Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
The Use of Telemedicine in the Care of Pregnant Women with Gestational Diabetes
*Corresponding author: Dr Katarzyna Cyganek, Department of Metabolic Diseases, Jagiellonian University Medical College, Jakubowskiego 2 St, 30-688 Kraków, Poland.
Received: July 11, 2023; Published: July 19, 2023
DOI: 10.34297/AJBSR.2023.19.002611
Abstract
Gestational diabetes mellitus (GDM) is a relatively common complication of pregnancy. It is crucial that GDM is correctly diagnosed and managed, as it is associated with a considerable number of adverse events for the mother, and also adverse perinatal outcomes. In pregnancy it is necessary to initiate the treatment as quickly as possible and maintain glycemia throughout pregnancy at the level of normoglycemia as in a healthy pregnant woman.
Currently, modern technologies facilitate the implementation of diabetes education and the intensification of therapy. Used in diabetes care, they relate to the possibility of insulin administration: injectors - smart pens with dose memory, insulin pumps and systems for glucose monitoring: modern glucometers, continuous glucose monitoring systems connected with mobile applications and the possibility of exporting data to the cloud. The mobile applications from patients’ smartphones can serve as an interface that transfers blood glucose monitoring data between patient and healthcare providers.
The current telemedicine mainly consists of teleconsultation, tele-diagnose, tele-education, tele-medical care and uses video conferencing, smartphones, wireless tools and other forms of tele communications technology. The SARS-CoV-2 virus pandemic has shown how many opportunities remote care offers, especially in monitoring chronic diseases.
Due to the need for education, frequent and quick modification of treatment, many studies have been conducted to assess the possibilities of using modern technologies in virtual care of women with GDM. Numerous studies have shown that virtual diabetic care during pregnancy can help manage hyperglycemia in pregnancy and improve perinatal outcomes for newborn and mother’s health.
Keywords: Telemedicine, M-Health, Gestational diabetes mellitus, Pregnancy
Introduction
Diabetes mellitus is one of the most common chronic diseases in the world [1]. The number of diabetics continues to grow, and this applies to both type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) patients [2], although almost 90% of all diagnoses of the disease are type 2 diabetes. As a consequence of chronic hyperglycemia, various organs are damaged, and the late complications of diabetes mellitus: micro- and macroangiopathy develop [3]. Diabetes mellitus is progressive, which makes it necessary to constantly intensify the therapy [4]. According to the current American and European diabetes recommendations, including the Polish Diabetes Association (PDA), the treatment of diabetes should take into account not only disorders related to hyperglycemia, but also the presence of additional diseases, especially cardiovascular diseases, overweight and obesity, kidney function, the patient’s age, previous eating habits and the patient’s financial capacity [5,6]. Diabetes is not only the patient and his treatment, but also the costs associated with the use of drugs, hospitalization, absenteeism, disability pension, treatment of disease complications. Economically, the disease affects the whole of society. About 3 million people in Poland suffer from diabetes, of which 1 million do not know about the disease [7].
In the treatment of diabetes, it is important to maintain the target blood glucose values determined individually for the patient [5,6]. However, due to the progressive nature of the disease, it is difficult to maintain these glycemic targets in the long term, and despite medical advances, still only 56% achieve the target glycated hemoglobin - HbA1c [8,9]. Diabetes treatment begins with modification of the patient’s diet and lifestyle, and implementation of metformin as the first-line drug [5,6]. As part of the intensification, further oral drugs or drugs administered in injection, such as GLP-1 analogues or insulin therapy, are added [5,6]. According to diabetes recommendations, treatment should be intensified every 3 months. However, despite the recommendations, a certain therapeutic inertia (delay) in the intensification of treatment is observed, which is associated with difficulties both on the part of the patient and the care team.
There are different types of diabetes among pregnant women. When diabetes occurred in a woman before pregnancy, it is pre-pregnancy diabetes: it may be type 1 (autoimmune), type 2 (insulin-resistant) diabetes, monogenic diabetes (MODY, maturity onset diabetes of the youth), or secondary diabetes (e.g. after pancreatic damage for various reasons). On the other hand, if carbohydrate metabolism disorders appear for the first-time during pregnancy, then hyperglycemia in pregnancy (HIP) is diagnosed. Different forms of hyperglycemia are diagnosed depending on the level of glycaemia during pregnancy: diabetes in pregnancy (DIP) is a disorder in which fasting or random blood glucose levels are as high as in newly diagnosed diabetes and usually develops in early pregnancy. If the first diagnosis of glucose intolerance is made during the second or third trimester of pregnancy, and type 1 or type 2 diabetes not pre-existed, then a diagnosis of gestational diabetes mellitus (GDM) is made [2,3]. Gestational diabetes mellitus is a relatively common complication of pregnancy, the International Diabetes Federation estimates suggest that globally hyperglycaemia in pregnancy affects about 15.8% of live births, with around 84% of these being due to gestational diabetes mellitus [2,10]. GDM is transient, most often diagnosed in the middle of pregnancy and usually resolves after delivery [2,3,11]. It is crucial that gestational diabetes is correctly diagnosed and managed, as it is associated with a considerable number of adverse events for the mother, and also adverse perinatal outcomes. In pregnancy, in addition to the quick diagnosis of carbohydrate metabolism disorders, it is also necessary to initiate the treatment as quickly as possible and maintain glycemia throughout pregnancy at the level of normoglycemia as in a healthy pregnant woman. Usually, the treatment of gestational diabetes concerns about 12-16 weeks and during this period, therapy should be intensified in order to maintain normal glucose levels. Such rapid intensification of treatment is difficult and requires the earliest possible education on the diabetic diet, self-monitoring and glycemic goals, and frequent medical check-ups [6].
Currently, modern technologies facilitate the implementation of diabetes education and the intensification of therapy. Modern technologies used in diabetes care relate to the possibility of insulin administration: injectors - smart pens with dose memory, insulin pumps and systems for glucose monitoring - modern glucometers, continuous glucose monitoring systems connected with mobile applications and the possibility of exporting data to the cloud [12]. The mobile applications from patients’ smartphones can serve as an interface that transfers blood glucose monitoring data between patient and healthcare providers. The technology has also influenced screening capabilities: these are tools to assess the risk of diabetes, the presence of diabetes complications: such as eye fundus photography, foot temperature measuring devices and risk assessment of the development or deterioration of diabetic feet, pressure recorders, measurements of body weight, temperature, heart rate and connecting all these devices through mobile applications with the data cloud. This makes it possible for the healthcare team to analyze various patient data in real time and improve the patient’s metabolic control.
Telemedicine (also known as telehealth) is defined as the provision of health services at a distance using a range of technologies and is a growing field nowadays [13] or according to the American Telemedicine Association it is the use of medical information exchanged from one site to another via electronic communications to improve a patient’s clinical health status [14]. Telemedicine application is now ubiquitous in modern society. The current telemedicine mainly consists of:
a) Teleconsultation,
b) Tele-diagnose,
c) Tele-education,
d) Tele-medical care
We can use video conferencing, smartphones, wireless tools and other forms of tele-communications technology. We now know that telemedicine and digital diabetes care has a positive impact on the experiences of patients and health care professionals (HCP). Digital health-related diabetes prevention and treatment saves the time needed to travel to the HCP providers, shortens the waiting time for an appointment, offers unlimited time assistance and greater availability of care, greater patient convenience and comfort, timely diagnosis, cost savings, and the greater frequency of virtual visits also enables a closer relationship between the patient and the HCP [15,16]. At the same time, the use of technology and remote monitoring of patients causes greater involvement of patients in controlling their disease, learning and avoiding errors in the case of chronic disease.
The main problems to the development of telemedicine are problems at the organizational level, both on the part of the patient and the time care, such as difficulties related to the lack of competence in the use of digital technologies among patients and doctors. Another group of obstacles relates to the issues of cost recovery, safety and liability. The security of the connection between different patient databases, systems, platforms and information exchange, and the issues of trust between the patient and the physician, when the latter must rely on information provided by patients, further complicate the advancement of telemedicine. And finally, the inability to perform a complete physical examination and the risk of overlooking disturbing symptoms [15-21]. However, despite these enumerated drawbacks, the effectiveness of telemedicine has now been proven in the care of patients with type 1 diabetes, type 2 diabetes, and in the care of pregnant women. This effectiveness was manifested in the improvement of metabolic control of patients with diabetes - especially in the reduction of the level of glycated hemoglobin (HbA1c), body weight, improvement of lipid profile, blood pressure, quality of life of patients, less hypoglycaemia or hospitalization [22-24]. Retrospective analysis by Whaley et al. showed that remote digital diabetes management program also had a financial impact and was linked to lower medical spending at 1 year [23].
Remote - virtual visit includes:
1. Assessment of well-being: the patient’s complaints
2. Patient health assessment: examination elements:
i. Body weight / BMI
ii. Blood pressure
iii. Heart action, rhythm of heart
iv. Temperature
v. Blood glucose, HbA1c, episodes of hypo- and hyperglycaemia, Time in Range (TIR), Time Below Rage (TBR), Time Above Range (TAR)
3. Reading data from devices/mobile applications/cloud
4. Effective analysis of data records:
i. Insulin administration / insertion
ii. Drug / insulin / base-bolus doses
iii. Diet, CHO count (calculation of carbohydrate exchangers), calories, number of meals
iv. Activity - quantity, intensity
5. Clinical recommendations
6. e-prescription, e-orders
However, the SARS-CoV-2 virus pandemic has shown how many opportunities remote care offers, especially in monitoring chronic diseases. The potential benefits, telehealth and m-health have great promise in transforming diabetes care, education and group support. Currently, most of the guidelines are trying to combine the technologies and possibilities of telemedicine with in-person visits and recommended use of digital diabetes technologies and telehealth protocols within a digital/virtual diabetes clinic [6,15,16,25]. Patients with diabetes are very eager to use modern technologies. In Poland however, many of those solutions, especially insulin pumps and continuous glucose monitoring systems, are expensive. Only the children and young adults with type 1 diabetes are eligible for reimbursements of some of these devices. Most of the diabetic patients use free mobile applications regardless of the type of disease and treatment. Mobile applications supporting insulin therapy enable standardized calculation of insulin dose, meal bolus calculator, calculation of carbohydrate exchangers (CHO counting), diet caloric value, and control of physical activity, improve rate of medication adherence. Also, applications related to the modification of lifestyle regarding education allow regular phone calls and video calls with the educator/nurse/dietitian/ psychologist, virtual education, support for patient exercises and training, the possibility of virtual exercise sessions [25].
The analysis of the research showed that the most popular diabetes- related applications are self-care, among patients with T1DM more than half (52.2%, n = 549) used the application, and about 1/3 of patients with T2DM (33.3%, n = 210). The most frequently used applications are mySugr and applications related to continuous glucose monitoring systems (CGM) - Dexcom, Freestyle Libre, Xdrip + [22,26].
As mentioned earlier, gestational diabetes is the most common metabolic disorder that occurs during pregnancy [2,10]. According to earlier diagnosis of GDM during gestation it is important to maintain good glucose blood level control to improve maternal and fetal short and long-term outcomes [11,27,28]. In Poland, the fasting venous blood glucose level is already obligatorily monitored during the first visit to the obstetricians. The oral glucose tolerance test is also mandatory [6]. Due to the need for education, frequent and quick modification of treatment, many studies have been conducted to assess the possibilities of using modern technologies in virtual care of women with gestational diabetes. Numerous scientific studies have shown that virtual diabetic care during pregnancy can help manage hyperglycemia in pregnancy and improve perinatal outcomes for newborn and mother’s health [24,29-31]. Pregnant women are increasingly using mobile APP to access information, monitor fetal development, track individual health indicators, diet, exercise [32,33]. The use of mobile phone-based health behaviour interventions in pregnancy demonstrates some correlation with positive beliefs, behaviours, and health outcomes [33,34]. In meta- analysis published in 2016 by Ming, et al., [29] identified 7 trials and demonstrated a modest but statistically significant improvement in HbA1c associated with the use of a telemedicine technology. The mean HbA1c level of women using telemedicine was 5.33% (SD 0.70) compared with 5.45% (SD 0.58) in the standard care group (mean difference of - 0.12% (95% CI - 0.23% to - 0.02%). When this comparison was limited to women with gestational diabetes mellitus (GDM) only, the mean HbA1c level of women using telemedicine was 5.22% (SD 0.70) compared with 5.37% (SD 0.61) in the standard care group (mean difference - 0.14% (95% CI - 0.25% to - 0.04%). There were no differences in other maternal and neonatal outcomes reported. In this 6-year-old analysis, the data were insufficient to demonstrate a clinical advantage of telemedicine technology in terms of improved neonatal outcomes superior to standard care for women with diabetes in pregnancy; however, there was no evidence of harm. In the newest meta-analysis published by Xie, et al., [35], a total of 32 RCTs were identified, with a total of 5108 patients. The meta-analysis showed that telemedicine group had significant improvements in controlling glycated haemoglobin (HbA1c) [mean difference (MD) = - 0.70, P < 0.01], fasting blood glucose (FBG) (MD = -0.52, P < 0.01) and 2-h postprandial blood glucose (2hBG) (MD = -1.03, P = 0.01) compared to the corresponding parameters in the standard care group. In the telemedicine group, lower incidences of caesarean section [relative risk (RR) = 0.82, P = 0.02], neonatal hypoglycaemia (RR = 0.67, P < 0.01), premature rupture of membranes (RR = 0.61, P < 0.01), macrosomia (RR = 0.49,P < 0.01), pregnancy-induced hypertension or preeclampsia (RR = 0.48, P < 0.01), preterm birth (RR = 0.27, P < 0.01), neonatal asphyxia (RR = 0.17, P < 0.01), and polyhydramnios (RR = 0.16, P < 0.01) were found. The researchers concluded that compared to standard care, telemedicine interventions contributed to beneficial impacts on the glycaemic level, and some maternal and neonatal/foetal complications in patients with gestational diabetes mellitus compared to the effects of standard care. Telemedicine can decrease the glycaemic levels of patients with GDM more effectively and reduce the risk of maternal and neonatal/foetal complications. The application of telemedicine in the clinical management of gestational diabetes mellitus may be advisable [35].
In a recently published systematic review a total of 27 articles met defined inclusion criteria. m-health interventions were implemented by smartphone, without referring to its type, in 26% (7/27) of selected studies, short message service (SMS) in 14.9% (4/27), mobile-based applications in 33.3% (9/27), telemedicine-based on smartphones in 18.5% (5/27), and SMS reminder system in 7.1% (2/27). Most of the included studies (n=23) supported the effectiveness of m-health interventions on GDM management and 14.3% (n=4) reported no association between m-health interventions and pregnancy outcomes. Based on these findings, m-health interventions could enhance GDM patients’ pregnancy outcomes. A majority of the included studies suggested positive outcomes. m-health can be one of the most prominent technologies for the management of GDM [36].
Furthermore, in a small randomized trial a total of 124 patients with gestational diabetes mellitus (GDM) were selected and patients were randomly divided into two groups: the control, received standard outpatient treatment and examined m-health group received a nurse’s online guidance both through a mobile medical App installed on their phone and through regular offline clinical treatment. The authors showed that mobile health intervention management of gestational diabetes mellitus improves patients’ compliance and blood glucose control, and reduces weight gain, thereby reducing the rates of complications in both pregnant women and foetuses during delivery during pregnancy [24]. Another randomized controlled trial has provided further evidence of the effect of digital virtual care and telemonitoring, which significantly decreased medical visits and direct costs in GDM women without compromising pregnancy outcomes, quality of care, or patient satisfaction. Digital diabetes care in women with GDM was shown to be cost-effective despite placing an additional burden on nursing time [30].
Also, observational studies bring forward evidence of a positive effect of a real-life e-health lifestyle intervention on the improvement of glycemic control and the improvement of the comfort of patients with GDM thanks to the use of opportunities related to virtual care. In a small observational study the authors showed that e-health care of women with GDM may provide an effective new avenue to enhance multidisciplinary care in the face of COVID-19 disruptions and challenges to traditional care pathways [31].
In the era of the pandemic, it was possible to observe an improvement in the care of patients with diabetes. The option of using telehealth in antenatal care has been brought sharply into focus with the coronavirus disease 2019 (COVID-19) pandemic. This advice has led to recommendations to limit face-to-face consultations and for rapid implementation of remote access to antenatal care [6,37-40]. Thanks to telemedicine and the use of mobile applications, we did not notice any deterioration in the care of pregnant women with diabetes. Thanks to Bluetooth technology, modern glucometers are connected to a mobile application and have the ability to send each blood glucose value measured by the patient from the meter to the patient’s smartphone, also mobile applications are used to educate the patient and increase his responsibility for his health self-care options. In Poland we could use several glucometers with mobile applications: Accu-Chek Instant and mySugr application, Contour Plus One or Elite and application Contour Plus One, One Touch Select and One Touch Reveal, Glucomax Connect and SweetPregna, Abra Smart and Istel Health. The patient’s blood glucose data from mobile applications can be sent directly to the physician in the form of a report and to the data cloud and evaluated in real time by the therapeutic team. If the patient in the mobile application marks the amount of insulin taken and the number of carbohydrate exchangers (CHO), data will be also available for the physician.
The education of patients in a virtual environment not only affords a direct exchange of information, but also the ability to employ additional learning tools, such as interactive diagrams, visual aids, and gaming. Some applications have additional options, such as a meal bolus calculator - calculation of insulin dose after meal/correction, the ability to estimate (estimate) the level of glycated hemoglobin, it is illustrative information and at the same time a motivating factor for the patient, the ability to search for the necessary information related to diabetes and strengthening the patient’s motivation and the patient’s participation in self-care. Also, the application enables the diabetic patient to collect data, report and actively modify diabetes therapy. As part of education, the therapeutic team of the Diabetes Clinic should train the patient on the necessary terms and data interpretation.
We have recently published a retrospective analysis on diabetes care and pregnancy outcomes in GDM during the first wave of the COVID-19 pandemic in Poland [41]. Both before and during the pandemic, education about the diet, the release of the glucometer and the training how to use and how to connect the meter with telephone application and how to export data from application to health care professionals, education about glycemic self-control, and finally the release of the insulin pen and teaching the technique of insulin administration were performed personally by a dietitian and a nurse. Usually in our Department we use Contour Plus glucometer with related app, Accu-chek Instant and MySugr app or an application SweetPregna. Online teleconsultations in the form of a telephone conversation became widely utilized since the beginning of pandemic. We did not observed a negative impact on pregnancy outcomes in GDM women, excepting higher incidence of prolonged labour and a decrease in the frequency of preeclampsia both observed among mothers giving birth during the COVID-19 pandemic [41].
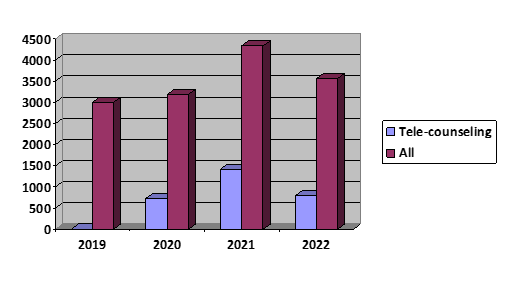
In our Out-Patients Diabetes Clinic for Pregnant Women with Diabetes, the part of Department of Metabolic Diseases, Jagiellonian University Medical College, we take medical care for women with pre-diabetes planning pregnancy and women with hyperglycemia during pregnancy, mostly with GDM. In the pre-COVID era, there were no teleconsultations. During the pandemic, the payer in public medical care, the National Health Fund, agreed to cover the costs of teleconsultation Over the last 3 years, we have observed a gradual increase in medical advice in the form of tele-advice. In Figure 1 we show how the number of tele-counselling in the Diabetes Clinic for Pregnant Women increased in 2019-2022: from 0% in 2019 years to 22,8% in 2020 yrs; 32,8% in 2021 yrs and 22,5% in 2022yrs.
Based on our own experience and recommendations of Polish Diabetes Association, we are still using the possibilities related to telemedicine. In our Department, we have developed our own model of the structure of care for pregnant women with diabetes. The first visit is always done in person. On this first visit, the patient receives both medical and dietary advice as well as nursing education in the use of self-monitoring and glycemic goals. Patient receives educational materials in paper and online form, glucometer, and connection to the appropriate application. The next visit, mostly 1 or 2 weeks later, is also personal, the next visit every 2 to 4 weeks, usually carried out virtually. The penultimate visit is carried out in person, then the patient is trained in postpartum management and the need to report 10-12 weeks postpartum in order to perform the 75g Oral Glucose Tolerance Test (75g OGTT) and verify carbohydrate disorders.
In conclusion, caring for patients with diabetes, regardless of the type, the effectiveness of telemedicine systems in improving glycemic control and self-care, the adherence to dietary recommendations, the number of glycemic measurements or physical activity has been proven, as well as greater patient participation in the treatment of a chronic disease - taking the patient’s self-care and responsibility for the therapy [22]. Mobile applications also enable greater cooperation between the patient and the therapeutic team and education in the field of various aspects of the patient’s life, self-control, diets, physical activity [15] (Table 1).
Summary - key aspects of virtual visit in pregnancy:
a) Data on well-being, pregnancy, medications used
b) Weight gain in pregnancy and the implementation of dietary recommendations
c) Reliable glycemic report - data analysis (CareLink, GlucoContro, Clarity, LibreView, IstelCare, date from mobile app: mySugr, Contour Plus, IstelHealth and others)
d) Current treatment (diet / insulin doses)
e) Make sure the patient has understood the recommendations (repeat)
f) Schedule another pregnancy check-up
g) Preparation for childbirth - teach about the procedure before and after childbirth
Acknowledgment
None.
Funding
No funding to declare.
Disclosures
None.
Conflict of Interest
None declared.
References
- Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF (2010) Projection of the year 2050 burden of diabetes in the US adult population: dynamic modelling of incidence, mortality, and prediabetes prevalence. Pop Health Metr 8: 29.
- https://diabetesatlas.org
- Report of a WHO Consultation (1999) Definition, diagnosis and classification of diabetes mellitus and its complications. WHO, Geneva, Switzerland.
- Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA (2008) 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 359(15): 1577-1589.
- Davies MJ, Aroda VR, Collins BS, Gabbay RA, Green J, et al. (2023) Management of hyperglycaemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 45(11): 2753-2786.
- Polish Diabetes Association (2023) Guidelines on the management of diabetic patients. A position of Diabetes Poland. Curr Top Diabetes 3(1): 1-140.
- Czupryniak L, Grzeszczak W, Cukrzyca SK (2012) Ukryta pandemia. Sytuacja w Polsce. Edycja 2012. red. Czupryniak L., Grzeszczak W., Strojek K. Wyd. Novo Nordisk.
- Holman RR, Thorne KI, Farmer AJ, Davies MJ, Keenan JF, et al. (2007) Addition of biphasic, prandial, or basal insulin to oral therapy in type 2 diabetes. N Engl J Med 357: 1716-173.
- Holman RR, Farmer AJ, Davies MJ, Levy JC, Darbyshire JL, et al. (2009) Three-year efficacy of complex insulin regimens in type 2 diabetes. N Engl J Med 361(18): 1736-1747.
- Yuen L, Saeed P, Riaz M, Karuranga S, Divakar H, et al. (2019) Projections of the prevalence of hyperglycaemia in pregnancy in 2019 and beyond: Results from the International Diabetes Federation Diabetes Atlas, 9th Diabetes Res Clin Pract 157: 107841.
- Buchanan TA, Xiang AH, Page KA (2012) Gestational diabetes mellitus: risks and management during and after pregnancy. Nat Rev Endocrinol 8(11): 639-649.
- Aberer F, Hochfellner DA, Mader JK (2021) Application of Telemedicine in Diabetes Care: The Time is Now. Diabetes Ther 12(3): 629-639.
- Oh H, Rizo C, Enkin M, Jadad A (2005) What is eHealth: a systematic review of published definitions. J Med Internet Res 7(1): e1.
- https://www.healthit.gov/sites/default/files/telehealthguide_final_0.pdf
- Phillip M, Bergenstal RM, Close KL, Danne T, Garg SK, et al. (2021) The digital/virtual diabetes clinic: the future is now-recommendations from an international panel on diabetes digital technologies introduction. Diabetes Technol Ther 23(2): 146-154.
- Zulman DM, Verghese A (2021) Virtual Care, Telemedicine Visits, and Real Connection in the Era of COVID-19 Unforeseen Opportunity in the Face of Adversity. JAMA 325(5): 437-438.
- Patel SY, Rose S, Barnett ML, Huskamp HA, Uscher Pines L, et al. (2021) Community Factors Associated With Telemedicine Use During the COVID-19 Pandemic. JAMA Netw Open 4(5): e2110330.
- Shachar C, Gupta A, Katznelson G (2021) Modernizing Medical Licensure to Facilitate Telemedicine Delivery After the COVID-19 Pandemic. JAMA Health Forum 2(5): e210405.
- Cortez C, Mansour O, Qato DM, Stafford RS, Alexander G (2021) Changes in Short-term, Long-term, and Preventive Care Delivery in US Office-Based and Telemedicine Visits During the COVID-19 Pandemic. JAMA Health Forum 2(7): e211529.
- Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, et al. (2020) Trends in Outpatient Care Delivery and Telemedicine During the COVID-19 Pandemic in the US. JAMA Intern Med 181(3): 388-391.
- Lum E, Jimenez G, Huang Z, Thai L, Semwal M, et al. (2019) Decision Support and Alerts of Apps for Self-management of Blood Glucose for Type 2 Diabetes. JAMA 321(15): 1530-1532.
- Kebede M, Pischke CR (2019) Popular Diabetes Apps and the Impact of Diabetes App Use on Self-Care Behaviour: A Survey Among the Digital Community of Persons With Diabetes on Social Media. Front Endocrinol 10: 135.
- Whaley CM, Bollyky JB, Lu W, Painter S, Schneider J, et al. (2019) Reduced medical spending associated with increased use of a remote diabetes management program and lower mean blood glucose values. J Med Econ 22(9): 869-877.
- Guo H, Zhang Y, Li P, Zhou P, Chen LM, et al. (2019) Evaluating the effects of mobile health intervention on weight management, glycemic control and pregnancy outcomes in patients with gestational diabetes mellitus. J Endocrinol Invest 42(6): 709-714.
- Al-Badri M, Hamady O (2021) Diabetes clinic reinvented: will technology change the future of diabetes care? Ther Adv Endocrinol Metab 12: 1-10.
- Debong F, Mayer H, Kober J (2019) Real-world assessments of my Sugr mobile health app. Diabetes Technol Ther 12: S235-S240.
- Lim Sl, Ong KW, Johal J, Han CY, Yap QV, et al. (2021) Effect of a Smartphone App on Weight Change and Metabolic Outcomes in Asian Adults With Type 2 Diabetes A Randomized Clinical Trial. JAMA Network Open 4(6): e2112417.
- Cortez C, Mansour O, Qato DM, Stafford RS, Alexander C (2021) Changes in Short-term, Long-term, and Preventive Care Delivery in US Office-Based and Telemedicine Visits During the COVID-19 Pandemic. JAMA Health Forum 2(7): e211529.
- Ming WK, Mackillop LH, Farmer AJ, Loerup L, Bartlett K, et al. (2016) Telemedicine Technologies for Diabetes in Pregnancy: A Systematic Review and Meta-Analysis. J Med Internet Res 18(11): e290.
- Lemelin A, Pare´ G, Bernard S, Godbout A (2020) Demonstrated Cost-Effectiveness of a Telehomecare Program for Gestational Diabetes Mellitus Management. Diabetes Technol Ther 22(3): 195-202.
- Varnfield M, Redd C, Stoney RM, Higgins L, Scolari N, et al. (2021) MvTHer, an mHealth System to Support Women with Gestational Diabetes Mellitus: Feasibility and Acceptability Study. Diabetes Technol Ther 23(5): 358-366.
- Daly LM, Horey D, Middleton PF, Boyle FM, Flenady V (2018) The Effect of Mobile App Interventions on Influencing Healthy Maternal Behavior and Improving Perinatal Health Outcomes: Systematic Review. JMIR Mhealth Uhealth 6(8): e10012.
- Hussain T, Smith P, Yee LM (2020) Mobile Phone-Based Behavioral Interventions in Pregnancy to Promote Maternal and Fetal Health in High-Income Countries: Systematic Review. JMIR Mhealth Uhealth. 8(5): e15111.
- Fantinelli S, Marchetti D, Verrocchio MC, Franzago M, Fulcheri M, et al. (2019) Assessment of Psychological Dimensions in Telemedicine Care for Gestational Diabetes Mellitus: A Systematic Review of Qualitative and Quantitative Studies. Front Psychol 10: 153.
- Xie W, Dai P, Qin Y, Wu M, Yang B, (2020) Effectiveness of telemedicine for pregnant women with gestational diabetes mellitus: an updated meta-analysis of 32 randomized controlled trials with trial sequential analysis. BMC Pregnancy and Childbirth 20(1): 198.
- Zahmatkeshan M, Zakerabasali S, Farjam M, Gholampour Y, Seraji M, et al. (2021) The use of mobile health interventions for gestational diabetes mellitus: a descriptive literature review. J Med Life 14(2): 131-141.
- ADA (2021) Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2021. American Diabetes Association. Diabetes Care 44(Suppl 1): S15-S33.
- Torlone E, Sculli MA, Bonomo M, Benedetto AD, Cianni GD, et al. (2020) Recommendations and management of hyperglycaemia in pregnancy during COVID-19 pandemic in Italy. Diabetes Res Clin Pract 166: 108345.
- Peahl AF, Smith RD, Moniz MH (2020) Prenatal care redesign: creating flexible maternity care models through virtual care. Am J Obstet Gynecol 223(3): 389.e1-389.e10.
- Aziz A, Zork N, Aubey JJ, Baptiste CD, D'Alton ME, et al. (2020) Telehealth for High-Risk Pregnancies in the Setting of the COVID-19 Pandemic. Am J Perinatol 37(8): 800-808.
- Wilk M, Surowiec P, Matejko B, Wróbel A, Zięba Parkitny J, et al. Diabetes Management Delivery and Pregnancy Outcomes in Women with Gestational Diabetes Mellitus during the First Wave of the 2020 COVID-19 Pandemic: A Single-Reference Center Report. J Diabetes Res 2021: 5515902.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.