Short Communication 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Percutaneous Transluminal Caval-flow Regulation PTCR®: An Emerging Therapy to Reduce Total Cardiac Burden in Heart Failure Patients
*Corresponding author: José E Herrera, Asociación Cardiológica de Occidente, ASCARDIO, Universidad Central ‘Lisandro Alvarado’ (UCLA), Barquisimeto 3001, Venezuela.
Received: July 07, 2023; Published: July 26, 2023
DOI: 10.34297/AJBSR.2023.19.002622
Abstract
In this communication we want to make the scientific community aware of a new procedure called Percutaneous Transluminal Caval flow Regulation PTCR as an emerging therapy to reduce hypervolemia present in 90% of cases of AHF acute heart failure in the emergency department, this therapy Emergent is capable of producing a reduction in hypervolemia that leads to a reduction in preload, filling pressures, LV diastolic and systolic diameters, producing remodeling reversal and total cardiac load. Also producing a marked reduction in pulmonary congestion, this procedure is minimally invasive and so far no contralateral effects have been reported.
Keywords: Percutaneous Transluminal Caval-flow Regulation, Inferior Vena Cava Heart Failure, Catheter Balloon.Medical Devices, Cardiac Output, Ejection Fraction
List of Abbreviations: HFrEF: Heart failure with Reduced Ejection Fraction; PTCR: Percutaneous Transluminal Caval Flow Regulation; HV: Hypervolemia; TCB: Total Cardiac Burden; ED: Expiration Diameter; ID: Inspiration diameter; IVC: Inferior Vena Cava; CO: Cardiac Output; AHF: Acute Heart Failure; HF: Heart Failure; EF: Ejection Fraction
Introduction
Percutaneous Transluminal Caval-flow Regulation (PTCR) is an emerging alternative therapy to treat patients with acute heart failure (AHF). AHF represents the first cause of hospitalization in elderly persons and is the main determinant of the huge healthcare expenditure related to heart failure (HF). Despite therapeutic advances, the prognosis of AHF is poor, with in-hospital mortality ranging from 4% to 7%, 60 to 90-day mortality. Hypervolemia was demonstrated in 90% of the AHF patients presenting to the emergency department [1].
PTCR is inspired by our echocardiographic discovery of a spontaneous natural phenomenon produced by a fibrocalcic formation of the right cavo-diaphragmatic junction called Dynamic Inferior Vena Cava Stenosis (DIVCS) [2], capable of reducing the total cardiac burden and producing benefits of echocardiographic parameters such as diastolic volume. and LV end systolic diameter, LV diastolic and systolic diameter, left atrial AP diameter as well as surrogate echocardiographic parameters of filling pressure (E/A Ratio), with a slight increase in ejection fraction from 32% up to 40.6%.
In view of these excellent results observed in the spontaneous natural model represented by the DIVCS, we decided to replicate this natural phenomenon with an artificial model capable of reducing the total cardiac load, so a balloon catheter medical device has been designed to produce cyclic occlusions of the Inferior Vena Cava (IVC) supported by the phases of respiration, thus having subtotal occlusion during expiration and total occlusion during inspiration, producing an intermittent regulation of venous return or preload from the IVC to the right atrium. This PTCR procedure is minimally invasive. It is performed through the insertion of the balloon catheter via the femoral vein. This catheter is advanced to the IVC guided by echocardiogram or fluoroscopy to be placed prior to drainage of the hepatic vein. At this point, the balloon is inflated up to 70% to 80% of the diameter of the IVC in expiration, which has to be previously evaluated by echocardiography. Then inspiratory collapse (20 to 30% average) of the IVC diameter produces total occlusion during inspiration and a partial or subtotal occlusion during expiration of the IVC, thereby regulating caval flow in an intermittent manner.
This innovative procedure is aimed at regulating the hypervolemia present in the IVC, normalizing venous return, preload, intracardiac pressures, biventricular diastolic and systolic diameters, diastolic and systolic volume, thus, obtaining reduction of total cardiac burden (TCB) and producing a reversal of ventricular remodelling. In this manner the heart returns close to its original design, with improvement in ejection fraction (EF) and maintaining cardiac output. This information can be observed in our publication “Firstin- human experience of preload regulation with percutaneous transluminal caval flow regulation in heart failure with reduced ejection fraction patients” [3].
According to the American Heart Association there are approximately 6.2 million heart failure (HF) patients in the US alone [4], 64.3 worldwide in 2018, HF was mentioned in 379,800 death certificates (13.4%) [4]. HF costs the nation an estimated $30.7 billion in 2012 [4]. This total includes the cost of health care services, medications to treat HF, and lost workdays. Nearly 1 in 4 HF patients are readmitted within 30 days of discharge and approximately half are readmitted within 67. These patients have to go to the hospital every 90 days for 4-5-day decongestant treatment with the use of potent diuretics. 25% of the 6.2 million HF patients in the US represent 1.7 million patients who are our target patients for use of our procedure Transluminal Caval flow Regulation PTCR and Catheter Medical Device (Figure 1).
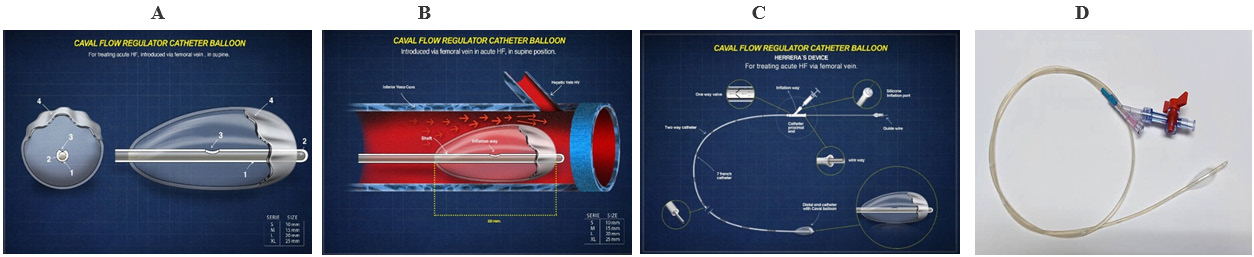
Figure 1: Caval Flow Regulating Catheter Balloon. A: Caval balloon en short and longitudinal axis view. B: Caval balloon inside IVC before hepatic vein drainage. C: Catheter Balloon schematic view for femoral vein insertion. D: Catheter balloon prototype for use in acute Heart Failure.
This great reality shown with its statistics, creates a rather bleak picture because until now current therapies have not been able to, significantly, reduce hospital readmissions of patients with acute or chronic decompensated HF nor treat pulmonary congestion, which endangers patient’s life.

Figure 2: Caval Flow Regulation by Spontaneous Natural Phenomenon (Dynamic Stenosis of IVC Or IVC Valve) and Its Flow. A: Caval Flow Regulation By Spontaneous Natural Phenomenon. B: IVC flow regulation and its flow.
See video CaseHP
With this review of our article where we show our experience in humans using our procedure, we want to make it well established that, with the results obtained, our procedure and device represent a new alternative to treat HF patients with great advantages over current therapies. This is due to the fact that it is a safe temporary therapy, without collateral effects, and very effective in achieving hemodynamic and echocardiographic benefits. Thus, meaning a true innovation, capable of changing the paradigm of HF treatment with great benefits for patients and great savings for the state health service (Table) (Figure 2).
How The PTCR Procedure Is Performed
The methodology to implement the PTCR procedure consists of a series of rules that guarantee the function of regulating venous return, preload and therefore the total cardiac burden (Figure 2).
The diameter of the caval balloon is related to the anteroposterior diameter of the IVC at the time of inspiratory collapse. For example, if the expiratory diameter is 18 mm and the collapse is 30% (5,4 mm), it would suffice to subtract 18mm (diameter in expiration) - 5,4mm (diameter in inspiration) = Balloon size must be inflated until reaching 12,6 mm, the balloon is designed to remain free floating in the IVC lumen and so on for any other case.
For a better understanding, please see videos: How the Caval Flow Regulator Balloon works and Percutaneous Transluminal Caval Flow Regulation.
Conclusion
PTCR is a new alternative to reduce total cardiac burden and treat patients with heart failure, reducing intracardiac pressures, biventricular volumes, ventricular diameters, ventricular filling pressure and ventricular wall stress, resulting in clinical benefits such as reduced congestion, lung and improving cardiac output, without side effects. It has demonstrated to date to be a safe and effective procedure.
More studies are needed with a larger number of patients to confirm our initial observation in our study.
References
- Constanzo MR, Guglin ME, Saltzberg MT, Jessup ML, Bart BA, et al. (2007) Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J Am Coll Cardiol 49(6): 675-683.
- Herrera JE, Herrera JA, Marques JE, Mendoza I (2011) A novel method to reduce preload mechanically in patients with congestive heart failure, the dynamic restriction of flow in the inferior vena cava. Eur J Heart Fail Supplements 10: 4.
- José Herrera, José A Octavio, Juan A Marqués, Robert A Levine, Igor F Palacios, et al. (2022) First-in-human experience of preload regulation with percutaneous transluminal caval flow regulation in heart failure with reduced ejection fraction patients. Journal ESC Heart Failure 9(2): 1118-1126.
- (2017) American Heart Association’s statement. Heart failure is projected to increase dramatically, according to new statistics Published.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.