Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
A Case of Glossodynia after Dental Implant Replacement Successfully Treated with Goreisan and Kamishoyosan
*Corresponding author: Hidenori Tanaka, Onoba Tanaka Ladies Clinic, Department of Traditional Japanese Medicine, Japan.
Received: December 21, 2023; Published: December 26, 2023
DOI: 10.34297/AJBSR.2023.20.002788
Keywords: glossodynia, dental implant replacement, goreisan, kamishoyosan
The oral implant extends from the living jawbone within the body to the oral cavity outside the body. Consequently, it is continuously exposed to external influences from the oral cavity. One of the drawbacks associated with implants is the potential for inflammation in the tissues surrounding the implant [1]. In this case report, we present a patient who developed glossodynia following implantation and was successfully treated with Kampo medicine alone.
The patient is a 56-year-old woman who has been through menopause for 51 years and has had one childbirth. Her medical history includes a right ovarian cystectomy at the age of 32. Two months prior to the current date, she underwent dental implantation. Following the surgery, she presented to our clinic in the month preceding the current date, reporting symptoms of glossodynia as diagnosed by “3rd edition of the International Headache Classification” [2]. We initially prescribed goreisan (GRS) with considering the presence of a tooth mark tongue and kikyoto for anti-inflammatory purpose, but these treatments were not effective.
Subsequently, she sought care at an internal medicine clinic due to ongoing glossodynia and gastrointestinal disturbances. There, she was prescribed anchusan and hangekobokuto, but these treatments also proved ineffective. She returned to our clinic seeking Kampo therapy for glossodynia.
Upon examination, the patient appeared slim, had a slightly pale complexion, exhibited a weak pulse, and her abdominal dia gnosis did not reveal any specific abnormalities. However, her ton gue presentation was distinctive (Fig. 1a). The main body of the tongue exhibited a fluid retention (swollen, moist, and tooth marks on tongue), and the central color of her tongue coating ranged between yellow and black, brown, suggesting ongoing inflammation related to the implant. During her treatment, we considered tongue diagnosis to be of paramount importance.
First, we selected GRS to address the fluid retention of the tongue, as previously mentioned [3]. Fluid is regarded as a colorless substance that sustains the nutrition and metabolism of the living organism; it encompasses components other than blood within the body fluid.
Secondly, given the change in tongue coating color from yellow to black-brown, indicative of potential oral issues related to the implants, we decided to include kamishoyosan (KSS) based on our prior experience [4]. We prescribed GRS (a Tsumura medical extract) at a dose of 5.0 g/day for 14 days and KSS (a Tsumura medical extract) at the same dosage for 14 days. The dosing regimen involved administering each Kampo formula, 2.5g in the morning and 2.5g in the evening, over the course of 14 days.
After treatment with Kampo, the pain in the patient’s tongue decreased by over 90%, and it was considered effective, and her overall condition had improved. Additionally, her gastrointestinal issues had also alleviated. The yellow-to-brown coloration of her tongue coating transformed into a vibrant and healthy appearance (Fig. 1b).

Figure 1A: Tongue examination a. Return visit, the body of her tongue is swollen and moist with tooth marks. The color of her tongue coating ranges between yellow and black, brown.
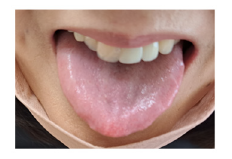
Figure 1B: b. Fourteen days after the administration of goreisan and kamishoyosan, the yellow-to-brown coloration of her tongue coating transforms into a vibrant and healthy appearance.
Currently, she is experiencing minimal tongue pain and has remained symptom-free without any noticeable side effects for the past 4 months.
It is important to note that GRS is a well-known diuretic with the ability to regulate fluid metabolism in the body, exhibiting diuretic effects in cases of edema and antidiuretic effects in cases of dehydration [3]. In this case, GRS effectively addressed the fluid retention of the tongue. Furthermore, previous reports have suggested that GRS can be effective for glossodynia [5]. This may be attributed to its potential to enhance tissue metabolism, particularly in local mucous membranes, alleviate stasis, and improve lymphatic flow, ultimately leading to relief from chronic pain.
Conversely, we have previously reported various beneficial effects of KSS on oral problems. KSS, a recognized prescription for menopausal women, contains ten different herbal components. Among these, Bupleuri Radix, Paeoniae Radix, and Atractylodis Lanceae Rhizoma have demonstrated anti-inflammatory properties. However, treating glossodynia with KSS alone has proven challenging [4]. Therefore, we decided to leverage the pharmacological effects of both GRS, which promotes tissue metabolism in local mucous membranes of the tongue, and KSS, with its anti-inflammatory properties, administered simultaneously. This combined approach led to a successful outcome for the patient. It seems beneficial that we not only rely on our conventional medical experience but also focus on tongue diagnosis in Kampo assessment.
Conflict of interest
Hajime Nakae received honoraria from Tsumura & Co. The other authors declare no conflicts of interest.
Informed Consent
Informed consent was obtained from the participants.
Approval of the research protocol by an Institutional Reviewer Board and the approval number
N/A
Registry and the Registration No. of the study/ trial
N/A
Animal Studies
N/A
References
- Japanese Society of Oral Implantology.
- (2018) Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition Cephalalgia 38(1): 1-211.
- STORK (http://mpdb.nibiohn.go.jp/stork/)
- Tanaka H, Irie Y, Nakae H (2021) Kamishoyosan is effective for female patients with oral and nasal cavity problems. Traditional & Kampo Medicine 8(3): 251-254.
- Ayuse T, Okayasu I, Tachi YM, Sato J, Saisu H, et al. (2020) Examination of pain relief effect of Goreisan for glossodynia: Medicine 99(33): e21536.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.