Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Thrombotic Thrombocytopenic Purpura: Illustrative Case
*Corresponding author: José Bohórquez-Rivero, University of Sinu-Cartagena Sectional.
Received: July 12, 2023; Published: July 19, 2023
DOI: 10.34297/AJBSR.2023.19.002607
Abstract
Thrombotic thrombocytopenic purpura is a disease that belongs to the group of thrombotic microangiopathies together with hemolytic uremic syndrome, atypical hemolytic uremic syndrome and microangiopathies of pregnancy. This pathology is characterized by the occurrence of microangiopathic hemolytic anemia, severe thrombocytopenia and organ ischemia related to disseminated platelet-rich microvascular thrombi. It is mainly caused by deficiency or malfunction of the ADAMTS13 protein (a disintegrin and metalloprotease). We illustrate a case of thrombotic thrombocytopenic purpura with a brief review of the literature.
Keywords: Thrombotic thrombocytopenic purpura, Microangiopathic, Anemia hemolytic anemia, ADAMTS13 protein (MeSH)
Introduction
Thrombotic Thrombocytopenic Purpura (TTP) was first described by the physician Eli Moschcowitz in 1921. It is a disease that is part of the Thrombotic Microangiopathies (TMA) along with hemolytic uremic syndrome, atypical hemolytic uremic syndrome and microangiopathies of pregnancy. TTP is characterized by occurrence of Microangiopathic Hemolytic Anemia (MAHA), severe thrombocytopenia and organ ischemia related to disseminated platelet-rich microvascular thrombi. It is primarily caused by deficiency or malfunction of the ADAMTS13 protein (a disintegrin and metalloprotease). The TTP has two spectrums of presentation, it can be acquired due to inhibition by autoantibodies or inherited due to inherited mutations in ADAMTS13.
It is a rare hematologic entity. The incidence of acquired TTP is approximately 3 cases per million adults per year, according to data from the Oklahoma TTP-HUS Registry. Acquired TTP is very rare in children under 18 years of age and is estimated to present in approximately 1 out of 10 million per year. Therefore, in children, the possibility of hereditary rather than acquired TTP should be considered, in contrast to adults, where acquired TTP is approximately 30 times more common than the hereditary TTP [1-3]. At the level of Colombia, there is no information available regarding its epidemiology, the only data on the disease are obtained through case reports [4,5]. We communicate a case of this interesting pathology.
Presentation of the Case
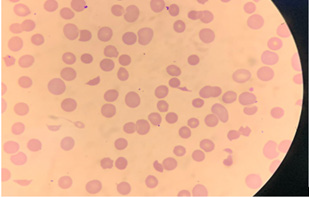
A 44-year-old male with a history of non-Hodking’s lymphoma treated in 2012 in remission, presented to the emergency department with a clinical picture of 7 days of evolution characterized by pulsatile headache of insidious onset, frontotemporal location, 6/10 on the analogue pain scale, asthenia, adynamia and paresthesia in the lower limbs. Physical examination evidenced Systolic Blood Pressure (SBP) of 142mmHg, Diastolic Arterial Pressure (DBP) of 89mmHg, Mean Arterial Pressure (MAP) of 102mmHg, Heart Rate (HR) of 106 beats/minute, Respiratory Rate (RF) of 17 breaths/ minute, oxygen saturation (SaO2) of 98% and Temperature (T) of 37.5℃. The patient was conscious, oriented in time, space, and person, with Glasgow 15/15, with no findings of purpura or petechiae. In the admission paraclinical findings, the hemoglobin of 7.5g/dL of macrocytic, hypochromic characteristic was striking (reticulocytes 11.4%, reticulocyte production index of 2), platelets at 27,000 per mm3, hyperbilirubinemia at the expense of indirect (BT:3.0mg/ dL, BI:2.5mg/dL, BD:0.5mg/dL), elevated lactate dehydrogenase (1139IU/L), with negative direct antiglobulin test, serum creatinine of 0.8mg/dL and INR at 1. The peripheral blood smear showed macrocytosis, marked polychromatophilia, spherocytes, basophilic stippling, presence of schistocytes in more than 5%, white series with neutrophil predominance without morphological alterations and severe thrombocytopenia (Figure 1). The Elisa test for HIV third generation was negative.
These findings were compatible with MAHA with a PLASMIC score of 6 points for a high probability of suffering from a deficiency of ADAMTS13. In view of this, plasmapheresis was initiated urgently, and glucocorticoid methylprednisolone was initiated, with a torpid evolution due to the development of atrial fibrillation, altered state of consciousness, pneumonia associated with health care with the need for prolonged mechanical ventilation and the need for tracheostomy. The diagnosis was confirmed days after initiation of treatment, with an ADAMTS13 activity of 0.2%. The patient was finally discharged from home hospitalization care.
Discussion
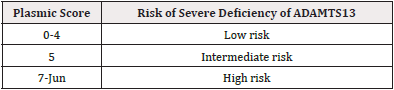
The diagnosis of this pathology should be suspected when MAHA (hemoglobin almost always<10 g/dL) and severe thrombocytopenia (platelet count almost always<30,000/microliter) are present, with or without symptoms of organ affectation and without other clinically apparent etiology [6]. At the time of presumed diagnosis, the PLASMIC SCORE is important because the measurement of ADAMS13 is not always available in many hospitals, it depends on the background in which the patient is found.
The PLASMIC SCORE was designed to predict the pre-test probability of the activity of ADAMTS13 ≤10%, it consists of 7 items (see Tables 1 and 2), the higher the score, the greater the possibility of presenting deficiency of that enzyme. The studies suggest that all patients with a PLASMIC score of 5 or more should be treated empirically for TTP unless there is an obvious alternative explanation for the individual’s clinical presentation. The diagnosis is confirmed by measurement of ADAMTS13, which should be less than 10%, however levels of ≥10% do not discard the possibility of TTP in individuals with a high suspicion for the diagnosis [1,6-9] (Tables 1,2). With respect to treatment, it should be initiated urgently, where the first line will be plasmapheresis and glucocorticoids. In refractory cases, the use of rituximab is indicated [6,10-12].
Declaration of Funding Sources
The authors declare that this research was conducted with the authors’ own support.
Ethical Considerations
For the realization of this case, informed consent was obtained from the patient and approval was obtained from the institution’s ethics committee.
Acknowledgments
None.
Conflicts of Interest
None.
References
- Acquired TTP: clinical manifestations and diagnosis-UpToDate [Internet].
- Reese JA, Muthurajah DS, Kremer Hovinga JA, Vesely SK, Terrell DR, et al. (2013) Children and adults with thrombotic thrombocytopenic purpura associated with severe acquired Adamts13 deficiency: comparison of incidence and demographic and clinical characteristics. Pediatric Blood Cancer 60(10): 1676-1682.
- Hereditary thrombotic thrombocytopenic thrombocytopenic purpura (TTP)-UpToDate [Internet].
- Velasco Pedro P, Buitrago N, Gonzalez Danna (2015) THROMBOTIC THROMBOCYTOPENIC PURPURA: DIFFERENTIAL DIAGNOSIS WITH HEMOLYTIC UREMIC SYNDROME. CASE REPORT. Cienc E Investig Medico Estud Latinoam 20: 20-24.
- Olaya V, Montoya JP, Benjumea ÁM, Gálvez K, Combariza JF (2012) Thrombotic thrombocytopenic purpura Description of the diagnosis and management of a rare entity with high mortality. Acta Medica Colomb 37(4): 201-206.
- Joly BS, Coppo P, Veyradier A (2017) Thrombotic thrombocytopenic purpura. Blood 129(21): 2836-46.
- Jamme M, Rondeau E (2017) The PLASMIC score for thrombotic thrombocytopenic purpura. Lancet Haematol 4(4): e148-e149.
- Bendapudi PK, Hurwitz S, Fry A, Marques MB, Waldo SW, Li A, et al. (2017) Derivation and external validation of the PLASMIC score for rapid assessment of adults with thrombotic microangiopathies: a cohort study. Lancet Haematol 4(4): e157-e164.
- Paydary K, Banwell E, Tong J, Chen Y, Cuker A (2020) Diagnostic accuracy of the PLASMIC score in patients with suspected thrombotic thrombocytopenic purpura: a systematic review and meta-analysis. Transfusion 60(9): 2047-2057.
- Acquired TTP: initial treatment.
- Morales Montoya A (2019) Thrombotic thrombocytopenic purpura. Med Interna Mexico 35(6): 906-911.
- Oliveira DS, Lima TG, Benevides FLN, Barbosa SAT, Oliveira MA, Boris NP, et al. (2019) Plasmic score applicability for the diagnosis of thrombotic microangiopathy associated with ADAMTS13-acquired deficiency in a developing country. Hematol Transfus Cell Ther 41(2): 119-124.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.