Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Usefulness of the Modified Rockall and Baylor Scales in Hemorrhage Upper Digestive due to Peptic Ulcer
*Corresponding author: Pedro Rolando López Rodríguez, First and second-degree specialist in general surgery, Hospital Enrique Cabrera, Havana, Cuba.
Received: June 22, 2023; Published: July 13, 2023
DOI: 10.34297/AJBSR.2023.19.002603
Abstract
Introduction: Upper gastrointestinal hemorrhage is a common health problem worldwide and one of the emergencies determining a huge number of admissions into general surgery services in our scenario, it is therefore of great clinical and sanitary importance. Objective: To determine the usefulness of the modified Rockall and Baylor scores in predicting rebleeding in patients with upper gastrointestinal hemorrhage.
Method: A prospective, descriptive, observational study was carried out, including patients admitted for upper gastrointestinal hemorrhage due to peptic ulcer in Enrique Cabrera, from January 1st, 2018, to December 31, 2022.
Results: Among the 300 patients admitted for upper digestive hemorrhage due to peptic ulcer, we took a sample of 71 patients. All patients were performed endoscopic treatment, while 8.4% were performed surgical treatment. Nine patients presented with rebleeding (12.7%). The modified Rockall and Baylor scores showed a specificity of 82% and 86%, respectively, with low sensitivity in both cases. Despite this, the Rockall score is the one with the highest sensitivity.
Conclusions: The two scores were highly specific, but the Rockall score was more sensitive for identifying patients at high risk of rebleeding.
Keywords: Upper Gastrointestinal Hemorrhage, Prognostic scores, Surgery
Introduction
Upper Gastrointestinal Bleeding (UGH) is a common health problem throughout the world. the world and is one of the emergencies that determines a large number of admissions in General Surgery services in our environment, so it is of great importance clinical and health in order to predict the possibility of rebleeding and thus reduce the mortality of this disease, prognostic scales were designed, one of them was the Baylor scale, created in 1995, and subsequently modified. In 1996, the Rockall scale by the National Audit of Acute Gastrointestinal Hemorrhage. It is currently one of the most used and well-known worldwide. The Rockall clinical scale has application in classifying individuals with upper gastrointestinal bleeding according to the risk of presenting active gastrointestinal bleeding or recent, and that require urgent digestive endoscopy. When Added to the results of endoscopy, the full Rockall scale has been shown to be useful for predicting the probability of rebleeding, the need for surgery, or the risk of mortality. Subsequently, others were designed such as the Glasgow Blatchford and the Cedars-Sinai Medical Center Predictive Index. They differed in terms of the elements they use, clinical, laboratory, endoscopic, or combinations of them, which allows adapting its use according to different health institutions [1-5]. The main objective is to determine the usefulness of the Rockall and Baylor scales. modified to predict rebleeding in patients with upper gastrointestinal bleeding in the Teaching General Hospital “Dr. Enrique Cabrera. It is of great importance because allows us to compare two prognostic scales applicable to our environment and according to the results to use in patient care the one with the greatest specificity and sensitivity brings us. This will reduce morbidity and mortality from this entity in the center.
Methods
A descriptive, prospective, observational study was carried out at the General Hospital Teacher “Enrique Cabrera”, from January 1, 2018, to December 31, 2022. Aimed at all patients with HDA caused by peptic ulcer treated in that period. The universe was 300 patients, from which a sample was taken. randomized study of 71 patients, who met the inclusion criteria (greater than 19 years old, with a diagnosis of HDA who underwent a digestive endoscopy superior. Patients with no endoscopic signs of recent bleeding (Forrest III) and those with underlying hematologic diseases
Results
The mean age was 52.2 years (SD 11.5 years). Patients older than 60 years (33.8%), and the male sex with 42 patients (59.1%). By applying the scale of Rockall, the predominance of patients with high risk of rebleeding was observed (70.4%) (Table 1).
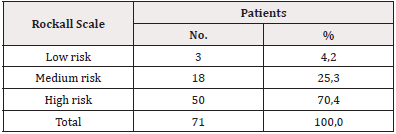
Table 1: Distribution of patients according to risk rebleeding with Rockall Scale.
Source*: Information obtained from medical records.
When using the Baylor scale, a stratification of the patients at high risk greater than in Rockall, these being 91.5% of the sick (Table 2).
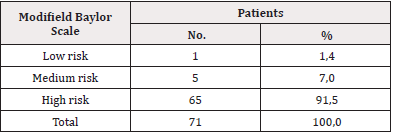
Table 2: Distribution of patients according to risk rebleeding with modifield Baylor Scale.
Source*: Information obtained from medical records.
There were 9 (12.6%) patients who presented rebleeding during admission. When analyzing the sensitivity and specificity of the scales, we observed that the Rockall scale presented low sensitivity (18%) of high risk and high specificity (82%), intermediate risk and Low rebleeding had a specificity of 100% with very low sensitivity.
On the Baylor scale, the sensitivity regarding rebleeding in high risk was 13.8% (9 patients) with very low sensitivity in the rest of the categories. The High-risk specificity was 86.2%, with 100% for the rest of the categories. The intermediate and low risk was 6 patients. There were 9 (12.6%) patients who presented rebleeding during admission. When analyzing the sensitivity and specificity of the scales, we observed that the Rockall scale presented low sensitivity (18%) of high risk and high specificity (82%), intermediate risk and Low rebleeding had a specificity of 100% with very low sensitivity. On the Baylor scale, the sensitivity regarding rebleeding in high risk was 13.8% (9 patients) with very low sensitivity in the rest of the categories. The High-risk specificity was 86.2%, with 100% for the rest of the categories. He intermediate and low risk was 6 patients.
Discussion
In the study carried out, we can see that most of the patients were aged over 60 years of age, similar to García, [6]. who found in his study that most they were elderly. The observed meaning was similar to Mildred’s study, [7]. as well as in the rego studio [8]. where 118 of 161 cases presented 60 years. The results are similar to those obtained by most of the consulted authors who report that the age at which these cases most frequently occur is 60 years or older. The sex that predominated in the study was male. This coincided with the study of Bravo Valencia [9]. where the majority were men, likewise García Valdés [10]. obtained in his study, the largest number of patients diagnosed with HDA due to ulcer peptic was male, with a ratio of approximately 1.7:1. The latter matches Rego [8] that shows a predominance of the male sex, which shows several of the in the reviewed literature, the sex that predominates in patients with HDA is male. Endoscopic procedures have made it possible in many cases to stop the bleeding, reduce the number of urgent interventions and carry out the elective ones that They always pose less surgical risk. On some occasions, control of the bleeding for a sufficient period, enables the patient to reach the operating room in better conditions of hemodynamic stability; in others it constitutes the solution of problem. Study patients received various treatments, endoscopic, surgical, and both. In our study, the most used was the endoscopic, unlike other studies in which it is found that medical treatment predominated, followed by medical-endoscopic. This was evidenced in the study by García and Gil [10] where 91.4 % received exclusive medical treatment, 2.9% associated with medical treatment the endoscopic and 5.7% received surgical treatment Basto Valencia [11] in his studio suggests that the most effective treatment is the medical-endoscopic one. Regarding the Forrest classification, it was observed that the most frequent was the ulcer with Forrest IIc (lesion with black base). Hierro González [12] agrees with this finding since that he found that the majority of cases were classified as stage IIc (29.9%); without However, García Valdés [10] in his work on endoscopic results according to the Forrest classification, a predominance of group IIb was observed with 40 patients (28.6%) It was observed that most of the works present a classification of Forrest fundamentally in II what varies is in IIa, IIb or IIc, which is related with the progress that has been made in the various treatments, both medical and endoscopic that the patient may have.
The presence of rebleeding was lower than the study by García and Gil [10] of patients of the series, 29 of them (20.7% of the sample) presented signs and symptoms of rebleed Bravo Paredes [9] presented in his work a rate of rebleeding at 30 days (5.52%). It could be observed that in several studies the rebleeding varies from 10% to 30%, despite effective endoscopic therapy in gastrointestinal bleeding discharged for peptic ulcer. Hence the importance of identifying patients with high risk of rebleeding in order to decrease this index. The Rockall scale identified more than half of the patients at high risk of rebleed in the work of Infante Velázquez [13] on the usefulness of the scale of Rockall, 83 patients (70.3%) were classified as high risk, while 29.7% (35 cases) were found within the low-risk category. Others of the reviewed studies showed similar values, which gives us reference that the Most patients fall into the highest risk category, which is very important in predicting the possibility of rebleeding. Like the Rockall scale, the modified Baylor scale identified most of the patients at high risk of rebleeding. However, García Valdés [6] in his study on the modified Baylor index obtained patients with a low-risk score from 0 to 7 points) there were 63 patients and in the group with a medium risk score (from 8 to 11 points) is made up of 46 patients, the high-risk group (greater than or equal to 12 points) of the 31. The specificity was high on both scales. Rockall’s had greater sensitivity than the modified Baylor test to identify patients at high risk of rebleeding. This is in agreement with other studies showing similar results. Such as that of Bravo Paredes [9] in his study on the usefulness of the Baylor scale. This The author presented a sensitivity and specificity to predict mortality of 13 (S: 75% and E: 82%) and that of Infante Velázquez [13] in his work on the utility of the scale of Rockall the ability of the Rockall clinical index to predict the need for Urgent endoscopy was excellent, with an area under the curve (AUC) value= 0.960. (95% CI: 0.904-1.017). The cut-off points equal to 1 turned out to have the best predictive value (Y= 0.971), with a sensitivity of 97% and specificity of 71. In a review article on the diagnosis and treatment of the patient with gastrointestinal bleeding, Trawick and Yachimski [14,15] summarize the diagnostic performance of the pre-endoscopic Rockall scale for the rebleeding with the following values: sensitivity, 69.6%; specificity, 17.5%; worth positive predictive, 5.5% [16-18].
Conclusions
The application of the prognostic indices in this case that of Rockall and Baylor modified proved to be a tool that helps us predict the possibility of rebleeding and thus reduce HDA mortality. Both scales were highly specific, but Rockall’s was more sensitive to identify patients with high risk of rebleeding.
Author Contributions
Dra. Yaneris Pérez Arias: He wrote the article, participated in the diagnosis and surgical treatment of the patient and his evolution, searched for bibliographic references.
Dr. Pedro Rolando López Rodríguez: He helped write the article and mark the bibliography, applied the rules for article presentation and translated the work.
Conflict of Interest
The authors declare that there is no conflict of interest.
Acknowledgments
None.
References
- Kahi CJ, Jensen DM, Sung JJ (2005) Endoscopic Therapy Versus Medical Therapy for Bleeding Peptic Ulcer with Adherent Clot: A Meta-analysis. Gastroenterology 129(3): 855-862.
- Allen A (2013) Gastroduodenal mucosal protection. Physiol Rev 73: 823.
- Domschke W, Lederer P, Luz G (1983) The value emergency endoscopy in upper gastrointestinal bleeding: Review and analysis of 2014 cases. Endoscopy 15(1): 126-131.
- Masaoka T, Suzuki H (2014) Does the AIMS65, a new risk score for upper gastrointestinal bleeding, work in Japan? Dig Endosc 26(3): 331-332.
- Huang KW, Luo JC, Leu HB (2012) Chronic obstructive pulmonary disease: an independent risk factor for peptic ulcer bleeding: a nationwide population-based study. Aliment Pharmacol Ther 35(7): 796-802.
- García Valdés A (2010) Protocol of action in the gastrointestinal hemorrhage. Med Int Emerg 30(10): 28-30.
- Koksal O, Ozeren G, Mildred A, Ozdemir F, Armagan E, et al. (2012) Prospective validation of the Glasgow Blatchford scoring system in patients with upper gastrointestinal bleeding in the emergency department. Turk J Gastroenterol 23(5): 448-455.
- Rego Hernandez JJ (2006) Clinical-therapeutic characterization of digestive bleeding high. MEDISAN 41(3): 90-94.
- Bravo Paredes EA, Guzmán Rojas P, Gallegos López RC, Ciliotta Chehade A, Corzo Maldonado MA, et al. (2013) Usefulness of Baylor's score in patients with upper gastrointestinal bleeding in a hospital in Lima - Peru. Rev Gatroenterol Peru 33(4): 307-313.
- García Valdés A, Gil Manrique L, Brizuela Quintanilla R, García Vega M (2007) Index Modified from Baylor. Experiences of its use in an intermediate care unit Surgical. Rev Cubana Med Int Emerg 6(1).
- Basto Valencia M, Vargas Cárdenas G, Chaparro A (2005) Risk factors increase morbidity and mortality in patients with upper gastrointestinal bleeding in National Hospital. "Archbishop Loayza"1980-2003. Rev Gastroenterol of Peru 25(3): 90-123.
- Hierro González A, Jiménez Sánchez N (2013) Upper digestive bleeding. Behaviour clinical in a group of patients. Med Int Emerg 42(4): 69-75.
- Infante Velázquez H (2016) Gastrointestinal bleeding due to esophagus-gastric varicose veins. Minutes Peruvian Med 23(3): 156-161.
- Trawick EP, Yachimski PS (2012) Management of non-variceal upper gastrointestinal tract hemorrhage: controversies and areas of uncertainty. World J Gastroenterol 18(11): 1159-1165.
- Santiesteban Pupo WE, Borges Sandrino RS, Ramon Musibay E (2018) Value of the Rockall Scale in the prediction of morbidity of upper gastrointestinal bleeding. Rev Hab Cienc Med 17(5): 728-735.
- Gonzála López N (2020) Usefulness of the nasogastric tube and compliance with the Rockall index in non-varicose upper gastrointestinal bleeding. Enferm Endosc Diag 7(1): 4-11.
- Martinez SG, Figueroa NP, Toro PJ, et al. (2021) Current behavior in the face of upper gastrointestinal bleeding. From diagnosis and treatment. Rev Cir 73(6): 728-743.
- Rondon Porras A, Carmona Garcia V, Gonzalez Acosta I, et al. (2022) Rev Esc Cienc Salud Univ Pont Boliv Col 4(1): 67-74.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.