Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Telehealth and It’s Application in Pandemic
*Corresponding author: Yong Li, Department of Orthopedic Surgery, Biomedical Engineering at Western Michigan University Homer Stryker MD School of Medicine, Kalamazoo, MI, USA.
Received: April 19, 2023; Published: May 23, 2023
DOI: 10.34297/AJBSR.2023.18.002530
Abstract
Telehealth is an innovative method to provide medical care to patients through the utilization of digital services. The process of medical information exchange between clinical doctors or clinicians and patients can be done digitally, such as video, phone, and online patient portals. Telehealth can be beneficial to large patients in several fields of medicine and increase healthcare equity and palliative treatment. During the pandemic, the utilization of telehealth increased substantially and efforts were made to ensure healthcare was effectively provided to patients. Access to healthcare increased significantly as telehealth allowed patients to overcome obstacles such as transportation, distance, scheduling availabilities, and with the pandemic, close contact. Although use has risen over the past few years, various aspects of telehealth need to be further evaluated to determine its continual use beyond the pandemic.
Keywords: Telemedicine, Telehealth, Pandemic, Digital service, Healthcare, Clinic, COVID-19
Introduction
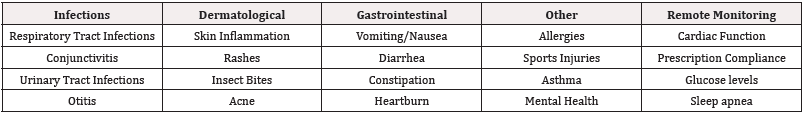
Telehealth is the utilization of digital services when providing healthcare. The exchange of medical information between clinicians and between clinical and patients can be done via video, phone, and online patient portals. It can be synchronous, where the patient and provider communicate in real-time via a phone or video call, but can also be asynchronous, allowing the provider to view patient data, images, and messages outside of scheduled appoint ments and quickly respond to any questions or concerns patients may have without having to setup a meeting. This allows patients to get the necessary clinical aid without the barriers that may prevent this in their everyday life, such as transportation, time off from work, or familial responsibilities. The original intent of telehealth was to close the medical gap within rural & underserved communities [1]. It has now grown to be an essential aspect of healthcare with increased accessibility for all patients (Table 1).
Specialties that have been primarily in-person have given patients the opportunity to use telehealth, further increasing access. Psychiatry and therapy have become more accessible to individuals with the use of telehealth. Between 2010 to 2017, there was an increase in overall telehealth visits amongst rural communities contributing to the 425% increase of mental health appointments [2]. This increases the ability for patients that have undiagnosed conditions to receive treatment as individuals can attend their session from the comfort of their own homes, decreasing the nerves and anxiety that can stem from an initial psychiatry or therapy visit. Patients that have diagnosed conditions can have their follow up sessions over telehealth, which ensures their provider can monitor their mental health progress.
Telehealth has also incorporated at-home monitoring systems. This includes glucose and blood pressure monitors that can be an indication for patients if their values are abnormal [3]. With these devices, patients can record their values and report to their healthcare provider to analyze the trends within their health. With continuous results outside of patients’ normal range, modifications can be done to ensure patients’ condition do not progress dangerously. This is also advantageous for patients are starting a new medication to control their glucose or hypertension as it can aid in determining if that medication is effective.
Telehealth is also a source of communication between medical facilities and providers to ensure continuity of care for patients. A study was done where a multi-disciplinary team was created with advanced practice nurses skilled in wound care and faculty at long term care facilities. The nurses informed faculty members about proper prevention and treatment of pressure ulcers, as well as providing access through telehealth for continual aid [4]. With telehealth, the number of visits to the clinic or the emergency department due to wounds can decrease. Not only is this time and cost effective for patients, but it can also decrease the number of nosocomial infections that patients could be exposed to.
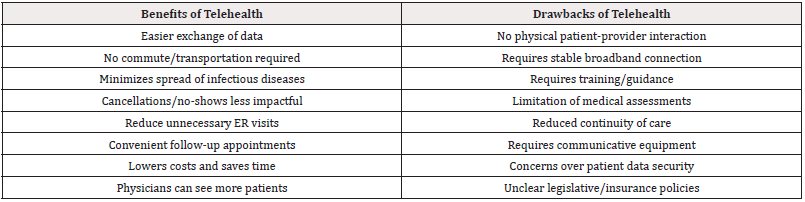
There are many advantages to telehealth that benefit both the patient and the provider. For example, a patient that has difficulty traveling (either due to a lack of reliable transportation/pre-existing medical condition) or is located far away from a healthcare facility can utilize telehealth to meet with a healthcare provider from the comfort of their own home. This accessibility of telehealth expands scheduling options and allows for more convenient appointment- timeslots for the patient. This applies to follow-up appointments as well, as it is much easier to schedule a brief meeting that does not require any commuting than a meeting that might require the patient taking a day off work to be able to attend.
Another advantage of telehealth is that providers can view and share patient data more efficiently amongst themselves, which ultimately improves patient care. The incorporation of the patient’s medical history into an intuitive online database can shorten wait times for the patient when it comes to receiving referrals and treatment, as collaboration between the patient’s different healthcare teams is streamlined. Finally, telehealth reduces the spread of infection. If a patient is mildly sick and does not require immediate medical attention, a virtual visit can reduce their chance of spreading disease. A contagious patient cannot spread their illness to others if the patient remains isolated at home, whereas someone leaving their home to travel to a healthcare facility very well can.
With all its advantages, telehealth also has some shortcomings that must be taken into consideration. Perhaps the biggest disadvantage for telehealth is the lack of physical interaction between the patient and provider. It is not possible for the provider to do a physical assessment of the patient when they are separated by a screen. While the provider can do a limited visual inspection of the patient, a low quality of video (or lack of video-capable technology) would make even that difficult, potentially allowing for misinterpretation/ underestimation of the patient’s condition. Another disadvantage is that telehealth requires a minimum threshold of broadband and technology from the patient. Certain populations, such as older adults, racial/ethnic minorities, and those with lower socio-economic statuses have higher rates of reduced access to those technologies [5].
The Essentials of Telehealth in The Pandemic
Telehealth quickly became a central element to patient healthcare with the emergence of the COVID-19 pandemic. According to a report from the US Department of Health and Human services, from 2019 to 2020, a 63-fold increase was seen in Medicare visits conducted through Telehealth services. In 2019, a total of 840,000 individuals attended their visits through Telehealth mediums, and this number jumped to 52.7 million in 2020 [6] Evidently, this shows that the pandemic resulted in a bolstered use of Telehealth services across the country. Moreover, it can be said that because of the pandemic, Telehealth services previously being used by providers and patients were significantly improved upon- both out of ingenuity being born from a challenging worldwide environment, and out of necessity for those patients who were absolutely unable to attend appointments in person for a host of reasons.
In an analysis done by McKinsey & Company, it was noted that investments in digital health and virtual care has increased dramatically in the last few years [7] Specifically, as compared to investments in 2017, in 2020 a 3X increase was seen in venture capitalist investment in digital health technologies [7] According to Rock Health’s H1 Digital Health Funding Report for 2021, the total venture capital investment for digital health services in the first half of 2021 was $14.7 billion, compared to that of 2020 ($14.6 billion) and 2019 ($7.7 billion).7 This clearly demonstrates that investments are being made in the realm of Telehealth and digital medicine following the emergence of the pandemic, as individuals have come to understand the value of virtual medical care. These investments will surely pave the way for ingenuity in this realm, leading to an improvement of current virtual care, and a positive outlook for the future of digital medicine.
In fact, studies have shown that following COVID-19’s impact on the health system, significant changes were implemented in the realm of digital health that increased accessibility and functionality of these services. It was noted that improvements in broadband infrastructure and internet access and connectivity have increased to facilitate the usage of virtual care technologies [8] An enhanced availability and provision of information and communication technologies was also seen- including electronic communication using technological devices, video conferencing, phone calls, and digital monitoring.8 Video conferencing especially, according to Mc Growder et. al, was shown to be increasingly on the rise for use, as it allows for efficient and reliable communication in real-time between the patient and their provider [8] Having an interface in which patients and providers are able to see one another significantly adds to the patient experience and allows for better care to be delivered.
Patient satisfaction with telehealth services was shown to actually increase following the pandemic, studies have shown. Ramaswamy et al. performed a retrospective cohort analysis of a New York hospital, in which 620 virtual visits and 37,989 in-person visits were compared for patient satisfaction.9 This was divided into pre-COVID and during-COVID groups for analysis. The hospital saw an 8729% increase in video visits in the during-COVID group compared to the pre-COVID group, and also noted that Press Ganey patient satisfaction survey scores were significantly higher for video visits compared to in-person visits [9] After adjusting for other factors, it was also seen that patient satisfaction was higher for both video visits, as well as during the during-COVID group [9] This study emphasizes the notion that virtual healthcare has found its place in the healthcare system, and that many patients in fact view it as equal, if not better than in-person visits. Furthermore, in a systematic review of 36 studies performed by Mc Growder et al. [8] it was found that “... a high level of contentment with telehealth across dimensions such as consumer focus, information sharing, system experience and overall satisfaction [8] The researchers indicated that patients residing in remote areas were mostly satisfied with telehealth services due to increased access to health care while decreasing possible inconvenience of travelling to a medical facility [8].
This highlights how technological advancements in the realm of healthcare are improving accessibility and ease of care, which will certainly pave the way for digital medicine to become a crucial factor in the general healthcare landscape. Increased accessibility for those in remote areas, for immunocompromised patients, and more, was an extremely significant benefit that came along with the advancement of digital health technologies. Being that patient satisfaction is as high as it is, this signifies that COVID-19 immensely impacted the healthcare landscape and that virtual healthcare services will continue to emerge and advance to support the current modes of healthcare that have been in use. High patient satisfaction signifies that telehealth models that were put in place and bolstered with the emergence of the pandemic were successful, and that they do in fact have a place in the future of healthcare. COVID-19 changed the landscape for healthcare, but the emergence of telehealth and the increase in its use has evidently left patients feeling satisfied and that they are still receiving adequate and useful care.
The field of telehealth has proliferated since the start of the COVID-19 pandemic, allowing providers to treat their patients without unnecessary exposure to the coronavirus. Yet, as the pandemic has calmed, the growth and pervasiveness of telehealth’s presence within modern medicine is here to stay. Improvements in technology have improved experiences for both patients and providers encouraging more usage and implementation of telehealth in their medical experiences. In addition, the further interconnected health information technology becomes the more seamless the experience will be. However, with the transition of medical delivery, attitudes and trust must change for full acceptance of telehealth. Public opinion and regulations can create changes within each other, telehealth friendly regulations may signal to patients that telehealth is a new pillar in our medical structure. Lastly, as technology improves and is applied to telehealth novel use cases will be implemented.
Looking Beyond the Pandemic
In telehealth the clinical application and outcomes are principally considered, however almost equally important is the execution of the technology. Both for doctors hoping to introduce telehealth into their practice and for patients wishing to get their healthcare virtually. Technological literacy and cost of devices provide barriers to the implementation of telehealth. As the cost of more powerful computers, cell phones, and internet connections decreases and baseline technological literacy increases within different age groups, this challenge to telehealth will only decline [6] From a provider’s perspective, improvements in technology will allow greater efficiency and confidence in obtaining objective findings from patients, potentially increasing the scope of telehealth implementation. Furthermore, more powerful programs will cross communicate with other platforms within telehealth ranging from fitness trackers, genomic data, sleep trackers, and palliative care monitors to improve care [7,8]. As technology improves, it will become less of a forethought for patients and doctors in the delivery of telehealth.
Emerging and Future Technologies
An increasing demand for telehealth services has placed pressure on telehealth technologies to provide solutions for modern healthcare. New improvements and development in software allow mobile applications to track specific disease progression and connect patients with providers. Virtual and augmented reality may provide benefits in telehealth, improving patient education and communication. In addition, wearable technology like smartwatches can measure vitals, location, sleeping, eating, and medication/ treatment adherence. For example, wearable technology has been described in treatment and tracking of asthma and COPD, where flair ups can be multifactorial in etiology. The data provided by wearable technology can connect symptoms to triggers like pollution, allergens, or missed medication doses, allowing for trigger avoidance and improved treatments [9]. Furthermore, on the cutting edge of medical technology there is the utilization of telerobotics, where a surgeon and their patient can be in separate locations, allowing procedural specialties to have an opportunity to practice telehealth. Developing these tools and new technologies will improve the practice and experience of telehealth in the future.
Attitudes
As telehealth transitions from a novelty to potentially a normal facet medical care, its use will become more pervasive healthcare option. This shift comes from positive experiences and successful implementation by patients and providers. The multiple strengths of telehealth, discussed above, can provide these satisfactory interactions. However, telehealth must overcome public concerns of privacy and appropriate medical care. Both of these anxieties are found within normal medical delivery and will be increasingly scrutinized in telehealth. As personal privacy has become a higher priority in the internet age, patients may be privy to discuss their intimate health details over a telehealth model. In addition, patients will be hesitant to commit to telehealth if they must compromise the quality they receive [10,11].
Regulations
Much of the behavior in medicine is influenced by healthcare reimbursement, especially by Medicare and Medicaid due to their considerable size. As a result of their power, health insurance groups can influence norms within healthcare, consequentially impacting cultural attitudes and expectations [12,13]. Similarly, malpractice liability applies pressure by causing defensive medicine or usage of less conservative options, defeating the cost savings of telehealth [14]. Especially pertinent to telehealth, is the unique challenge of collecting objective information, including vitals, labs, imaging, and physical exam findings. This limitation is why telehealth is most useful to certain specialties. Appropriate malpractice regulations are therefore necessary to protect patients, while also allowing providers to practice sensible healthcare through telehealth. Lastly, telehealth friendly geographical regulations will remove a barrier for doctors attempting to treat underserved populations outside their region. Regulators must understand the benefits and drawbacks of telehealth and create sensible regulations to foster this field’s growth [15].
Summary
Medicine is constantly evolving with the intention of providing the upmost care to patients. Telehealth has been a significant component in advancing this purpose, especially during the pandemic where healthcare was needed the most. Although telehealth has provided significant benefits to patient care and has progressed tremendously in recent years, there are still hindrances that need to be addressed for telehealth to reach its maximal effectiveness for patients (Table 2).
The future of telehealth will hopefully prove to contribute to the three aims of healthcare improvement: improving the experience of care, improving the health of populations, and reducing per capita costs of health care [16,17].
Conflicts of Interests
Dr. Li is one of the executive editors for the Journal of Cellular Biochemistry (JCB). All other authors declare no COI or otherwise.
Acknowledgements
The article prepared is partially supported by the Homer Stryker MD School of Medicine.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.