this meta-analysis because of the differences in studies either due to sample size, outcome assessment, and tools to measure the outcomes. This was also confirmed by a greater degree of heterogeneity using the I2 statistic and Q-test statistics. Finally, we used random-effects models to calculate the overall effect size and its respective 95% CI to evaluate the impact of Metformin in reducing mortality [19]. Forest plots were generated to compute an individual as well as pooled effects of the intervention for the primary outcomes (mortality: Yes or NO) and to assess statistical heterogeneity. We also evaluated the publication bias visually using a funnel plot, which was further confirmed by eager test statistics. A p-value of < 0.05 was considered statistically significant.
Results
Results of the Search Strategy
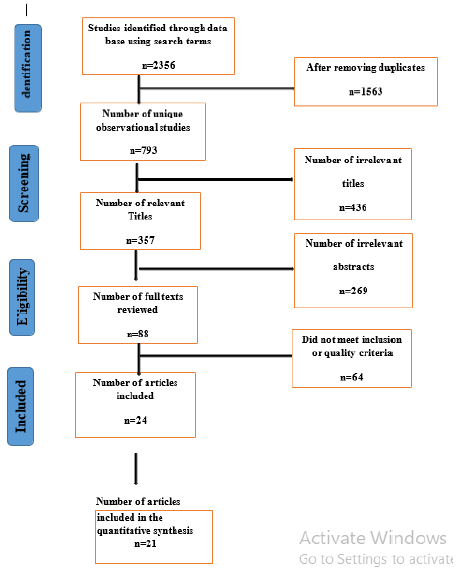
The selected articles were initially screened by titles, then by abstracts, and finally by full-text articles. Our preliminary search recognized 2356 citations in different databases, and after removing 1563 duplicates, 793 unique observational studies were screened for their titles and abstracts. This was followed by reviewing 88 full-text articles, and 64 were further excluded as these studies did not meet the eligibility criteria. Finally, we included 24 articles for qualitative synthesis, and 21 studies were incorporated in the quantitative synthesis as displayed in the PRISMA flow diagram for screening the studies (Figure 1).
Characteristics of the Eligible Studies
With respect to the study design, all studies were observational epidemiological studies, i.e., either retrospective cohort one-center or multi-center studies or cross-sectional studies. However, almost more than 95% of the studies were retrospective cohort studies as shown in Table 1. The studies were conducted in countries such as the United States of America (USA) (n=5), United Kingdom (n=3), Turkey (n=1), Spain (n=1), Brazil (n=1), Ireland (n=1), Philippines (n=1), France (n=3), Korea (n=), and China (n=6). All studies were either conducted in 2021 or 2020. For example, eight studies were conducted recently in 2020, whereas the remaining studies (n=17) were conducted in 2021, as illustrated in (Table 1). The overall sample size of all eligible research articles ranged between 131 to 2, 851, 465 with an almost similar distribution by gender. On average, the study participants were between 51.8 years to 75.6 with varying proportions of males and females in the Metformin or no metformin group. While reviewing the studies, we found that most studies included participants who were either diabetic or obese and had been admitted to the hospital with COVID-19.
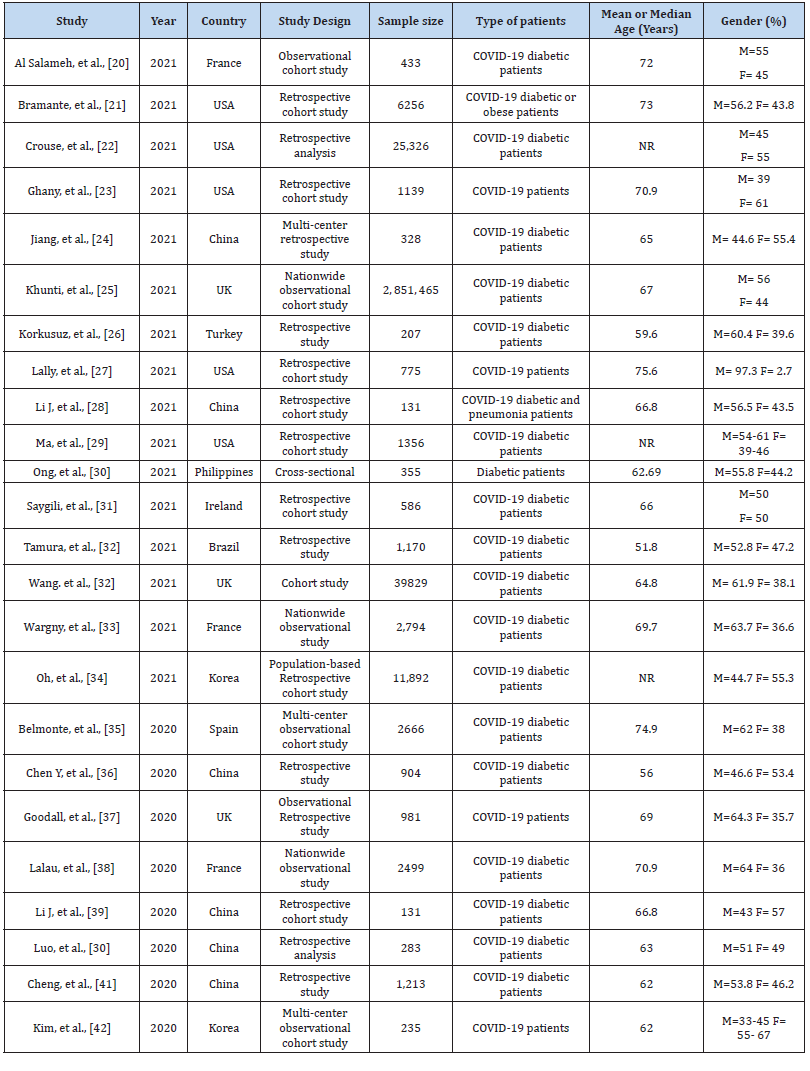
Table 1:Characteristics of the studies that assessed the effect of metformin on mortality among diabetic patients with COVID-19 (n=24).
Findings Regarding the Effect of Metformin in Reducing the Mortality
Quantitative Synthesis and Evaluation of Heterogeneity: Figure 2 shows the forest plot for the pooled results for the effect of Metformin in reducing mortality or improving the survival among patients admitted with COVID-19.
We included 21 studies to analyze the data for the effect of Metformin on reducing mortality as the remaining three studies did not have sufficient data to be incorporated in the analysis. Overall, it was found that Metformin reduced mortality by about 35%, and the results were statistically significant (OR= 0.66; 95% CI 0.62 to 0.69; p<0.05) (Figure 2). This revealed that patients who took Metformin had improved survival by more than onethird than those who were not given Metformin. However, upon assessing the heterogeneity, we found a relatively higher heterogeneity with an I2 value of 85.60% (Chisquared = 138.85), suggesting that there may be a range of factors explaining this heterogeneity.
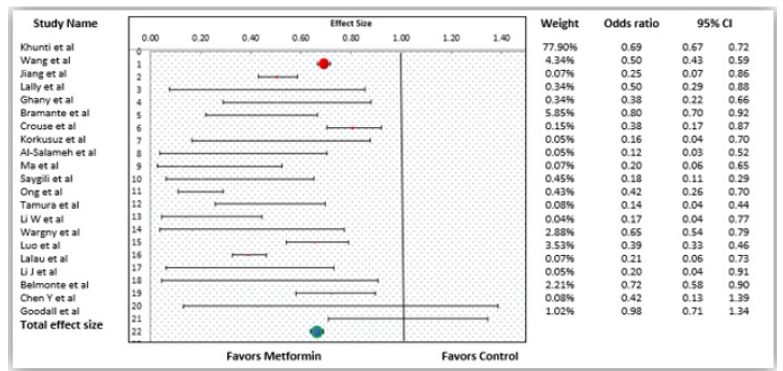
Figure 2:Forest plot showing the individual studies and overall effect of Metformin in reducing the mortality among COVID patients.
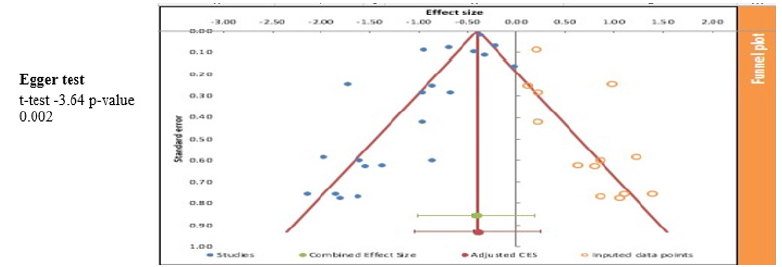
Publication bias Using Funnel Plot and Eager Test
We evaluated publication with the help of an inverted funnel plot and eager tests for the findings, as shown in Figure 3. The inverted funnel plot for the results for the effect of Metformin on mortality revealed publication bias with test statistics for an eager test of -3.64 and a P-value of 0.002. A significant Eger’s test indicated the presence of small-study effects. The asymmetrical funnel plot suggests the presence of systematic differences between the studies that are published and the studies that are not published (Figure 3).
In order to study the influence of the transmission rate λ1 of the primary communicator on the propagation process, keep other parameters unchanged, k = 0.01, λ 2 = 1 − λ1 = 0.8,μ1 = μ 2 = 0.175,β = 0.35 . Change the transmission probability of the primary communicator λ1 to 0.15 and 0.3 respectively and calculate the propagation process through MATLAB. Figure 2.2 shows the trend of the number of primary communicators, onlookers, secondary communicators, immunizers, and quitters over time under different transmission rates. The maximum value and time data of each state node are shown in Table 1.1 & Table 1.2.
The pandemic due to COVID-19 has affected the world severely, and the effects are even more drastic for diabetic patients. Diabetes is usually associated with adverse outcomes among COVID-19 patients, and this is further supplemented by a higher body mass index. Since diabetic patients are usually obese, which increases their susceptibility to getting infected by COVID-19 easily and also experiences complications more than nondiabetic and non-obese patients. This has encouraged researchers and physicians to find out ways to reduce such adverse outcomes, such as mortality. And Metformin could be one of the potential drugs that can reduce mortality among COVID-19 patients owing to its anti-inflammatory and hypoglycemic properties. Thus, in the existing pandemic crisis with changing variants of the COVID-19 virus, Metformin could be a promising therapy and a potential agent to reduce the complications, and subsequent mortality rates among diabetic patients admitted with COVID-19.
The findings of the current meta-analysis suggest that Metformin improves the survival among COVID-19 patients by about 65% and can be used to reduce the rates of deaths among diabetic patients suffering from COVID-19. The findings of this metaanalysis are analogous to the findings of a previously conducted series of reviews and meta-analyses on various outcomes including mortality. Also, the research has demonstrated that metformin use before the confirmation of COVID-19 can be beneficial to diabetic patients [22]. However, we should be mindful of the fact that all meta-analyses have been performed on observational studies, which are not free from issue of unmeasured confounding. This warrants for more interventional studies in future before making any definitive conclusions about the role of Metformin in improving the survival among diabetic patients suffering from COVID-19 patients.
The possible explanations for these consistent findings of the effect of Metformin could be either its role in reducing the oxidative damage due to anti-inflammation or in minimizing the neutrophils’ extracellular traps among diabetic patients suffering from COVID-19 [43,44]. Besides, other biological mechanisms through which Metformin can play its role are by helping in decreasing the release of cytokines, mainly interleukin 6, or it can also decrease the formation of thrombosis reduce glycemia, and help in reducing the release of inflammatory markers [13]. The COVID-19 virus leads to vascular endothelial glycocalyx damage, which is a potential mechanism for life-threatening complications and subsequent mortality [45]. This damage is prevented by Metformin as it restores the glycocalyx and protects the cardiovascular system [46, 47]. As a result of these properties, metformin can play a role in reducing the storm related to cytokines, thereby reducing the inflammation and related mortality [48]..
Strengths and Limitations
This is the large meta-analysis of its kind that provides valuable evidence regarding the effect of Metformin in improving survival among diabetic patients with COVID-19. Secondly, we updated the existing meta-analyses by including more studies from 2021, which could not be incorporated in the previously conducted meta-analyses. Third, this meta-analysis included a relatively more significant number of studies when compared to the previously undertaken meta-analysis that included less than 20 studies. However, one limitation of this meta-analysis was that all the included studies were not intervention studies; therefore, there is a threat to the internal validity of the original studies. Besides, these studies were primarily retrospective in nature, which undoubtedly warrants conducting more prospective studies. Second, the likelihood of publication bias was high, as indicated by asymmetrical funnel plots and significant eager tests, which implies that studies with negative findings or small sample sizes may not have been published. Third, studies primarily did not consider the dosage of metformin, thus there is a need to analyze the data in future to see the dose-response relationship between metformin and mortality. Besides, most of the studies were from high-income countries; therefore, we may not be able to make any firm conclusions about generalizing the results to low-income countries. Despite these limitations, we hope that this updated and large meta-analysis can provide useful insights to both physicians and policymakers to make evidence-based decisions for diabetic patients affected with COVID-19 [49-54].
Conclusions
The present updated meta-analysis revealed a positive effect of Metformin in reducing mortality among diabetic patients suffering from COVID-19. However, the presence of confounding, smallstudy effects, and possible publication bias indicate publishing and conducting randomized controlled trials to confirm the findings from existing literature on observational studies. Therefore, before implementing Metformin at a larger scale, clinicians and endocrinologists need to assess the risks versus benefits associated with Metformin for diabetic patients of COVID-19. Also, future studies are warranted to investigate the effects of Metformin for non-diabetic patients as well..
Acknowledgements
None.
Conflict of Interest
None.
References
- Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, et al. (2020) Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. Jama 323(16):1574-1581.
- Park SE (2020) Epidemiology, virology, and clinical features of severe acute respiratory syndrome -coronavirus-2 (SARS-CoV-2; Coronavirus Disease-19). Clin Exp Pediatr 63(4):119-24.
- Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, et al. (2020) Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J 55(5): 2000547.
- Choi SH, Kim HW, Kang JM, Kim DH, Cho EY, et al. (2020) Epidemiology and clinical features of coronavirus disease 2019 in children. Clin Exp Pediatr 63(4):125-132.
- (2019) World Health Organization Coronavirus Disease (COVID-19) Situation Report97.
- Dong X, Cao YY, Lu XX, Zhang JJ, Du H, et al. (2020) Eleven faces of coronavirus disease 2019. Allergy 75(7): 1699-1709.
- Moller DE, Kaufman KD (2006) Metabolic syndrome: a new view of some familiar transplant risks. Annu Rev Med 56: 45-62.
- Ralph AD, Ferrannini E, Groop L, Henry RR, Herman WH, et al. (2015) Type 2 diabetes mellitus. Nat Rev Dis Primers 1: 15019.
- Federation ID (2017) IDF diabetes atlas 8th International Diabetes Federation: 905-911.
- Carton JA, Maradona JA, Nuño FJ, Fernandez AR, Pérez GF, et al. (1992) Diabetes mellitus and bacteraemia: a comparative study between diabetic and nondiabetic patients. Eur J Med 1(5): 281-287.
- Dai M, Liu D, Liu M, Zhou F, Li G, et al. (2020) Patients with Cancer Appear More Vulnerable to SARS-CoV-2: A Multicenter Study during the COVID-19 Outbreak. Cancer Discov 10(6): 783-791.
- Lighter J, Phillips M, Hochman S, Sterling S, Johnson D, et al. (2020) Obesity in Patients Younger Than 60 Years Is a Risk Factor for COVID-19 Hospital Admission. Clin Infect Dis 71(15): 896-897.
- Huang I, Lim MA, Pranata R (2020) Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia - A systematic review, meta-analysis, and meta-regression. Diabetes Metab Syndr 14(4): 395-403.
- Xie Y, Bowe B, Yan Y, Xian H, Li T, et al. (2019) Estimates of all-cause mortality and cause specific mortality associated with proton pump inhibitors among US veterans: cohort study. BMJ 365: 1580.
- Woo A, Lee SW, Koh HY, Kim MA, Han MY, et al. (2021) Incidence of cancer after asthma development: 2 independent population-based cohort studies. J Allergy Clin Immunol 147(1): 135-143.
- Li X, Klompas M, Menchaca JT, Young JG (2020) Effects of daily treatment with acid suppressants for stress ulcer prophylaxis on risk of ventilator-associated events. Infect Control Hosp Epidemiol 41(2): 187-193.
- Ma C, Shaheen AA, Congly SE, Andrews CN, Moayyedi P, et al. (2020) Interpreting Reported Risks Associated With Use of Proton Pump Inhibitors: Residual Confounding in a 10-Year Analysis of National Ambulatory Data. Gastroenterology 158(3): 780-782.e3.
- Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, et al. (2015) Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes care 38(1): 140-149.
- Zangiabadian M, Nejadghaderi SA, Zahmatkesh MM, Hajikhani B, Mirsaeidi M, et al. (2021) The Efficacy and Potential Mechanisms of Metformin in the Treatment of COVID-19 in Diabetics: A Systematic Review. Front Endocrinol 12: 645194.
- Schuiveling M, Vazirpanah N, Radstake T, Zimmermann M, Broen JCA (2018) Metformin, A New Era for an Old Drug in the Treatment of Immune Mediated Disease? Current drug targets. 19(8): 945-959.
- Dalan R (2020) Metformin, Neutrophils and COVID-19 infection. Diabetes Res Clin Pract 164: 108230.
- Poly TN, Islam MM, Li YJ, Lin MC, Hsu MH, et al. (2021) Metformin Use Is Associated with Decreased Mortality in COVID-19 Patients with Diabetes: Evidence from Retrospective Studies and Biological Mechanism. J Clin Med 10(16): 3507.
- Yamaoka Tojo M (2020) Endothelial glycocalyx damage as a systemic inflammatory microvascular endotheliopathy in COVID-19. Biomed J 43(5): 399-413.
- Eskens BJ, Zuurbier CJ, Van Haare J, Vink H, Van Teeffelen JW, et al. (2013) Effects of two weeks of metformin treatment on whole-body glycocalyx barrier properties in db/db mice. Cardiovasc Diabetol 12: 175.
- Targosz Korecka M, Malek Zietek KE, Kloska D, Rajfur Z, Stepien E, et al. (2020) Metformin attenuates adhesion between cancer and endothelial cells in chronic hyperglycemia by recovery of the endothelial glycocalyx barrier. Biochim Biophys Acta Gen Subj 1864(4): 129533.
- Al Benna S (2020) Association of high level gene expression of ACE2 in adipose tissue with mortality of COVID-19 infection in obese patients. Obes Med 19: 100283.
- Al Salameh A, Bennis Y, Cariou B, Lalau JD (2021) The association between metformin treatment and COVID-19 outcomes according to metformin continuation during hospitalisation. Diabetes Metab 47(6): 101297.
- Bramante CT, Ingraham NE, Murray TA, Marmor S, Hovertsen S, et al. (2021) Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis. Lancet Healthy longev 2(1): e34-e41.
- Ghany R, Palacio A, Dawkins E, Chen G, Mc Carter D, et al. (2021) Metformin is associated with lower hospitalizations, mortality and severe coronavirus infection among elderly medicare minority patients in 8 states in USA. Diabetes metab syndr 15(2): 513-518.
- Jiang N, Chen Z, Liu L, Yin X, Yang H, et al. (2021) Association of metformin with mortality or ARDS in patients with COVID-19 and type 2 diabetes: A retrospective cohort study. Diabetes Res Clin Pract 173: 108619.
- Khunti K, Knighton P, Zaccardi F, Bakhai C, Barron E, et al. (2021) Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England. Lancet Diabetes Endocrinol 9(5): 293-303.
- Korkusuz R, Karandere F, Okay F, Koçoğlu H (2021) Metformin significantly lowers the mortality rate in diabetic COVID-19 patients.
- Lally MA, Tsoukas P, Halladay CW, O Neill E, Gravenstein S, et al. (2021) Metformin is Associated with Decreased 30-Day Mortality Among Nursing Home Residents Infected with SARS-CoV2. J Am Med Dir Assoc 22(1): 193-198.
- Li J, Wei Q, Mc Cowen KC, Xiong W, Liu J, et al. (2022) Inpatient use of metformin and acarbose is associated with reduced mortality of COVID-19 patients with type 2 diabetes mellitus. Endocrinol Diabetes Metab 5(1): e00301.
- Ma Z, Patel N, Vemparala P, Krishnamurthy MJm (2022) Metformin Is Associated with Favorable Outcomes in Patients with COVID-19 and Type 2 Diabetes Mellitus. Sci Rep 12(1): 5553.
- Ong AN, Tan CC, Cañete MT, Lim BA, Robles J (2021) Association Between Metformin Use and Mortality among Patients with Type 2 Diabetes Mellitus Hospitalized for COVID19 Infection. J ASEAN Fed Endocr Soc 36(2): 133-141.
- Saygili ES, Karakiliç E, Mert E, Şener A, Mirci A (2021) Preadmission usage of metformin and mortality in COVID-19 patients including the post-discharge period. Ir J Med Sci: 1-7.
- Tamura RE, Said SM, De Freitas LM, Rubio IGS (2021) Outcome and death risk of diabetes patients with Covid-19 receiving pre-hospital and in-hospital metformin therapies. Diabetol Metab Syndr 13(1): 76.
- Wargny M, Potier L, Gourdy P, Pichelin M, Amadou C, et al. (2021) Predictors of hospital discharge and mortality in patients with diabetes and COVID-19: updated results from the nationwide CORONADO study. Diabetologia 64(4): 778-794.
- Oh TK, Song IA (2021) Metformin use and risk of COVID-19 among patients with type II diabetes mellitus: an NHIS-COVID-19 database cohort study. Acta diabetol 58(6): 771-778.
- Pérez Belmonte LM, Torres Peña JD, López Carmona MD, Ayala Gutiérrez MM, Fuentes Jiménez F, et al. (2020) Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucose-lowering drugs: a nationwide cohort study. BMC Med 18(1): 359.
- Chen Y, Yang D, Cheng B, Chen J, Peng A, et al. (2020) Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With GlucoseLowering Medication. Diabetes care 43(7): 1399-1407.
- Hariyanto TI, Kurniawan A (2020) Metformin use is associated with reduced mortality rate from coronavirus disease 2019 (COVID-19) infection. Obes Med 19: 100290.
- Yang W, Sun X, Zhang J, Zhang K (2021) The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus. Diabetes Res Clin Pract 178: 108977.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, et al. (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372: n71.
- Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11): 1539-1558.
- Barili F, Parolari A, Kappetein PA, Freemantle N (2018) Statistical Primer: heterogeneity, random- or fixed-effects model analyses?. Interact Cardiovasc Thorac Surg 27(3): 317-321.
- Crouse A, Grimes T, Li P, Might M, Ovalle F, et al. (2020) Metformin Use is Associated with Reduced Mortality in A Diverse Population with Covid-19 and Diabetes. medRxiv.
- Goodall JW, Reed TAN, Ardissino M, Bassett P, Whittington AM, et al. (2020) Risk factors for severe disease in patients admitted with COVID-19 to a hospital in London, England: a retrospective cohort study. Epidemiol Infect 148: e251.
- Lalau JD, Al Salameh A, Hadjadj S, Goronflot T, Wiernsperger N, et al. (2021) Metformin use is associated with a reduced risk of mortality in patients with diabetes hospitalised for COVID-19. Diabetes Metab 47(5): 101216.
- Li J, Wei Q, Li WX, Mc Cowen KC, Xiong W, et al. (2020) Metformin Use in Diabetes Prior to Hospitalization: Effects on Mortality in Covid-19. Endocr pract 26(10): 1166-1172.
- Luo P, Qiu L, Liu Y, Liu XL, Zheng JL, et al. (2020) Metformin Treatment Was Associated with Decreased Mortality in COVID-19 Patients with Diabetes in a Retrospective Analysis. Am J Trop Med Hyg 103(1): 69-72.
- Cheng X, Liu YM, Li H, Zhang X, Lei F, et al. (2020) Metformin Is Associated with Higher Incidence of Acidosis, but Not Mortality, in Individuals with COVID-19 and Preexisting Type 2 Diabetes. Cell Metab 32(4): 537-547.e3.
- Kim MK, Jeon JH, Kim SW, Moon JS, Cho NH, et al. (2020) The Clinical Characteristics and Outcomes of Patients with Moderate-to-Severe Coronavirus Disease 2019 Infection and Diabetes in Daegu, South Korea. Diabetes Metab J 44(4): 602-613.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.