Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Frequency of Anterior Knee Pain After Total Knee Arthroplasty
*Corresponding author: Imran Khan, Department of Orthopedic and Trauma, Medical Teaching Institute Lady Reading Hospital Peshawar, Pakistan.
Received: June 06, 2023; Published: June 13, 2023
DOI: 10.34297/AJBSR.2023.19.002561
Abstract
Introduction: Anterior Knee Pain (AKP) is one of the most common causes of persistent problems after knee replacement. Total Knee Arthroplasty (TKA) is a surgical procedure in which an artificial joint or prosthesis replaces the damaged knee. A significant proportion of the patients experience AKP after surgery. The pain is described as a retro patellar or peripatellar pain. Patients have trouble standing from sitting position, walking up and down stairs, and riding a bicycle in AKP.
Objective: To determine the frequency of Anterior Knee Pain after Total Knee Arthroplasty.
Material and Methods: This Cross-sectional study was carried out in the Department of Orthopedics, Khyber Teaching Hospital, Peshawar on 205 consecutive patients of either sex from June 2020 to January 2021.After recording complete history, physical examination and routine baseline investigations were done. Patients were put on OT list and surgeries were performed on all patients by expert orthopedic surgeon designated for performing total knee arthroplasty. Post-operatively, patients were kept under observation for 5 days in ward and were discharged if indicated. Patients were followed at regular intervals and finally at the end of the 3rd month to measure the intensity of pain on VAS.
Results: Out of 205 patients, 69.3% were males and 30.7% were females. Means±SD calculated for age was 48.62±7.98 years, for BMI was 24.63±3.07 and for Pain on VAS was 1.31±1.39. Most patients (51.7%) were recorded in the 51-60 years age group. Rheumatoid Arthritis (RA) in 18% while Osteoarthritis (OA) was found in 82% patients. 21.5% of patients were diabetic while 31.7% patients were hypertensive. AKP at 3rd month was found in 8.8% patients.
Conclusion: It is evident that Anterior Knee Pain (AKP) after the Total Knee Arthroplasty (TKA), or Total Knee Replacement (TKR) is prevalent and clinically relevant. There is an absolute necessity for further investigations to find out ways to reduce or eliminate the AKP after TKA to improve the quality of life after this surgery.
Keywords: Anterior knee pain, Patella, Total knee arthroplasty, Total knee replacement
Introduction
Anterior knee pain is one of the most common causes of persistent problems after total knee replacement. According to the literature, the rates of satisfaction after total knee arthroplasty (TKA) vary between 75 and 89% [1-3]. It can occur with or without patellar resurfacing. Sensi, et al. [4]. reported incidence of 8% anterior knee pain after TKA [4]. The intensity of pain is mostly mild to moderate. Nevertheless, after joint infection, patello-femoral problems are one of the most common reasons for reoperation or revision after TKA [5]. Total Knee Arthroplasty is a common surgical procedure in which artificial joints or prosthesis replace damaged knee. It’s mostly used for treating patients with osteoarthritis [6], still a significant proportion of the patients experience Anterior Knee Pain (AKP) after surgery. The pain is described as a retro patellar or peripatellar pain-limiting patients in their everyday activities. Patients experience difficulty in standing from sitting position, walking up and down stairs, and riding a bicycle in case of AKP [7].
For understanding of anterior knee pain after Total Knee Arthroplasty, it is important to have knowledge about healthy functioning knee. According to Dye theory, “the healthy knee is a complex assemblage of living asymmetrical moving parts whose purpose is to accept, transfer, and ultimately dissipate often high loads generated at the ends of the long mechanical lever arms of the femur, tibia, patella, and fibula” [8]. Furthermore, Dye’s refers to each knee having a unique “envelope of function”; a potential range of activity in which it maintains a homeostasis of all surrounding tissues [9]. The potential range of activity is different for individual knees, whether healthy, arthritic or with a knee arthroplasty. An arthritic knee can be viewed as a transmission with worn bearings, and thus with a limited capacity to accept and transfer loads [10]. In one study, 20.2% of patients subjected to TKA reported with AKP on follow up [11]. In another study, 8% of osteoarthritis and 7% of rheumatoid arthritis patients reported with AKP after subjecting to TKA [12].
The present study was designed to determine frequency of AKP after TKA. Doing a thorough literature search, we found that very rare data exists regarding the frequency of Anterior Knee Pain after Total Knee Arthroplasty and available data suggests variation in its magnitude from one setting to another. This study will be an attempt to determine the frequency of Anterior Knee Pain in our local population subjected to Total Knee Arthroplasty.
The main objective of this study was to determine the frequency of Anterior Knee Pain (AKP) after Total Knee Arthroplasty (TKA) in patients presented to Department of Orthopedic Surgery in Khyber Teaching Hospital Peshawar.
Material and Methods
This Cross-sectional study was carried out in the Department of Orthopedics, Khyber Teaching Hospital, Peshawar on 205 consecutive patients from June 2020 to January 202. All patients scheduled for TKA irrespective of indication of age above 30 to 60 years with either sex was included in the study while patients with BMI of more than 30kg/m2 Immunocompromised patients (diabetics with Fasting Blood Glucose of >126mg/dl, malignancy diagnosed through past medical records, patients with HIV/AIDS (diagnosed through medical records and patients with history of intake of steroids in the last 2 weeks). Patients with debilitating diseases like chronic liver, renal or cardiac impairment (diagnosed based on medical records and history) were excluded from the study.
The study was carried out after getting approval from the hospital’s ethical and research committee. OPD/ER patients meeting the inclusion criteria were included in the study. The purpose, risks and benefits of the study were explained to all included patients in detail. They were assured that the study was purely conducted for research and data publication and written informed consents were obtained from all included patients. The complete history of all patients was recorded very keenly. Complete physical examination and routine pre-operative baseline investigations were done for all patients. According to hospital’s protocols, patients were put on OT list and surgeries were performed in all patients by single expert orthopedic surgeon who was fellow of CPSP and designated for performing total knee arthroplasty.
Post operatively, all patients were kept under observation for 5 days in ward and were discharged if indicated. The patients were followed at regular intervals and finally at the end of the 3rd postoperative month to measure the intensity of pain on Visual Analogue Scale (VAS) and label as presence or absence of Anterior Knee Pain. All the above-mentioned information including name, age, gender, address, and telephone numbers were recorded on a predesigned proforma. Exclusion criteria were followed strictly to control confounders and bias in the study results. All the data was entered and analyzed in SPSS 20. Mean±SD were calculated for numerical variables like age, BMI and pain on VAS. Frequencies and percentages were calculated for categorical variables like gender, indications for TKA (Rheumatoid Arthritis and Osteoarthritis), diabetes mellitus, hypertension and Anterior Knee Pain at 3rd month follow up. Anterior Knee Pain was stratified among age, gender, indications for TKA (Rheumatoid Arthritis and Osteoarthritis), diabetes mellitus and hypertension to see the effect modifiers using chi square test with P value < 0.05 as significant. All the results have been presented as tables.
Results
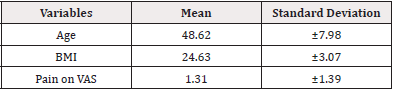
A total of 205 patients were recruited as per sample size calculated through WHO software to conduct this study at the Department of Orthopedic Surgery, Khyber Teaching Hospital, Peshawar. Means and Standard Deviation calculated for age was 48.62±7.98 years, for BMI was 24.63±3.07 and for Pain on VAS (at 3rd month follow up) was 1.31±1.39 (Table 1).
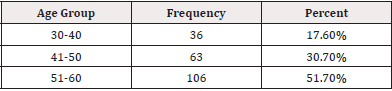
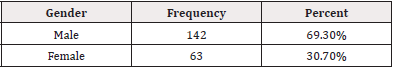
Total population was distributed in three age groups, wherein 51.7% patients were recorded in 51-60 years age group, 30.7% patients were recorded in 41-50 years age group and 17.6% patients were recorded in 30-40 years age group (Table 2). As per gender distribution, 69.3% patients where male while 30.7% patients were female (Table 3).
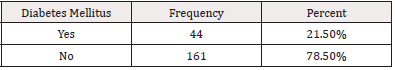
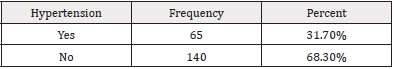
After recording the indications for Total Knee Arthroplasty (TKA) in all 205 patients, Rheumatoid Arthritis (RA) was found in 18% patients while Osteoarthritis (OA) was found in 82% patients (Table 4). Similarly, in total study population, 21.5% patients were diabetic, and 78.5% patients were non-diabetic (Table 5) while 31.7% patients were hypertensive, and 68.3% patients were non-hypertensive (Table 6).

Table 8: Stratification of Anterior Knee Pain (Akp) With Respect to Age (N = 205).
Note*: P Value = 0.727
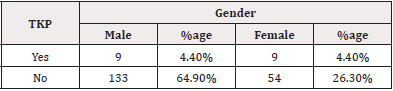
Table 9: Stratification of Anterior Knee Pain (Akp) With Respect to Gender (N = 205).
Note*: P Value = 0.064
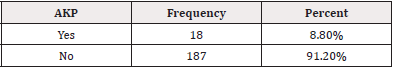
Anterior Knee Pain (AKP) at 3rd month follow up was found in 8.8% patients while it was absent in 91.2% patients according to our operational definition (Table 7). Anterior Knee Pain (AKP) at 3rd month follow up was stratified with respect to age, wherein it was found that 1.5% patients in 30-40 years age group, 3.4% patients in 41-50 years age group and 3.9% patients in 51-60 years age group were feeling Pain (AKP). On the other hand, 16.1% patients in the 30-40 years age group, 27.3% patients in 41-50 years age group and 47.8% patients in 51-60 years age group were not feeling the Pain (AKP) as per our operational definition (Table 8). Anterior Knee Pain (AKP) at 3rd month follow up was stratified with respect to gender wherein it was found 4.4 % male patients and 4.4% female patients were still feeling the pain while 64.9% male patients and 26.3% female patients were not feeling the pain at 3rd month follow up (Table 9).
Anterior Knee Pain (AKP) at 3rd month follow up was stratified with respect to indications for TKA (Rheumatoid Arthritis or Osteoarthritis), wherein it was found that 2.4% of the patients who were having Rheumatoid Arthritis and 6.3% of the patients who were having Osteoarthritis were still feeling the pain. On the other hand, 15.6% of the patients who were having Rheumatoid Arthritis and 75.6% of the patients who were having Osteoarthritis were not feeling the pain (Table 10).
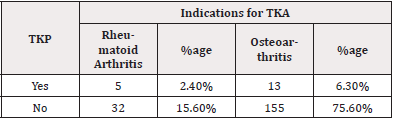
Table 10: Stratification of Anterior Knee Pain (Akp) With Respect to Indications for Tka (N = 205).
P Value = 0.261
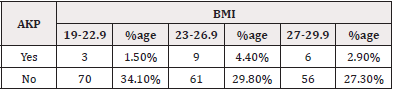
Anterior Knee Pain (AKP) at 3rd month follow up was stratified with respect to Body Mass Index (BMI), wherein it was found that 1.5% patients in 19-22.9 BMI group, 4.4% patients in 23-26.9 BMI group and 2.9% patients in 27-29.9 BMI group were feeling Pain (AKP). On the other hand, 34.1% patients in 19-22.9 BMI group, 29.8% patients in 23-29.9 BMI group and 27.3% patients in 27-29.9 BMI group were not feeling the Pain (AKP) as per our operational definition (Table 11).

Table 11: Stratification of Anterior Knee Pain (Akp) With Respect to Body Mass Index (Bmi) (n = 205).
Note*: P Value = 0.173
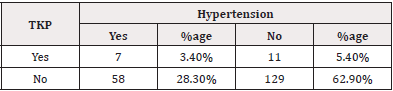
Anterior Knee Pain (AKP) at 3rd month follow up was stratified with respect to Diabetes Mellitus and Hypertension. Wherein it was found that 1.5% of the diabetic patients and 7.3% of the non-diabetic patients were still feeling the pain while 20% of the diabetic patients and 71.2% of the non-diabetic patients were not feeling the pain (Table 12). Similarly, 3.4% of the hypertensive patients and 5.4% of the non-hypertensive patients were still feeling the pain while 28.3% of the hypertensive patients and 62.9% of the non-hypertensive patients were not feeling the pain (Table 13).
Discussion
It has been estimated that clinically significant osteoarthritis of the knee currently affects 5% to 10% of people. With a predicted increase in life expectancy and an increasingly active population, the number of patients who are seeking treatment for significant pain and disability secondary to knee arthritis are undoubtedly increasing. In past, before 2005 it was considered that once a definitive diagnosis of osteoarthritis would be made, initial non-operative treatment modalities would include anti-inflammatory medications, heel wedges, off-loading knee braces, weight reduction, activity modification, and the use of ambulatory aids (e.g., cane, crutches). Failure of these non-operative methods to provide adequate relief might prompt treatment with infrequent use of intra- articular corticosteroid or Visco supplementation. But at last, surgical intervention with Total Knee Arthroplasty (TKA) was the need of the time which was offered to those who had exhausted non-operative attempts to improve quality of life. Occasionally, urgent referrals to orthopedic surgeons were indicated in patients who were presented with complaints of debilitating knee pain and radiographic evidence of severe bone loss and deformity on initial standard radiographs [13].
The most important finding of the current study is that various variables have been observed about the prevalence of AKP, with some clearly demonstrating a correlation with AKP. Patients’ characteristics including age, gender, BMI, diabetes mellitus, hypertension, and the presence of preoperative AKP were not found to be predictive of AKP. Knee-specific characteristics including diagnosis, radiographic grade of Osteoarthritis and Rheumatoid Arthritis, knee scores, range of motion, and deformity were not related to the occurrence of postoperative anterior knee pain [13,14].
While reviewing some studies [15,16], it was found that the occurrence of post- operative AKP was negatively correlated with patient satisfaction which is in accordance with the current study. Also, it was reported that patients with AKP had lower levels of quality of life than patients without AKP [17], which is quite rational particularly in elderly age. Considering the implications of AKP following TKA, patient satisfaction and quality of life, further study into the causative mechanisms of AKP is recommended to be conducted. In some other studies [18,19] a prior history of revision surgery was reported to be associated with AKP and impaired functional outcome. Each surgical intervention was reported adding up to a cumulative tissue injury and scar formation, which was hypothesized to be associated with concurrent increased activation as well as the intensity of the nociceptors being responsible for the experienced pronounced pain. Furthermore, it was also observed that the strength of the quadriceps muscle, the ability to stand from sitting on a chair, the thickness of the tibial inlay, and a radiologically measured PB were associated with experiencing postsurgical AKP. Logistic regression revealed that the inlay thickness, the strength of the quadriceps muscle, and the CD1 are associated with AKP, independently from the gender, BMI, age, knee re-surgery, and the number of months after surgery. Several investigations pointed out the importance of the function of the quadriceps muscle as a predictor of functional abilities in patients undergoing TKAs, especially for the elderly [20,21]. The observed association of AKP with reduced strength of the quadriceps muscle underlines the necessity of strength training and appropriate physical therapy. To accomplish a more profound approach to address the often-observed weakness of the quadriceps muscle, Werner, et al. [21], for instance, suggested a multiphasic approach, including an early correction of imbalance between the vastus medialis and vastus lateralis for physically active individuals with AKP. A significant association of the thickness of the tibial inlay with AKP was observed when comparing the samples and, in addition, as part of the logistic regression analysis as an independent variable, it was found that an independent association of the thickness of the tibial inlay with AKP, whereby participants having a thinner inlay implanted were more susceptible to experience postsurgical AKP. Multiple studies observed a correlation between different types and thicknesses of inlays and AKP [22-25]. It is conceivable that thinner inlays are predisposed for instability due to a slackening of the ligaments, which, in turn, may be related to AKP.
In line with previous studies, some studies were reviewed [26,27] wherein no association of AKP after TKA was found with the prosthetic design. Furthermore, it is not conclusively possible to clarify if the observed limited strength of the quadriceps muscle in participants with AKP is responsible for the postsurgical AKP or if the postsurgical AKP results in less loading of the leg, which impairs quadriceps muscle strength. To investigate further, future studies may consider focusing on quadriceps muscle strength of the uninvolved limb because patients tend to shift weight away from the operated limb. So that a causal relationship between postsurgical AKP and the ability to stand up from a chair can be finally drawn, and a careful interpretation of the obtained results may be made [22].
Conclusion
Postoperative pain is the most common complication after any surgery. It is evident that Anterior Knee Pain (AKP) after the Total Knee Arthroplasty (TKA), or Total Knee Replacement (TKR) is prevalent and clinically relevant. It is concluded that there is an absolute necessity for further investigations to find out ways to reduce or eliminate the AKP after TKA to improve the quality of life after this surgery.
Acknowledgments
None.
Conflict of Interest
None.
References
- Schnurr C, Jarrous M, Giidden I, Eysel P, Konig DP (2013) Pre-operative arthritis severity as a predictor for total knee arthroplasty patients' satisfaction. Int Orthop 37(7): 1257-1261.
- Chen K, Li G, Fu D, Yuan C, Zhang Q, et al. (2013) Patellar resurfacing versus nonresurfacing in total knee arthroplasty: a meta-analysis of randomised controlled trials. Int Orthop 37(6): 1075-1083.
- Petersen W, Rembitzki IV, Bruggemann GP, Ellermann A, Raymond Best, et al. (2014) Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop 38: 319-328.
- Sensi L, Buzzi R, Giron F, De Luca L, Aglietti P (2011) Patellofemoral function after total knee arthroplasty: gender-related differences. J Arthroplasty 26(8): 1475-1480.
- Li N, Tan Y, Deng Y, Chen L (2014) Posterior cruciate retaining versus posterior stabilized total knee arthroplasty: a meta-analysis of randomized controlled trials. Knee Surg Sports Traumatol Arthrosc 22: 556-564.
- Duan G, Liu C, Lin W, Shao J, Fu K, et al. (2018) Different factors conduct anterior knee pain following primary total knee arthroplasty: a systematic review and meta-analysis. J Arthroplast 33(6): 1962-1971.
- Dughbaj M, Shehab D, Ozcakar L (2017) Dynamic Ultrasound Imaging for Quadriceps Tendon Impingement in a Patient with Anterior Knee Pain. Pain Med 18(10): 2047-2048.
- Bigoni M, Zanchi N, Turati M, Pirovano G, Zatti G, et al. (2019) Short-term differences in anterior knee pain and clinical outcomes between rotating and fixed platform posterior stabilized total knee arthroplasty with a new femoral component design. World J Orthoped 10(3): 128-135.
- Flores DV, Mejia Gomez C, Pathria MN (2018) Layered approach to the anterior knee: normal anatomy and disorders associated with anterior knee pain. RadioGraphics 38(7): 2069-2101.
- Kwok KB, Fan JC, Hung YW, Chan AP, Bernard TW, et al. (2018) Iliotibial band impingement by overhanging tibial tray: A pain generator after total knee replacement treatable without revision. J Orthoped Trauma Rehab 25(l): 54-67.
- Metsna V, Vorobjov S, Martson A (2014) Prevalence of anterior knee pain among patients following total knee arthroplasty with nonreplaced patella: a retrospective study of 1778 knees. Medicina 50(2): 82-96.
- Pehlivanoglu T, Balci HI, Demirel M, Cakmak MF, Yazicioglu O, et al. (2019) Prevalence of anterior knee pain after patellar retention total knee arthroplasty: Comparison of patients with rheumatoid arthritis versus primary osteoarthritis. Acta Orthop Traumatol Turc 53(6): 420-425.
- Putman S, Boureau F, Girard J, Migaud H, Pasquier G (2019) Patellar complications after total knee arthroplasty. Orthop Traumatol Surg Res 105(1S): S43-S51.
- Kamal A, Dong RJ, Shah R, Li C (2020) Management of periprosthetic fractures of knee arthroplasty with revision surgery. J Orthop 22: 118-123.
- Barrack RL, Bertot AJ, Wolfe MW, Waldman DA, Milicic M, et al. (2001) Patellar resurfacing in total knee arthroplasty. A prospective, randomized, double-blind study with five to seven years of follow-up. J Bone Joint Surg (Am) 83(9): 1376-1381.
- Parvizi J, Rapuri VR, Saleh KJ, Kuskowski MA, Sharkey PF, et al. (2005) Failure to resurface the patella during total knee arthroplasty may result in more knee pain and secondary surgery. Clin Orthop Relat Res 438: 191-196.
- Breugem SJ, Sierevelt IN, Schafroth MU, Blankevoort L, Schaap GR, et al. (2008) Less anterior knee pain with a mobile-bearing prosthesis compared with a fixed-bearing prosthesis. Clin Orthop Relat Res 466(8): 1959-1965.
- Petersen KK, Simonsen O, Laursen MB, Thomas A Nielsen, Sten Rasmussen (2015) Chronic post- operative pain after primary and revision total knee arthroplasty. Clin J Pain 31(1): 1-6.
- Skou ST, Graven-Nielsen T, Rasmussen S, Ole H Simonsen, Mogens B Laursen (2013) Widespread sensitization in patients with chronic pain after revision total knee arthroplasty. Pain 154(9): 1588-1594.
- Connelly DM, Vandervoort AA (1997) Effects of detraining on knee extensor strength and functional mobility in a group of elderly women. J Orthop Spor Phys Ther 26(6): 340-346.
- Moxley Scarborough D, Krebs DE, Harris BA (1999) Quadriceps muscle strength and dynamic stability in elderly persons. Gait Post 10(1): 10-20.
- Werner S (2014) Anterior knee pain: an update of physical therapy. Knee Surg Sports Traumatol Arthrosc 22(10): 2286-2294.
- Keeney JA, Clohisy JC, Curry M, William J Maloney (2005) Revision total knee arthroplasty for restricted motion. Clin Orthop Rel Res 440: 135-140.
- Breugem SJ, Sierevelt IN, Schafroth MU, Leendert Blankevoort, Gerard R Schaap (2008) Less anterior knee pain with a mobile-bearing prosthesis compared with a fixed-bearing prosthesis. Clin Orthop Rel Res 466(8): 1959-1965.
- Breugem SJM, van Ooij B, Haverkamp D, Inger N Sierevelt, C Niek van Dijk (2014) No difference in anterior knee pain between a fixed and a mobile posterior stabilized total knee arthroplasty after 7.9 years. Knee Surg Sports Traumatol Arthrosc 22(3): 509-516.
- Pavlou G, Meyer C, Leonidou A, Mohammed As Sultany, Robert West (2011) Patellar resurfacing in total knee arthroplasty: Does design matter? A meta-analysis of 7075 cases. J Bone Joint Surg Am 93: 1301-1309.
- Metsna V, Vorobjov S and Martson A (2014) Prevalence of anterior knee pain among patients following total knee arthroplasty with nonreplaced patella: a retrospective study of 1778 knees. Medicina 50(2): 82-96.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.