Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Clinicopathologic Characteristics of Epithelioid Hemangioendothelioma in a Series of 34 Cases: a Double Center Retrospective Study
*Corresponding author: Hongtu Zhang, Department of Pathology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences, and Peking Union Medical College, No. 17 Pan jiayuan South Road, Chaoyang District, Beijing 100021, China, Tel: 0086-10-87787508; Fax: 0086-10-87787515
Received: May 30, 2023; Published: June 16, 2023
DOI: 10.34297/AJBSR.2023.19.002565
Abstract
Objectives: Epithelioid hemangioendothelioma is an exceedingly rare vascular neoplasm with an indolent clinical course in various body sites. Its morphological appearance and prognosis are heterogeneous and complicated.
Methods: We aimed to summarize the clinicopathologic features and prognostic factors of epithelioid hemangioendothelioma in retrospective research of 34 cases in two medical centers.
Results: There were 14 (41.2%) males and 20 (58.8%) females, with a median age of 46.6 years (range 16-75 years). We compared the clinicopathological characteristics of lesions occurring from 7 body sites, including liver (N=15), lung (N=10), skin and soft tissue (N=3), bone (N=2), anterior mediastinum (N=2), adrenal gland (N=1) and left supraclavicular (N=1). In resected lesions, the multi-nodular growth pattern, the endovascular flower-like structure, and the forming of immature blood vessels were remarkable. Immunohistochemistry was essential for accurate diagnosis, especially in a biopsy. ERG and CD31 immunostaining are the most helpful markers. Ki67 index was mostly lower than 10%. Although there were multiple therapeutic options, patients who underwent operation had a better prognosis than unresectable groups in our study.
Conclusions: Epithelioid hemangioendothelioma was clinically indolent, and the prognosis depended mainly on tumor location and the general state of the patients. Long-term follow-up should be applied to epithelioid hemangioendothelioma patients to improve clinical outcomes.
Keywords: Epithelioid hemangioendothelioma; Vascular malignancy; Angiosarcoma; ERG; CAMTA1
Key Points
In this study, we observed that EHEs from different anatomic sites shared some clinicopathological features. For example, the slight predominance of middle-aged females, multifocal growth pattern, and the expression of endothelial IHC markers, such as ERG, and CD31, were common in the lesions. The endovascular flowerlike structure and intracytoplasmic vacuoles of neoplasm cells were remarkable diagnostic clues for EHE, especially in biopsies. The epithelial morphological appearance and controversially low Ki67 index (≤10%) were essential clues.
Although EHEs had a tendency of multifocal occurrence in the liver and lung, it was biologically indolent, with a 5-year survival rate of over 75% in our study. The prognosis depends mainly on tumor location and the general state of the patients. Multiple treatments and long-term follow-up should be applied to EHE patients to improve the clinical outcome.
Introduction
Epithelioid hemangioendothelioma (EHE) is a rare vascular neoplasm that can arise anywhere in the body with relatively less aggressive clinical progression. The most commonly involved anatomic locations were soft tissue, bone, liver, and lung [1-5]. Cases of EHE have been documented in any period of adulthood, with an incidence peak in the fourth and fifth decades [6] and a low incidence in children and adolescent patients [7,8]. In addition, females were slightly more predominant in gender distribution [9-11]. Despite having a regularly multifocal development pattern, the biological behavior of EHE was indolent. EHE had a prognosis between benign vascular neoplasm and highly malignant angiosarcoma, with a relatively favorable five-year overall survival rate of more than 70% [10,11].
Since EHE is extremely rare and morphologically variable, it is difficult to make a concise pathological diagnosis, particularly in biopsies. Furthermore, cases in splanchnic organs, such as the liver and lung, are always multiple lesions. With the clustered growth pattern and the typical cytoplasm-sufficient tumor cells, it is not uncommon for biopsy specimens to be mistaken as metastatic poorly differentiated carcinoma [12,13], which may result in overtreatment for EHE patients. As a result, accurate pathological diagnosis is extremely important. However, due to the small number of EHE cases, comparing the morphological, immunohistochemical, and prognosis characteristics of tumors arising in various body parts is challenging. Except for the previously documented intrasinusoidal growth pattern in hepatic EHE [14], there is relatively little information in the literature about organ-specific histology of EHE. Do they have similar or organ-specified morphological features and clinical outcomes? Do we need to apply distinct treatment strategies for EHE rising from different sites? Our knowledge is still quite inadequate of this rare malignancy.
In this study, we collected 34 EHE cases that were diagnosed and treated in both National Cancer Center/Cancer Hospital and affiliated Shenzhen Cancer Hospital in China. The tumors were found in seven anatomical locations, including liver, lung, bone, front mediastinum, subcutaneous, adrenal gland, and supraclavicular tissues. The diagnoses were made by either biopsy or the dissected tissues. For cancers involving diverse locations, detailed clinicopathologic and prognostic information was examined and summarized. Hopefully, our study will enhance the knowledge of this rare tumor and improve its clinical management.
Materials and Methods
Patient Selection
A total of 34 cases of EHE were selected in two centers (National Cancer Center/Cancer Hospital and affiliated Shenzhen Cancer Hospital) from January 2011 to March 2021, and their medical data were retrieved. Three senior pathologists reviewed the hematoxylin and eosin stained and immunohistochemical slides from each case to confirm the diagnosis of EHE. The diagnosis was made when the tumor showed typical morphology and expressed endothelial markers such as ERG, CD31, or CD34.
Clinical Information Records and Follow-Up
Clinical characteristics such as patient age at presentation, gender, medical history, number and location of the lesion (solitary or multifocal), the existence of distant metastasis, and date of last follow- up or death were recorded.
Immunohistochemistry
Immunohistochemistry staining was done on 4-μm-thick formalin-fixed and paraffin-embedded (FFPE) tissue slides. The primary antibodies included anti-ERG (Ventana, prediluted), anti- CD31(Ventana, prediluted), anti-AE1/AE3 (Dako, prediluted), anti-CAMTA1 (Novus Biologicals, Littleton, CO), and anti-TFE3 (CellMarque, Rocklin, CA). Heat-induced antigen retrieval was used, and the EnVision system (Dako) was used for detection. The staining results were classified as negative (<25% positive cells), mildly positive (1+, 25-50% positive cells, with light yellow or light brown signals), and strongly positive (2+, 25-50% positive cells, with dark brown signals or 3+, ≥ 50% positive cells, with dark brown signals).
Statistical Analyses
SPSS software, version 22.0, was used to analyze the data (IBM Corporation, New York, NY, USA). The Kaplan-Meier method was used to compute the survival rates based on the date of either the clinical record or phone follow-up. Results with P-value <0.05 were considered significant for all statistical analyses.
Results
Clinicopathological Characteristics
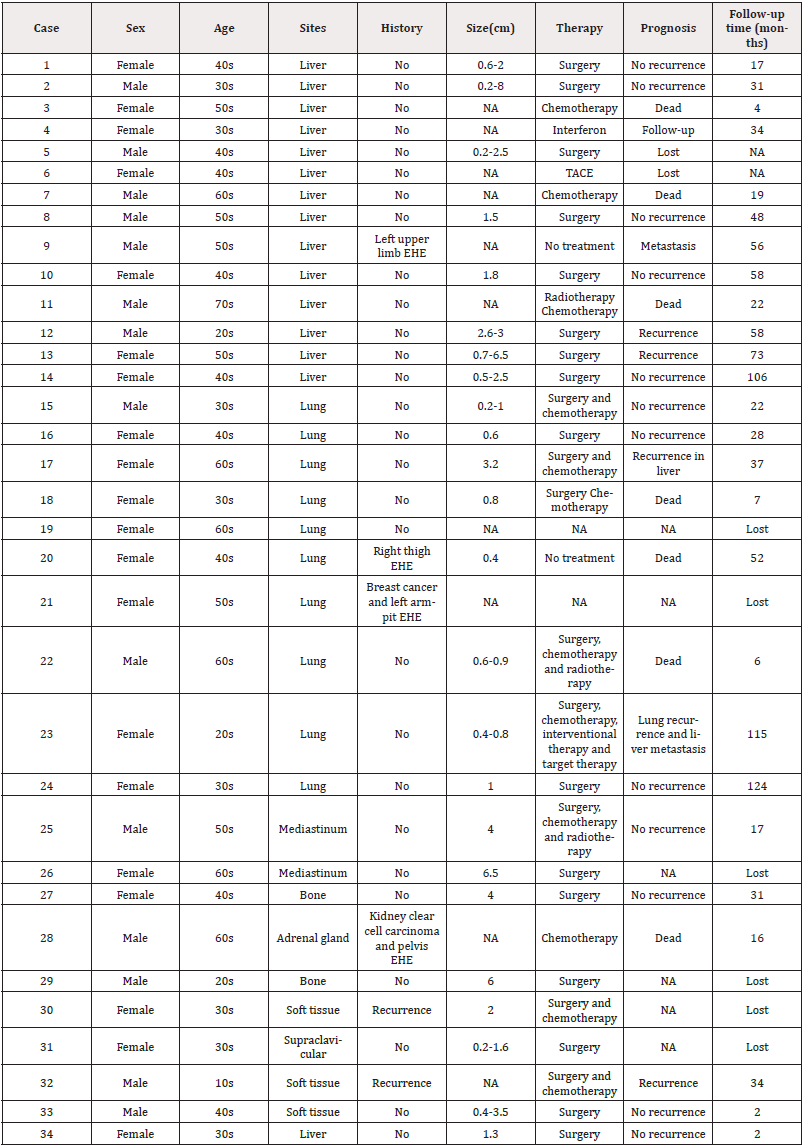
A total of 34 patients were diagnosed as EHE at National Cancer Center/Cancer Hospital (N=31) and affiliated Shenzhen Cancer Hospital (N=3) between January 2011 and March 2021, including 14 (41.2%) males and 20 (58.8%) females, with a median age of 46.6 years (range from 16 to 75 years). Table 1 summarizes the basic clinicopathological facts. Seven locations were involved, including liver (N=15), lung (N=10), skin and soft tissue (N=3), bone (N=2), anterior mediastinum (N=2), adrenal gland (N=1) and left supraclavicular (N=1). There were 28 cases of original neoplasms (including three with lymph node metastases), while the others had recurrent neoplasms (N=2, both occurring in soft tissue) or metastatic neoplasms (N=4, 2 occurring in the lung, 1 in the liver and 1 in the adrenal gland). Only five of the 28 primary EHE were solitary lesions (including 2 bones, 2 anterior mediastina, and 1 supraclavicular case). The remaining 23 instances were multifocal, with the liver being the most affected organ (N=15). In our study, the tumors involving the liver were frequently close to the capsule and multi-centered and mostly occurred in middle-aged and elderly patients. Thus, no wonder metastatic carcinoma and intrahepatic cholangiocarcinoma were the top two considerations for radiological diagnoses.
Massive and Microscope Features
The study included 24 cases of surgically dissected samples and 10 cases of biopsy samples. The latter were from liver (N=6), lung (N=2), skin (N=1), and adrenal gland (N=1). The dissected tumors appeared as solid masses with either pale white or pale-yellow color. Although the tumors were often well defined, no capsule was found in any of the 24 cases. Liver capsule and pleural invasion were observed in seven hepatic (7/9, 77.8%) and one pulmonary (1/8, 12.5%) cases, respectively.
Under the microscope, a multi-nodular-forming structure was found in 20 of the 24 cases (83.3%, Figure 1A), including all the dissected tumors of liver (9/9) and lung (8/8), two of the three soft tissue, and one of the two bone tumors. The tumor cells are arranged in clusters, cords, nests, and strands (Figure 1B-1D). The nodules were made up of epithelioid tumor cells densely distributed near the edge and sparsely in the center. The center portion of the nodules exhibited hyalinization, calcification, and cholesterol crystals. Thus, the lesions arising in lung were morphologically analogous to granulomatous inflammation sometimes, leading to the misdiagnosis of pulmonary tuberculosis in the frozen section. The nodular formation was absent in the other six surgical samples that affected the mediastinum (N=2), left supraclavicular (N=1), bone (1/2), and soft tissue (1/3).

Figure 1: Histology appearance of EHE. The typical nodular growing pattern (A). Tumor cells arranged in nests, clusters, cords, and pseudoglandular structures (B-D). The classical intracellular vacuoles similar to signet ring like cells (E). Endovascular flower-like structure (F).
Under the moderate to high power view, the tumors were characterized by middle-sized epithelioid cells arranged in cords, clusters, papillary and glandular patterns. Signet ring-like or vacuolated cells were present in 31 cases (91.2%) (Figure 1E). In addition, immature blood vessel was encountered in 20 cases (58.9%), with a single red blood cell presented in the tiny vascular cavity (Figure 1E). The tumor cells were generally short fusiform, spindle, or epithelioid with abundant eosinophilic cytoplasm and vesicular nuclei. In all cases, the nucleoli were indistinguishable. The nuclear atypia was mild to moderate, and the mitotic rate was usually low (0 to 2/10HPF), seemingly incompatible with its growth pattern.
Aside from the normal endothelial features, the endovascular flower-like structure was another diagnostic clue frequently observed in dissected EHE samples. This structure was characterized by papillae covered by tumor cells protruding into the lumen of a small to medium-sized blood vessel. This special structure was discovered in 19 cases of (79.2%) dissected specimens (Figure 1F).
Lymph node biopsy and dissection were performed on five patients, three of whom had lymph node metastases. During the follow-up period, one patient died of disease and the other two patients with lymph node metastasis were alive. There was no evidence of nerve invasion in the 34 cases.
Immunohistochemistry Detection
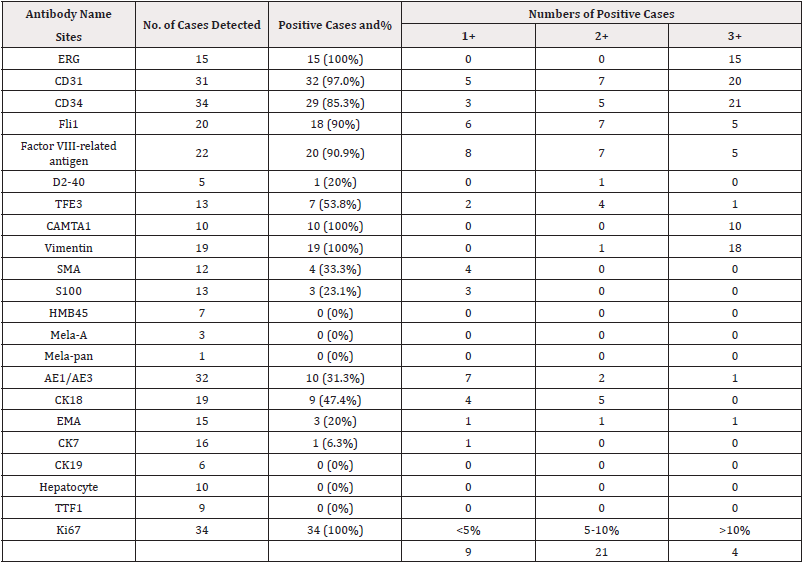
Immunohistochemistry staining was carried out on all the 34 EHE samples. The major staining results are summarized in Table 2. The most prevalent positive markers were ERG, CD31, CD34, and CAMTA1 (Figure 2A-2D). 15/15 (100%) cases were detected with strong positivity for ERG staining. 32/33 (97.0%) cases were with CD31 expression. 29/34 (85.3%) cases demonstrated CD34 positivity in the cytoplasm. Factor VIII was expressed in 20/22 (90.9%) cases, followed by Fli1(18/20, 90%). D2-40 expression was only observed in one case (1/5, 20%). Mesenchymal markers demonstrated diffuse or focal expression, such as Vimentin (19/19, 100%), SMA (4/12, 33.3%), and S100 (3/13, 23.1%). Markers like HMB45, Melan-A, Mela-pan, CR, and MC were negative.
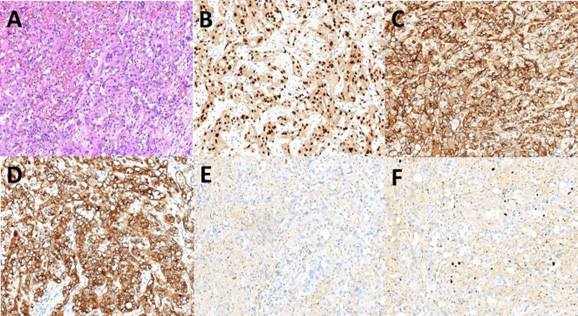
Figure 2: Typical immunohistochemistry staining of EHE. The epitheloid neoplasm cells (A). Positive ERG staining in all the tested EHE cases (B), followed by positive CD31 and CD34 in most detected cases (C-D). Negative AE1/AE3 staining (E). Ki67 index lower than 10% (F).
Compared to the diffuse and strong positivity of the vascular makers, the expression of epithelial markers was either focally weak or negative in EHE. The most frequently positive marker was CK18 (9/19, 47.4%), followed by AE1/AE3 (10/32, 31.3%), EMA (3/15, 20%) and CK7 (1/16, 6.3%) (Figure 2E). Entirely negatively expressed markers included CK19(0/6), Hepatocyte (0/10), TTF1 (0/9), and CK20 (0/2).
Furthermore, a low Ki67 index (≤10%) was demonstrated in 30 (88.2%) EHE cases that occurred in various anatomic sites (Figure 2F). Only four cases had a Ki67 index greater than 10%, including three cases with metastasis and recurrence and one who died of the disease shortly after surgery and chemotherapy. As a result, a greater Ki67 index suggested an increased chance of an unsatisfactory clinical outcome, consistent with prior findings [15].
Treatment and Prognosis
Multiple treatments were applied to the 34 EHE patients after pathological diagnosis. The most prevalent treatment option was surgery, which was chosen by 24 patients (70.6%), including one recurrent and one metastatic case. Two of the ten biopsy cases were lost throughout the follow-up period; thus, treatment data was unavailable (2/10). Chemotherapy was the most frequent treatment (3/8) for biopsy diagnosed EHE patients, followed by combined chemotherapy and radiotherapy (1/8), TACE (1/8), interferon intramuscular injection (1/8), amputation of thigh (1/8) and clinical follow-up (1/8).
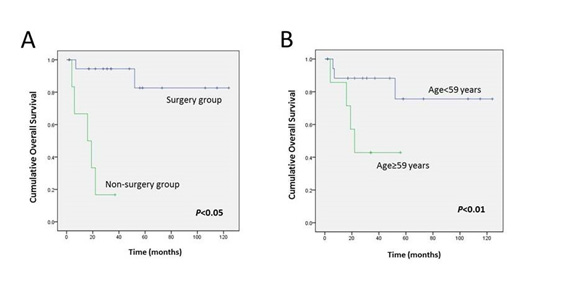
The follow-up records for 26 EHE patients were available, whereas the other 8 cases were lost. The average recorded time was 39.2 months, ranging from 2 to 124 months. 7 patients died of the disease (26.9%), of which 5 cases were elder than 59 years at the time of diagnosis (71.4%, ranged from 38 to 75 years). 12 cases (46.2%) were clinically cured without recurrence up to date. 7 cases (26.9%) survived with primary or recurrent tumors.
Discussion
EHE is a rare malignant vascular neoplasm that primarily affects people aged 40 to 50, with a slight predominance in women. In this study, 14 males (41.2%) and 20 females (58.8%) were included, with a median age of 46.6 years. According to previous studies, EHE is extremely rare in childhood and adolescence [7,16]. Moreover, there is only one patient under adulthood in our research group, a 16-year-old patient. This neoplasm can appear anywhere in the body [6,17,18]. In our research, the liver, lung, soft tissue, and bone were the most frequently involved organs. A number of EHE occurred asymptomatically, especially in Chinese patients [19]. Up to 50% of patients (17 cases in our research) were accidentally detected by routine body examination. Ache (8 cases, 47%) was the most common symptom, followed by palpable painful mass (4 cases, 23%), bleeding (3 cases, 18%), fever (1 case, 6%), and chest tightness (1 case, 6%). The clinical manifestation of EHE was nonspecific and may appear distinctly in different anatomic sites.
In our study, EHE from distinct anatomic sites shared several morphology features in common. First, the multi-nodular growth patterns with uneven cellular distribution were present in 19 excisional cases (19/24, 79.2%), including all nine dissected hepatic, eight pulmonary, one subcutaneous, and one bone lesions. The pushing rather than destructive infiltration was consistent with EHE’s relatively slow progression [20]. Second, it frequently showed multiple lesions with solid, or nest-like growth patterns composed of cytoplasm-sufficient cells. These characteristics were all diagnostic pitfalls that were easily confused with metastatic cancers, particularly in the liver and lung. The low mitotic activity of EHE may help in differentiation diagnosis. In most of our cases, the average mitotic rate was less than 2/10HPF. The only exception was a recurrent lesion in a 16-year-old patient, where the mitotic rate was 5-6/10HPF with a high Ki67 index. Third, the endovascular flowerlike structure and the immature blood vessel were remarkable and identical and can be helpful as diagnostic clues.
Immunohistochemistry was crucial for the accurate diagnosis of EHE. There was a consistently strong and diffuse expression of more than one endothelial marker, especially ERG and CD31, as well as CD34, Fli1, and F8. On the other hand, epithelial markers like AE1/AE3, EMA and low molecular weight keratin, such as CK18, CK19, and CK7, were either negative or focally and weakly positive in EHE, which was extremely useful for distinguishing from metastatic carcinomas. Besides, Ki67 was necessary for EHE diagnosis. In our study, the Ki67 index was either lower than or equal to 10% in most of the cases (30/34, 88.2%). Furthermore, novel markers such as CAMTA1 and TFE3 were used in the differentiation of hemangioma and angiosarcoma, which were totally negative for both the markers [21,22]. As per other research groups, CAMTA1 was more sensitive and specific than TFE3 [23-25]. Our findings from ten pulmonary EHE revealed that the immunohistochemical staining of CAMTA1 was diffusely positive in all the cases, with significant nuclear signals. Moreover, TFE3 was either negative or weakly positive, and a typical TFE3 gene fusion was only found in one case. Unlike previous studies, the case with TFE3-YAP1 fusion showed conventional morphology without predominant nuclei and abundant vascularization [26]. As a result, we conclude that CAMTA1 can be utilized as a potential immunohistochemical marker in differential diagnosis, which is consistent with the previous studies, and TFE3-YAP1 fusion can be detected in some EHE cases [11,27].
In many countries, surgery is still the first option for treating EHE. According to a recent ESMO consensus, complete resection of neoplasm (R0 resection) is highly recommended to reduce the recurrent risk, especially in unifocal EHE lesions [9]. For clinical studies of unresectable multiple neoplasms, chemotherapy, radiotherapy, and anti-vascular forming target therapy were carried out [28].
Although EHE arising in different body parts presented with similar histological features, the clinical result varied significantly. According to our experience, pulmonary EHE cases suffered a worse prognosis than the liver, bone, or soft tissue lesions, which was consistent with previous studies [3,28-30]. Interestingly, the liver involvement in EHE cases was not that fatal unless the patients had simultaneous lung lesions. The factors related to aggressive biological behavior of EHE included age >59 years, unresectable lesions, development of complications, Ki67 index >10%, mitotic count >2/10HPF, lymph node metastasis, and pleura invasion (Figure 3A,3B). Moreover, age >59 years and unresectable lesions were only statistically significant (P <0.05).
Conclusion
EHE is an extremely rare vascular malignancy with various clinicopathological appearances. The endovascular flower-like structure and the cells with intracytoplasmic vacuoles were remarkable diagnostic clues. Immunohistochemical markers ERG, CD31, and CAMTA1 are more helpful than CD34, Fli1, and F8. Consistent with its indolent clinical progress, the 5-year survival rate of EHE is over 75%. The factors including age elder than 59 years, development of complications, Ki67 index higher than 10%, mitotic count more than 2/10HPF, lymph node metastasis, and pleura invasion indicated a poor prognosis. The prognosis is primarily determined by the tumor location and the general state of the patients. Multiple treatment and long-term follow-up should be done on EHE patients to improve the clinical outcome.
Funding and Conflict of Interests
This study is supported by the funding of The National Key Research and Development Program of China (Grant number: 2021YFF1201300). The authors have no competing interests to declare that are relevant to the content of this article.
Ethics Approval and Consent to Participate
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of Cancer Hospital Chinese Academy of Medical Sciences. The approval number is 20/248-2444.
References
- Sardaro A, Bardoscia L, Petruzzelli MF, Portaluri M (2014) Epithelioid hemangioendothelioma: an overview and update on a rare vascular tumor. Oncol Rev 8(2): 259.
- Weissferdt A, Moran CA (2014) Epithelioid hemangioendothelioma of the bone: a review and update. Adv Anat Pathol 21(4): 254-259.
- Shao J, Zhang J (2014) Clinicopathological characteristics of pulmonary epithelioid hemangioendothelioma: A report of four cases and review of the literature. Oncol Lett 8(6): 2517-2522.
- Makhlouf HR, Ishak KG, Goodman ZD (1999) Epithelioid hemangioendothelioma of the liver: a clinicopathologic study of 137 cases. Cancer 85(3): 562-582.
- Errani C, Zhang L, Panicek DM, Healey JH, Antonescu CR (2012) Epithelioid hemangioma of bone and soft tissue: a reappraisal of a controversial entity. Clin Orthop Relat Res 470(5): 1498-1506.
- Rosenberg A, Agulnik M (2018) Epithelioid Hemangioendothelioma: Update on Diagnosis and Treatment. Curr Treat Options Oncol 19(4): 19.
- Cournoyer E, Al Ibraheemi A, Engel E, Chaudry G, Stapleton S, et al. (2020) Clinical characterization and long-term outcomes in pediatric epithelioid hemangioendothelioma. Pediatr Blood Cancer 67(2): e28045.
- Chavhan GB, Siddiqui I, Ingley KM, Gupta AA (2019) Rare malignant liver tumors in children. Pediatr Radiol 49(11): 1404-1421.
- Stacchiotti S, Miah AB, Frezza AM, Messiou C, Morosi C, et al. (2021) Epithelioid hemangioendothelioma, an ultra-rare cancer: a consensus paper from the community of experts. ESMO Open 6(3): 100170.
- Frezza AM, Napolitano A, Miceli R, Badalamenti G, Brunello A, et al. (2021) Clinical prognostic factors in advanced epithelioid haemangioendothelioma: a retrospective case series analysis within the Italian Rare Cancers Network. ESMO Open 6(2): 100083.
- Rosenbaum E, Jadeja B, Xu B, Zhang L, Agaram NP, et al. (2020) Prognostic stratification of clinical and molecular epithelioid hemangioendothelioma subsets. Mod Pathol 33(4): 591-602.
- Din NU, Rahim S, Asghari T, Abdul-Ghafar J, Ahmad Z (2020) Hepatic epithelioid hemangioendothelioma: case series of a rare vascular tumor mimicking metastases. Diagn Pathol 15(1): 120.
- Weiss SW, Enzinger FM (1982) Epithelioid hemangioendothelioma: a vascular tumor often mistaken for a carcinoma. Cancer 50(5): 970-981.
- Agostini Vulaj D, Pehlivanoglu B, Weiss SW, Krasinskas A, Feely MM, et al. (2019) Intrasinusoidal Spread of Hepatic Epithelioid Hemangioendothelioma: Implications for the Diagnosis in Minimal Samples. Am J Surg Pathol 43(4): 573-579.
- Shiba S, Imaoka H, Shioji K, Suzuki E, Horiguchi S, et al. (2018) Clinical characteristics of Japanese patients with epithelioid hemangioendothelioma: a multicenter retrospective study. BMC Cancer 18(1): 993.
- Song W, Zhen Z, Li L, Ye J, Zhou S, et al. (2020) Epithelioid hemangioendothelioma of the sternum. Thorac Cancer 11(6): 1741-1745.
- Deng Y, Yan R, Liu R, Song B (2021) Primary cardiac epithelioid haemangioendothelioma. Eur Heart J 42(15): 1532.
- Thway K, Mentzel T, Perrett CM, Calonje E (2018) Multicentric visceral epithelioid hemangioendothelioma, with extremity dermal deposits, unusual late recurrence on the nasal bridge, and TFE3 gene rearrangement. Hum Pathol 72: 153-159.
- Zhao XY, Rakhda MI, Habib S, Bihi A, Muhammad A, et al. (2014) Hepatic epithelioid hemangioendothelioma: A comparison of Western and Chinese methods with respect to diagnosis, treatment and outcome. Oncol Lett 7(4): 977-983.
- Li Z, Du Q, Ma PQ, Zhang HF, Zhang HT (2021) [Clinicopathological characteristics of hepatic epithelioid haemangioendothelioma]. Zhonghua Bing Li Xue Za Zhi 50(5): 511-513.
- Jung H, Kim HN, Jang Y, Park CK, Ha SY (2019) CAMTA-1 Expression in 24 Cases of Hepatic Epithelioid Hemangioendothelioma in a Single Institute: Diagnostic Utility for Differential Diagnosis from Hepatic Angiosarcoma. In Vivo 33(6): 2293-2297.
- Habeeb O, Rubin BP (2019) The Molecular Diagnostics of Vascular Neoplasms. Surg Pathol Clin 12(1): 35-49.
- Shibuya R, Matsuyama A, Shiba E, Harada H, Yabuki K, et al. (2015) CAMTA1 is a useful immunohistochemical marker for diagnosing epithelioid haemangioendothelioma. Histopathology 67(6): 827-835.
- Kuo FY, Huang HY, Chen CL, Eng HL, Huang CC (2017) TFE3-rearranged hepatic epithelioid hemangioendothelioma-a case report with immunohistochemical and molecular study. APMIS 125(9): 849-853.
- Zhang HZ, Dong L, Wang SY, Yang XQ (2020) TFE3 rearranged epithelioid hemangioendothelioma of bone: A clinicopathological, immunohistochemical and molecular study of two cases. Ann Diagn Pathol 46: 151487.
- Antonescu CR, Le Loarer F, Mosquera JM, Sboner A, Zhang L, et al. (2013) Novel YAP1-TFE3 fusion defines a distinct subset of epithelioid hemangioendothelioma. Genes Chromosomes Cancer 52(8): 775-784.
- Flucke U, Vogels RJ, de Saint Aubain Somerhausen N, Creytens DH, Riedl RG, et al. (2014) Epithelioid Hemangioendothelioma: clinicopathologic, immunhistochemical, and molecular genetic analysis of 39 cases. Diagn Pathol 9: 131.
- Noh OK, Kim SS, Yang MJ, Lim SG, Hwang JC, et al. (2020) Treatment and prognosis of hepatic epithelioid hemangioendothelioma based on SEER data analysis from 1973 to 2014. Hepatobiliary Pancreat Dis Int 19(1): 29-35.
- Han J, Wei JG, Gao XZ, Xu Y, Zhang L, et al. (2020) [Clinicopathological features of pulmonary epithelioid hemangioendothelioma: a study of 18 cases]. Zhonghua Bing Li Xue Za Zhi 49(6): 550-555.
- Mucientes P, Gomez-Arellano L, Rao N (2014) Malignant pleuropulmonary epithelioid hemangioendothelioma-unusual presentation of an aggressive angiogenic neoplasm. Pathol Res Pract 210(9): 613-618.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.