Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Challenges Impacting Clinical Placement Quality: Insights From Nursing Undergraduates in Sri Lanka - A Mixed Methods Study
*Corresponding author: Rasika Perera, Department of Biochemistry, Faculty of Medical Sciences, University of Sri Jayewardenepura, Sri Lanka.
Received: June 23, 2023; Published: June 28, 2023
DOI: 10.34297/AJBSR.2023.19.002571
Abstract
Introduction: Clinical experience plays a crucial role in nursing education programs, enhancing the clinical competence of nursing undergraduates. The research aimed to understand how nursing undergraduates perceive their clinical experiences and gather insights on the topic, as this area lacks research evidence.
Methodology: The study used a mixed method, including a descriptive quantitative design with qualitative inputs (n=78) and Focus Group Discussions (FGDs) (n=42). The sample consisted of nursing undergraduates in their 2nd, 3rd, and 4th years at the University of Sri Jayewardenepura. Self-administered questionnaires with open-ended questions and focus group discussions were employed for data collection.
Results: A total of 78 participants completed the self-administered questionnaire. Most participants were females (79.5%), and 4th-year students represented 46.2% of the sample. The quantitative analysis of the data showed that most participants agreed that clinical appointments were sufficient to enhance their knowledge and skills. However, they expressed dissatisfaction with aspects such as the availability of equipment, facilities in hospitals and universities for clinical practice, and guidance from hospital nursing staff. On the other hand, participants found the clinical supervision guidance provided by academic staff from the university to be adequate. Participants also reported positive experiences in clinical placements at certain hospitals, with Paksha Hospital being the best. Issues highlighted include transportation problems, lack of sufficient room and meal facilities, and the need for clearer objectives and procedure books for clinical placements. Participants also recommended improving facilities in changing rooms, assigning a graduate nurse or clinical instructor for support, and tailoring assessments to each placement. A descriptive qualitative study was conducted with an exploratory design and an inductive approach. Five FGDs (n= 42) were conducted until data saturation using a focus group guide, a trained note taker and a moderator. The qualitative analysis from the focus group discussions revealed four themes: inadequate resources, negative attitudes toward nursing undergraduates, motivations with support, and suggestions for improvement. It was observed that physical and human resources need to be improved, attitudes toward nursing undergraduates should be more positive, and staff nurses should be more aware and supportive of clinical placements.
Conclusions and Recommendations: In conclusion, the study suggests that enhancing nursing undergraduates’ clinical experience requires addressing resource inadequacies, fostering positive attitudes, and improving support and supervision. Recommendations include providing adequate physical and human resources, raising awareness among staff nurses, and developing strategies to enhance undergraduate clinical competencies in Sri Lanka.
Introduction
Nursing education institutions worldwide are actively searching for improved methods to adequately prepare future nurses, with particular focus on the significance of clinical education. Developing nurses’ clinical competence ensures safe and effective patient care [1]; Gaber son & Oermann, 2007). While there is a consensus on the importance of clinical competencies in nursing for safe and effective patient care, there is a lack of a universally accepted definition for this concept. Different regulatory bodies have made efforts to define the notion of “clinical competence” [2]; Nursing and Midwifery Board of Australia, 2006; Nursing & Midwifery Council, 2010) [3]. Clinical competence in nursing is commonly defined as the effective integration of cognitive, affective, and psychomotor skills during the delivery of nursing care. This definition draws from Bloom’s taxonomy for educational goals [4]. By the end of their undergraduate studies, nursing students are expected to attain a high level of clinical competence through adequate theoretical knowledge and practical training. Assessing clinical competence is crucial to ensure that practicing nurses provide safe and effective care [5].
Regarding nursing education, clinical settings, and classrooms are different learning environments for nursing students [6]. In terms of a clinical setting, a descriptive correlation study conducted among 162 nursing students by Hakim Zadeh, et al. [7]. found a 0.449 correlation coefficient of the clinical learning environment and clinical competence. It shows that students, who consider the clinical environment a suitable learning place, evaluated their clinical competence at a higher level. Further, the clinical environment atmosphere, behaviors of nurses and staff of the hospital, equipment and facilities needed for education and treatment, and clinical teaching methods all affect acquiring clinical competence [7].
The quality of the clinical learning environment is a crucial factor in shaping the clinical experience of nursing students. Its effectiveness largely depends on establishing a positive and supportive atmosphere within the hospital setting. An exploratory study involving 232 Italian nursing students found that all participants perceived their clinical learning environment as satisfactory [8]. Specifically, 3rd year nursing students expressed high levels of satisfaction with the activities conducted in the ward, while 2nd year students reported lower satisfaction levels. However, all participants agreed that practical work experience was valuable and not a waste of time. The researchers recommended that selecting clinical placements for students should prioritize creating a more suitable clinical learning environment that fosters professional development and ensures a facilitating atmosphere, resulting in a positive and enriching experience [8].
A descriptive qualitative study conducted involving 16 final-year nursing students in Ghana, utilizing a semi-structured interview guide [9]. highlighted several significant factors that contributed to clinical learning, including being exposed to new knowledge, receiving supervision, and having the opportunity for autonomy. Participants also emphasized their clinical experiences [10]. provided valuable learning opportunities that contributed to developing clinical competence. On the other hand, the students identified various challenges in the clinical environment, such as negative staff attitudes, insufficient equipment, unfavorable student attitudes, limited learning opportunities, and a shortage of clinical supervisors. Based on the study’s findings, the researchers recommended that deliberate efforts should be made to actively teach, supervise, and encourage students to exercise independence in the clinical setting, thereby enhancing clinical teaching and learning. They emphasized the need for collaboration among nursing educational institutions and other stakeholders to address and overcome students’ challenges in the clinical environment Ammo, et al. (2022).
Nabulsi, et al. [11] characterized various elements within the clinical setting, including the ward, staff, patients, facilities, and clinical nurse educators, as valuable resources. According to Corlett [12], key factors for effective clinical learning encompass staying updated with knowledge, possessing patience and self-confidence, demonstrating commitment, having clinical skills, fostering self-determination, and allowing students to engage in practical tasks while applying appropriate clinical knowledge. Furthermore, Nabulsi, et al. (2012) highlighted the essential role of teachers in student learning, as they serve as role models to guide students’ integration into the nursing profession.
In a case study, Lewis [13] studied educational barriers and factors affecting nursing education through nursing students’ experiences. Results showed that nursing students described such factors as motivation, a supportive environment for learning, teaching methods, curriculum design, and previous academic success and learning abilities as facilitators of learning. Barriers to learning were also similar: an unsupportive environment for learning, teaching methods, curriculum design, learning abilities and stress. On the other hand, a student’s perception of the clinical learning environment and his/her experiences can affect clinical competencies. The clinical learning environment, including opportunities and challenges of clinical learning, has been inserted in the research as a factor affecting clinical competencies. Furthermore, Chuan and Barnett [14]. conducted an exploratory study in a private hospital in Penang, Malaysia, to describe and compare the perceptions of the Clinical Learning Environment (CLE) among 142 student nurses, 54 staff nurses, and 8 nurse tutors. The study aimed to identify factors that either facilitated or impeded student learning. Data were collected through a structured, self-administered questionnaire comprising six pre-determined subscales. The overall perception of the CLE was positive among the participants. Notably, both students and their tutors regarded ‘supervision by clinical instructors’ as the most positive aspect of the CLE.
The researchers concluded that factors contributing to enhanced student learning included the attitudes of students and staff nurses toward student learning, a diverse range of clinical opportunities, availability of sufficient equipment, and adequate time allocated for performing procedures. Conversely, factors that hindered student learning included excessive students in the clinical unit, busy wards, and students being treated as mere workers [14]. In a study conducted in Botswana, Rajeswari (2017) found that nursing students face challenges in applying theory to practice due to inadequate supervision in the clinical setting, leading to negative impacts on their healthcare practices. Similarly, Phinehas, Mulenga, and Amad hila (2017) reported that the attitudes of teaching assistants affect the productivity of nursing students in the clinical setting. A positive and supportive learning environment is crucial for students, as it fosters their growth and development. Constructive feedback plays a vital role in advancing clinical practice, while negativity hinders efficient clinical performance. Furthermore, insufficient hands-on experience opportunities in teaching hospitals, a shortage of clinical instructors and nurse educators, and an overwhelming number of students enrolled in the program can all adversely affect students’ success in clinical practice [15].
In Sri Lanka, nursing education encompasses theoretical instruction in the classroom and practical training in the clinical setting. This comprehensive approach aims to equip nursing undergraduates with the necessary skills and knowledge to deliver effective and efficient care to their clients. Presently, pre-registration nursing education in Sri Lanka comprises a four-year Bachelor of Science in Nursing degree offered at state universities and a three-year diploma program conducted in government schools of nursing (Jayasekara & Amaras kara, 2015). Currently, sixteen Schools of Nursing (formerly named Nursing Training Schools / NTS), which are under the Ministry of Health, provide a three-year diploma in Nursing, and seven universities under the Ministry of Higher Education provide four-year -B.Sc. nursing degree honors programs. Upgrading the three years of the Diploma in Nursing program to the degree level was proposed in the National Health Policy of 1992 and the National Strategic Plan for Nursing and Midwifery Development 2001-2010 (Jayasekara & Amaras kara, 2015) [16,17]. The Open University of Sri Lanka also offers a BSc Nursing degree program as a Post Registered Nurse (Post RN) degree program. This program provides an opportunity for registered nurses working in the field to further their education and obtain their BSc Nursing degree.
Recently private universities in Sri Lanka have also introduced BSc Nursing degree for nurses working in State and Private hospitals. Some of these private universities are conducting diploma courses for direct entry students, and they can upgrade their diploma to a degree level from the institutions/ universities in the affiliated countries. Recently some state and private universities in Sri Lanka have also introduced master’s degrees in nursing for individuals who have completed their BSc in nursing. Especially, Sri Lankan nursing scholars who have recently obtained PhDs are making valuable contributions to advancing nursing education in the country. However, as Kumar and Sousing [18]. mentioned in their review, the existing nursing curriculum in Sri Lanka has less emphasis on research, evidence-based practice, therapeutic communication skills, exposure to advanced technology, and computer literacy skills.
The current study was conducted in the BSc nursing program at the University of Sri Jayewardenepura (USJ). It is a four-year full-time program with 12 terms, 3 terms per year. The first clinical placement for the first-year students starts in the 9th week of the first year when nursing undergraduates are supposed to have acquired basic nursing procedures skills according to their fundamentals of nursing practical subject and other professional knowledge. Clinical practice appointments are done as a rotation throughout the 4-years, designed to cover all specialties in nursing such as medical/surgical nursing, pediatric nursing, gynecological and obstetric nursing, psychiatric and mental health nursing. In order to get specialized training, these students are allocated to some special clinical areas like Accident and trauma care, Central Sterilization Supplying Department (CSSD), Blood bank, Operation Theaters, Anti Rabies unit, Outpatient Departments (OPD), Intensive Care Units (ICU), Neonatal Intensive Care Unit (NICU), labor room, Cardiology Unit, Endoscopy unit, Ear Nose Throat (ENT) and Eye wards. The Colombo South Teaching Hospital (CSTH) is the main and affiliated teaching hospital for the university. In addition, nursing undergraduates are given clinical placements at Sri Jayewardenepura General Hospital (SJGH) (for CSSD, Cardiology, NICU, ENT and Eye wards), National Hospital Sri Lanka (NHSL) (for Accident and Trauma care), Paksha Hospital (for cancer care) and National Institute of Mental Health (NIMH) (for psychiatric care) as specialized training. Additionally, these nursing undergraduates have community placements to improve their community nursing care and family health nursing care. Nursing undergraduates at the BSc nursing program/ USJ are taught mainly by the nursing academics and demonstrators from the Department of Nursing and Midwifery (former nursing unit), academics from the Faculty of Medical Sciences, nurses and other healthcare professionals from the clinical settings. The BSc Nursing program at the USJ holds the distinction of being Sri Lanka’s first preregistration nursing degree program. Despite its seventeen years of existence, research has not examined nursing undergraduates’ perceptions of their clinical training. Therefore, this study explored nursing undergraduates’ perspectives regarding their clinical competencies.
Method
Objectives
To explore perspectives towards clinical competencies and factors affecting clinical competencies as perceived by nursing undergraduates at the USJ, Sri Lanka.
Data Collection Methods and Instruments
The study used a mixed method, including a descriptive quantitative design with qualitative inputs (n=78) and focus group discussions (n=42). The sample consisted of nursing undergraduates in their 2nd, 3rd, and 4th years at the University of Sri Jayewardenepura. Self-administered questionnaires with open-ended questions and focus group discussions were employed for data collection. To explore the factors related to clinical competencies perceived by nursing undergraduates’ researchers developed a focus group guideline based on the intensive and extensive literature survey. A trained moderator who is not an academic member of the nursing program moderated the focus groups, and discussions were tape-recorded.
Quantitative Findings
Seventy-seven participants completed the self-administered questionnaire, and descriptive statistics were employed for data analysis. The demographic profile of the participants revealed that the majority were in their 4th year of study (46.2%), with a significant proportion being female (79.5%). The largest age group represented was between 20-24 years old, comprising 41% of the participants. Moreover, most participants identified as Sinhalese (94%). Financial support or Mahipala from the university was received by 49% of the participants.
Most participants (72%) agreed that clinical appointments are sufficient to enhance subject matters and to gain necessary clinical skills. However, most of the participants disagreed with the adequacy of equipment available in hospitals for clinical practice (48%), facilities provided by the hospitals for clinical learning (44%), facilities provided by the university for clinical practice (50%), and guidance from Hospital nursing staff for clinical practice (60%). Furthermore, most participants (53%) agreed that the clinical supervision guidance provided by the university’s academic staff is adequate.
Regarding the facilities (including transport to hospitals and facilities for taking breakfast and lunch at the clinical placement), all participants mentioned that transport facilities, changing room facilities, and places for taking their breakfast are not enough. The absence of transportation to the hospitals is a significant challenge, causing difficulties in attending clinical placements on time due to traffic and resulting in tiredness and exhaustion. Another common concern of all the participants was the lack of adequate space and facilities for having their breakfast and lunch. They emphasized the need for appropriate facilities to be provided to motivate them in their profession.
Most participants noted that the time allocated for clinical sessions is acceptable, allowing for clinical experience and nursing practice expertise. About the importance of maintaining a clinical record book, most of the participants mentioned that maintaining a clinical record book is good, but it is not always practical to do so consistently. The main problem encountered during clinical visits is filling out the record book and difficulty in getting signatures for every procedure as they are performed. Most students believe that clear objectives and procedure books for clinical placements are crucial. They also believe that assessments should be tailored to each placement to ensure appropriate evaluation, a graduate nurse or clinical instructor should be assigned to each unit to support and guide students during the clinical placements. In addition to these common recommendations, each batch made the following unique recommendations: The fourth-year nursing students noted that the heavy workload caused some students to experience depression and the necessity for medical treatment and that further steps needed to be taken to offer the students psychological support. The third-year nursing undergraduates suggested that it is better to inform the students regarding the number of clinical hours needed for each appointment, and it is preferable to have clinical instructors in each hospital as nurses frequently do not have enough time to teach them. The second-year nursing students argue that it would be preferable to give the nursing staff at each hospital specific instructions regarding the goals of the clinical placements for nursing undergraduates. Additionally, they advise against organizing clinical placements on weekends and public holidays.
Qualitative Findings
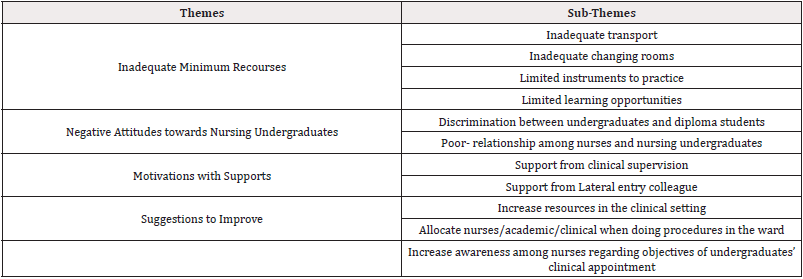
Qualitative data were analyzed using content analysis described by Granholm and Landman [19]. Transcripts were read numerous times to comprehend and establish basic meaning categories and codes. After familiarizing yourself with the data, the initial codes were created. The transcripts were generated codes, subcategories, categories, and themes. Subcategories and categories were created by labeling combinations of relevant beginning codes. Finally, until the researchers reached an agreement on the text’s underlying meaning and primary themes, the text’s latent meaning and primary themes were developed. Final themes were determined after constant comparisons of codes and themes (Table 1).
Data saturation was achieved through five Focus Group Discussions (FGDs) involving a total of 42 participants, leading to the identification of four thematic perspectives on clinical experience:
a) Inadequate minimum resources,
b) Negative attitudes toward nursing undergraduates,
c) Motivations with support, and
d) Suggestions for improvement
Discussion
Clinical experience plays a crucial role in nursing education programs, serving as a fundamental component for developing competent nursing practitioners. It provides students with real- world exposure, practical skills, and critical thinking abilities necessary for delivering high-quality patient care [20]. In the quantitative study, the self-administered questionnaire was completed by a total of 78 participants, and descriptive statistics were employed to analyze the collected data. The participants’ demographic profiles yielded several significant insights. Notably, a substantial proportion of the participants (46.2%) were in their 4th year of study, indicating a higher level of exposure to clinical settings and a better grasp of clinical competencies. Moreover, most participants (79.5%) were female, reflecting the gender distribution among nursing undergraduates. Additionally, the largest age group represented was 20-24 years (41%), indicating a predominantly young adult population pursuing nursing education. In Sri Lanka, the nursing degree program typically admits students immediately after they complete their A/L (Advanced Level) examinations, which is usually undertaken by students in their late teens or early twenties. Therefore, a predominantly young adult population is expected to pursue nursing education. Financial support was also found to be a significant factor, as most participants (49%) reported receiving financial assistance or Mahipala from the university, underscoring its importance for nursing undergraduates in Sri Lanka. This differs from other countries where individuals may enter nursing at any age and have different financial arrangements.
Regarding their perceptions of clinical experiences, most participants (72%) agreed that clinical appointments were sufficient for enhancing subject matter knowledge and acquiring the necessary clinical skills. However, participants expressed dissatisfaction with various aspects of their clinical experiences. They cited limited availability of equipment in hospitals for clinical practice (48%), inadequate facilities provided by hospitals for clinical learning (44%), insufficient facilities provided by the university for clinical practice (50%), and a lack of guidance from hospital nursing staff during clinical practice (60%). Conversely, most participants (53%) agreed that the clinical supervision guidance provided by academic staff from the university was adequate.
To delve further into nursing undergraduates’ perspectives on clinical experiences, a descriptive qualitative study was conducted using an exploratory design and an inductive approach. Participants emphasized the significance of dedicated nurse/academic support during procedures conducted in the ward. They recommended the allocation of experienced nurses, academic staff members, or clinical instructors to guide and supervise nursing students during practical procedures. This suggestion aimed to ensure that students receive real-time guidance, feedback, and support while delivering patient care. Furthermore, participants expressed the need for increased nurse awareness regarding the specific objectives of undergraduate clinical appointments. They suggested the provision of clear information and communication channels to ensure that nurses understand nursing students’ learning goals and expectations during their clinical placements. This suggestion aimed to foster collaboration and mutual understanding between nurses and nursing students, ultimately creating a supportive and conducive learning environment.
These findings shed light on both the positive and negative aspects of nursing undergraduates’ perceptions of their clinical experiences. While participants acknowledge the value of clinical appointments for enhancing their subject knowledge and clinical skills, they also identify significant areas for improvement, particularly in terms of facilities, equipment, and guidance from hospital nursing staff. It is crucial for nursing educators and policymakers to consider these perceptions and address the areas of dissatisfaction raised by nursing undergraduates. By enhancing the availability of resources, improving facilities, and providing better guidance and support during clinical placements, nursing education programs can ensure a more positive and effective learning experience for students, ultimately enhancing their clinical competencies.
Conclusion and Recommendations
This study represents a pioneering contribution to the field as it is the first of its kind to comprehensively explore the perspectives of nursing undergraduates regarding their experiences in clinical learning. This research fills a significant gap in the current body of knowledge by delving into the unique insights and perceptions of nursing undergraduates. Understanding the perspectives of nursing undergraduates is crucial for enhancing the quality and effectiveness of clinical education programs. By shedding light on their experiences, challenges, and suggestions for improvement, this study provides valuable insights that can inform the development and implementation of evidence-based strategies to enhance the clinical learning environment.
In conclusion, the findings of this study highlight the importance of improving undergraduate nursing education in Sri Lanka by enhancing the clinical experience of nursing undergraduates. Several key recommendations can be drawn from the study to address the identified areas for improvement. Firstly, there is a need to ensure that nursing undergraduates have access to adequate physical and human resources during their clinical placements. This includes addressing the limited availability of equipment in hospitals for clinical practice and providing sufficient facilities for clinical learning. By investing in and improving the resources available to nursing undergraduates, their learning experience can be enhanced, allowing them to acquire the necessary skills and knowledge in a supportive environment. Secondly, it is crucial to foster positive attitudes towards nursing undergraduates among the nursing staff. Negative attitudes reported by participants can hinder the learning process and impact the overall clinical experience. Creating awareness among nursing staff about the importance of supporting and mentoring nursing undergraduates can contribute to a more positive and collaborative learning environment.
Furthermore, it is essential to enhance staff nurses’ awareness of undergraduate clinical appointments’ specific objectives and expectations. Clear communication channels and information dissemination can ensure that staff nurses understand the learning goals and requirements of nursing students during their clinical placements. This mutual understanding between staff nurses and nursing undergraduates can foster a supportive and conducive learning environment. Implementing these recommendations will contribute to the improvement of undergraduate nursing education in Sri Lanka. By providing nursing undergraduates with adequate resources, fostering positive attitudes, and enhancing supervision and support during clinical placements, the quality of education and the development of clinical competencies among nursing undergraduates can be significantly enhanced.
It is imperative for nursing educators, policymakers, and healthcare institutions to consider these recommendations and take proactive steps to address the areas of improvement identified in this study. By prioritizing the enhancement of undergraduate nursing education, Sri Lanka can nurture competent and skilled nursing professionals who will contribute to the overall healthcare system’s effectiveness and quality of care.
Acknowledgments
None.
Conflict of Interest
None.
References
- Walker K (2005) Postmodern pedagogy and the nursing curriculum: Collaborating for excellence. Collegian 12(4): 36-40.
- Black J, Allen D, Redfern L, Muzio L, Rushowick B, et al. (2008) Competencies in the context of entry‐level registered nurse practice: a collaborative project in Canada. Int Nurs Rev 55(2): 171-178.
- Nursing and Midwifery Board of Australia. (2006) National competency standards for registered nurses.
- Bloom B (1956) Taxonomy of educational objectives. Handbook-Cognitive domain. New York: David Mckay Company.
- Cook KL, Cox CJ, Henning SE (2008) Breaking the boundaries: Standardization of a competency assessment model for all clinical disciplines. Nurse Leader 6(3): 34-40.
- Brown RA, Crookes PA (2011) Competency assessment using a standardized tool across nursing programs in Australia.
- Hakimzadeh R, Ghodrati A, Karamdost N, Ghodrati H, Mirmosavi J (2013) Factors affecting the teaching-learning in nursing education. GSE Journal of Education 174184.
- Perli S, Anna, Brugnoli A (2009) Italian nursing students’ perception of their clinical learning environment as measured with the CLEI tool. Nur Edu Today 29(8): 886890.
- Amoo SA, Aderoju YBG, Sarfo Walters R, Doe PF, Okantey C, et al. (2022) Nursing Students’ Perception of Clinical Teaching and Learning in Ghana: A Descriptive Qualitative Study. Nurs Res Pract 2022: 7222196.
- Rajeswaran L (2016) Clinical experiences of nursing students at a selected institute of health sciences in Botswana. Health Sci J 10(6): 1.
- Nabolsi M, Zumot A, Wardam L, Abu Moghli F (2012) The experience of Jordanian nursing students in their clinical practice. Procedia Social and Behavioral Sciences 46: 5849-5857.
- Corlett J (2000) The perceptions of nurse teachers, student nurses and preceptors of the theory-practice gap in nurse education. Nurse Educ Today 20(6): 499-505.
- Lewis EJ (2010) How accelerated nursing student learn: a comparative case study of the facilitators, barriers, learning strategies, challenges and obstacles of students in an accelerated nursing program 1986(30): 73-84.
- Chuan OL, Barnett T (2012) Student, tutor and staff nurse perceptions of the clinical learning environment. Nurse Educ Pract 12(4): 192-197.
- Pinehas LN, Mulenga E, Amadhila J (2017) Factors that hinder the academic performance of the nursing students who registered as first years in 2010 at the University of Namibia (UNAM), Oshakati Campus in Oshana, Namibia. JN Edu Prac 7(8): 63.
- Gaberson KB, Oermann MH (2010) Clinical teaching strategies in nursing. Springer publishing company.
- Jayasekara RS, Amarasekara TD (2015) Nursing education in Sri Lanka; challenges and vision for the future. 3rd Annual Worldwide Nursing Conference (WNC 2015).
- Jayasekara RS, Amarasekara TD (2015) Nursing education in Sri Lanka; challenges and vision for the future. 3rd Annual Worldwide Nursing Conference (WNC 2015).
- Graneheim UH, Lundman B (2004) Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 24(2): 105-112.
- Bradshaw C, O Connor M, Butler MP, Fahy A, Tuohy D, et al. (2012) Nursing students' views of clinical competence assessment. Br J Nurs 21(15): 923-927.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.