Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Assessment of Knowledge and Attitude Towards the Medical Interdisciplinary Team Among Health Science Students
*Corresponding author: Manana Machitidze, The University of Georgia, School of Health Science, Tbilisi, Georgia.
Received: October 02, 2023; Published: October 09, 2023
DOI: 10.34297/AJBSR.2023.20.002691
Abstract
Background: The team principle of work in the clinical sector, based on interdisciplinary cooperation, is associated with the effectiveness of treatment and increased patient safety. In addition, with lower hospitalization rates, complications, and medical errors. A multidisciplinary approach to the treatment process will strengthen and improve patient care coordination and access to medical services.
Aim: Providing/developing the knowledge and skills necessary for working in an interdisciplinary team for health school students should be carried out at the level of academic education. The skills and ability to work in a multidisciplinary team, which they will develop, is a prerequisite for perceiving the importance of interdisciplinary cooperation and recognizing its benefits - both for patients and medical professionals.
Methodology: The research methodology is a quantitative, cross-sectional study.
Results: Students in the graduating semester of medicine, nursing, and pharmacy at the University of Georgia Health School almost 100% understand their role in the interdisciplinary team. However, it should also be noted that they need practice, a deepening of knowledge, and more self-confidence to manage their function correctly. The knowledge, skills, and attitude of the students participating in the study toward interprofessional teamwork are positive. 60% of surveyed students support the introduction of simulation training for interprofessional work at different levels of education.
Conclusion: The student needs to get information about the interdisciplinary team and be able to apply it practically during the simulation training to focus on correct communication and time management. This will allow the student to apply knowledge and feel confident as a full-fledged member of an interdisciplinary team when working in the clinic after graduation.
Keywords: Interdisciplinary teamwork, Multidisciplinary team, Health Science students, Medical student
Introduction
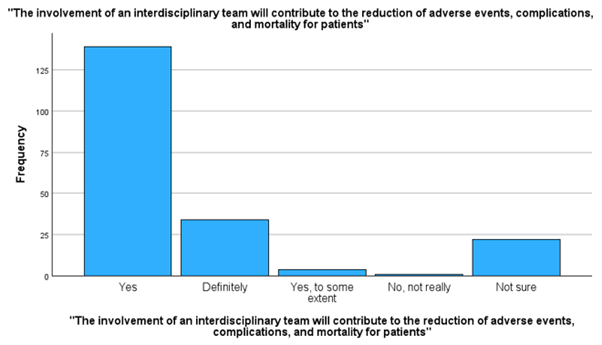
Patient safety is an important area of health care that ensures to prevent and reduce risks and errors that threaten patient safety while receiving medical services [1]. In 2010, the World Health Organization (WHO) published an action framework for interprofessional education and collaborative practice, emphasizing that the involvement of an interdisciplinary team in the patient care process will contribute to the reduction of adverse events, complications, and mortality for patients [2]. Modern information infrastructure and a sufficient and adequately qualified workforce are fundamental to the health system’s ability to be resilient and minimize harm. Violation of patient safety principles, neglect, or failure to comply increases the risk of growing patient deaths and disability cases every year [3]. “An interdisciplinary team is a group of professionals who work together to achieve a common goal” [2]. In the clinic, and not only there, but the teamwork of the medical interdisciplinary team is also essential for a patient’s successful treatment solution, more effective. When we talk about an interdisciplinary team, we mean a team of professionals from different specialties of one discipline (therapist, neurologist, cardiologist, etc.) or a group of specialists from other fields - doctor, nurse, pharmacist, etc. Each member must understand the principle of teamwork, his role in the team, and his readiness to share responsibility and work hard in the group. On the other way, the work of the team will need to be more effective. The result will be unsuccessful treatment and putting the patient at risk.
Many factors increase the need for interdisciplinary teamwork. Among them are the aging of the population, the risk of increasing chronic diseases, and the rapid development of various healthcare fields (specialties), which increases the risk of meeting all the complexities of patients’ needs. Interdisciplinary teamwork will be a continuous, growing way to improve patient care and service quality [4].
Methodology
The study was conducted among students of the Nursing, Medicine, and Pharmacy program of the University of Georgia Health School. The research methodology is a quantitative, cross-sectional study. The selection criteria of the respondents were determined by the main characteristics of the target population related to the research question. Three target groups were identified: nursing, medicine, and pharmacy program students. The criteria for inclusion in the study were students of the first [5,6] and final year (registered in the last two semesters) of nursing, medicine, and pharmacy programs who have not completed/have completed all fundamental and essential clinical subjects. All the respondents who agreed to participate took part in the study.
The research tool is a questionnaire with closed questions, developed in advance and approved by the Ethics Commission of the University of Georgia. Analytical and descriptive statistics are used to analyze the research results. The results of the research were statistically processed in the SPSS program.
Results and Discussion
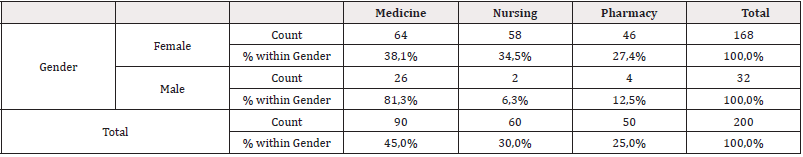
The questionnaire consisted of ten closed and one open question. The interviews of the respondents involved in the study were confidential and were mainly conducted through an online survey compiled in the Google Forms program. The students received the questionnaire on their UG page, in which medicine, nursing, and pharmacy students from the University of Georgia School of Health participated. Two hundred respondents took part in the survey. Among them were 60 for the nursing program, 50 for the pharmacy program, and 90 for the medicine program (Table 1). In total, the questionnaire was sent to 200 students. 100% participated in the study. Of the 200 interviewed, 168 respondents, or 84%, were female, and 32, or 16%, were male.
Forty-six respondents - 23% were from the first semester, 58 respondents - 29% from the second semester, 37 respondents - 18.5% from the seventh semester, 42 interviewees - 21% from the eighth semester, seven respondents - 3.5% from the eleventh and ten respondents - 5% from the twelfth-semester student. To the question - have you heard about the interdisciplinary team? - the answers of the respondents were different. Ninety respondents, or 49%, have heard about the multidisciplinary team, 61, or 30.5%, have not heard, 30, or 15%, know partially, and 11, or 5.5%, find it difficult to answer. 13 students - 6.5% think that an interdisciplinary team is a team consisting of doctors from different specialties that take care of the patient’s safety. 41 students - 20.5% say that the group of doctors and nurses is responsible for safe patient care. And 146 respondents, or 73%, say that healthcare professionals from different disciplines work together to provide safe patient care and treatment, including managing physical, psychological, and spiritual needs (Table 2). Fifty respondents, or 26%, answered that patient-oriented care with proper communication and cooperation. Four respondents, - 2%, say that this is good cooperation. One hundred forty-five respondents - 72.5% say it is practical cooperation, increases patient safety, lowers hospitalization rate, and reduces complications and medical errors. And one respondent, i.e., 0.5%, does not answer (Table 3).

Table 2: Which semester are you a student of? *Have you heard of an interdisciplinary team? Crosstabulation.
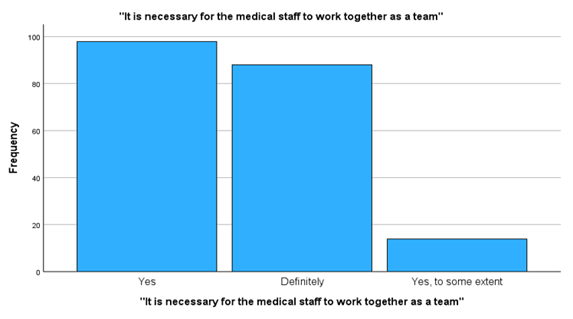
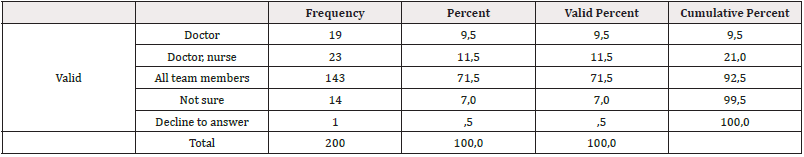
19 of the respondents believe that the “leader” in the interdisciplinary team is a doctor, 23 say that it is a doctor and a nurse, 143 respondents say that all members of the team, 14 respondents find it difficult to answer, and one respondent, does not answer (Table 4). However, it should be noted that 93% of the respondents agree with the opinion that medical personnel should work in a team, and only 7% partially agree (Figure 1).
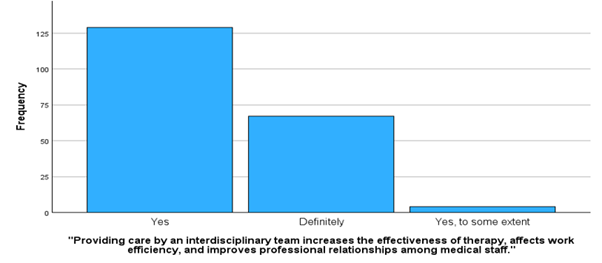
The open question of the research was about the attitude of students based on their profession and their role in the interdisciplinary team; according to the analysis of the student’s answers, the question, in your opinion, what is your role in the multidisciplinary team based on your profession, out of 200 respondents, 79 responded, while 121 respondents did not answer - 60.5%. According to the research, it was determined that the students think that information should be given to the patient correctly and appropriate treatment should be given to them. Must take responsibility and cooperate with teammates. Have proper communication skills and be tolerant. The majority of students surveyed believe their role is to collaborate with medical staff members to work toward patient- centred care and improved practice. However, respondents also think they are leaders in a given team and their role is the most important (Figure 2 and Figure 3).
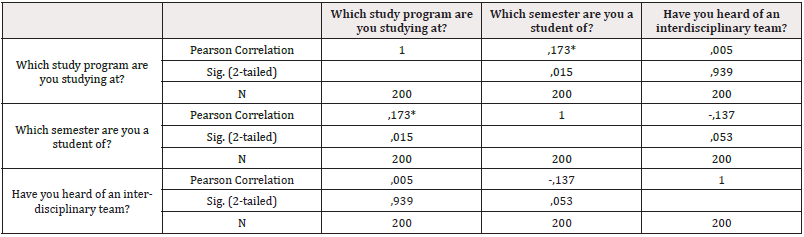
Table 6: Who is the “leader” of the interdisciplinary team?
Note*: *Correlation is significant at the 0.05 level (2-tailed).
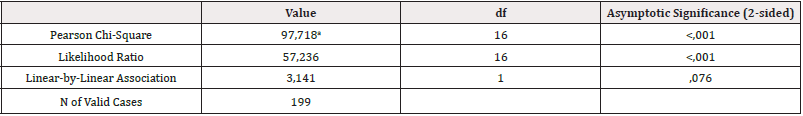
The information obtained as a result from the interviewed respondents was processed in the SPSS program and was conducted in the data analysis and chi-square testing to confirm and reject the null or alternative hypotheses. According to the Chi-Square analysis (Cl-0.01), as a result of testing, alpha is less than 0.01, which means that the null hypothesis - the students of the nursing, medicine, and pharmacy graduate course of the University of Health School of Georgia must understand the essence of the medical interdisciplinary team, their role, importance and are ready for teamwork - is true and there is a relationship between these two variables. As for the alternative view - the students of the nursing, medicine, and pharmacy graduate course of the University of Georgia Health School do not understand the essence of the medical interdisciplinary team, their role, and importance and are not ready for teamwork, in this case, it turned out to be false, and the relationship between them exists (Table 5). The study results showed a strong correlation between study semesters and students’ understanding of multidisciplinary teamwork - the higher a student’s semester, the more knowledge he has about the interdisciplinary team. According to the obtained correlational analysis, we can judge how correctly the emphasis is placed on the multidisciplinary team in the curriculum (Table 6).
Teamwork as a preferred method of collaboration in health care was popularized in the 1960s and has since been widely recognized as a measure to improve health care quality. Studies have shown that medical care based on interdisciplinary collaboration is associated with increased patient safety, lower rates of hospitalization, and reductions in complications and medical errors. In addition, it enhances care coordination and improves patient access to medical services [5].
A 2010 World Health Organization report emphasized the importance of the interdisciplinary team in family medicine, infectious disease treatment, and control. Studies have shown that such groups are more effective in controlling epidemics and non-communicable diseases. Institutions, where healthcare professionals collaborate, have reduced rates of medical complications and errors, as well as patient mortality and hospital length of stay. In addition, further research has shown improvements in patient access to medical care, proper coordination, and increased patient safety [2].
An interdisciplinary team can ensure a safe and high-quality patient treatment process, improving health service delivery and increasing the reliability and referral of patients to medical institutions. Students of healthcare programs at the initial stage of professional education need more understanding of the essence of professional collaboration; perhaps they need to understand their own and others’ roles and have effective communication during patient care [7]. During theoretical, simulation, and practical training, students gain knowledge and experience working collaboratively with professionals from different disciplines [8].
Research shows that providing care by an interdisciplinary team increases the effectiveness of treatment, affects work efficiency, and improves professional relationships among medical staff. A multidisciplinary approach to patient health problems, in which representatives of at least two professions collaborate to provide comprehensive care, can be a response to patient expectations and ongoing changes in society. For effective collaboration, medical staff must be able to work in a group. Professionals must be able to communicate effectively with other team members, the patient, and their family. They must be able to define the scope of their and other professionals’ competencies and accept responsibility for participating in decision-making.
Effective interprofessional collaboration is closely related to a work environment where they can equally contribute to patient care [7]. However, studies show that the role of doctors is often overshadowed by other healthcare personnel, such as nurses and pharmacists [9]. The perception of an interdisciplinary team is at risk due to many factors. Several studies have shown that, in many cases, the collaboration of nurses and doctors is more parallel than joint [10]. The patients and medical staff often accept the doctor’s “priority” leader position in the treatment process. Several studies have confirmed the heterogeneous attitude of doctors and nurses towards teamwork [11]. The current survey, conducted among health sciences students at the University of Georgia, once again emphasized doctor-students’ attitudes towards the work in a multidisciplinary team. Although the vast majority of respondents from different faculties understand that teamwork is essential and agree with this opinion, 9.5% of the surveyed students believe that the leader is a doctor, and 7% find it challenging to answer. This increases the chance of reinforcing the wrong opinion during working in the clinic. That is why, in the teaching process, emphasis and the correct approach to interdisciplinary teamwork are essential. Neglecting it in the studying process may become a prerequisite for forming “leadership” and ignores the membership of the multidisciplinary team [6]. It’s a pity that Georgian healthcare workers are still influenced by the “Soviet period,” the group still makes physicians a priority and prestigious profession [12]. For students to acquire the skills necessary for teamwork, it is vital to create a curriculum where they can learn from and about each other, solve problems together, and share experiences and knowledge. Interprofessional education fulfills these assumptions [13].
A factor supporting the implementation of interprofessional education, which builds the ability to work in an interdisciplinary team, is that medical students perceive the importance of multidisciplinary cooperation and recognize its benefits - both for patients and medical professionals [5]. The health care team, the primary care link (physicians, nurse practitioners, and physician assistants), and pharmacists working at the clinical and professional development levels will achieve essential steps in reducing the prescription of potentially inappropriate medications, thereby increasing patient safety [14].
Even in a successful collaboration, the team may differ in composition and experience. Still, they often share a view and opinion that allows for developing and implementing the proper care plan and high-quality patient care. Among them, it is essential to consider a patient-centred approach/practice. A successful interdisciplinary team understands the patient’s needs first and foremost. It is necessary that the patient is maximally involved in the treatment process and considered a member of the collaborative team. Students of healthcare programs at the initial stage of professional education need more understanding of the essence of professional collaboration; perhaps they need to understand their own and others’ roles and have effective communication during patient care [7]. During theoretical, simulation, and practical training, students gain knowledge and experience working collaboratively with professionals from different disciplines [8].
Based on the analysis of different study results, the involvement of an interdisciplinary team will detect the diagnosis of almost all patients more timely than each separately; therefore, the treatment starts faster, and the level of patient satisfaction increases. In 2007, the (IDT) Global Partnership for the Management of Type 2 Diabetes (T2DM) recommended an interdisciplinary team approach for effective diabetes management. [9]. A Canadian cohort study found that patients exposed to interprofessional care had significantly reduced hospitalizations after their involvement [15]. Interdisciplinary care is associated with greater patient preparedness and improved health across stages of chronic kidney disease, particularly in patients at increased risk of progression [16-18].
Conclusion
An interdisciplinary approach to patient health problems, in which representatives of at least two professions collaborate to provide comprehensive care, can be a response to patient expectations and ongoing changes in society. For effective collaboration, medical staff must be able to work in a group. Professionals must communicate effectively with other team members, patients, and their families. They must be able to define the scope of their and other professionals’ competencies and accept responsibility for participating in decision-making.
The benefits of interdisciplinary care are unambiguously clear and measurable. However, certain obstacles may prevent the maximum efficiency of its planning/implementation. Team members’ readiness, knowledge, attitude, communication, responsibility, and time management should be considered during collaborative work. Each of these skills is necessary for the student to acquire during his studies at the university. For this, it is required to actively collaborate in the learning process between students of different programs during simulation teaching, case discussions, and clinical practice. This will theoretically and practically prepare future healthcare professionals, who will be members of interdisciplinary teams, and increase self-confidence and form the right attitude to work in the actual clinical space.
Acknowledgment
The authors thank the Medicine, Nursing, and Pharmacy students at the University of Georgia for their interest in the study and sincere responses. Additionally, we would like to thank the authors of the literature review articles cited in this article and international organizations for open-accessing valuable research findings, recommendations, and opinions.
Conflict of Interest and Ethical Consideration
No conflict of interest and ethical norms were violated during the research process. Before conducting the survey, the questionnaire was developed and submitted to the Ethics Council of the University for approval. The approved questionnaire was sent to the students through the university’s student page. The questionnaire’s introduction briefly described the study’s purpose to the respondents, and their answers to the questions were considered as their informed consent. The study findings were presented in a public report to the respondents, the participating departments’ staff, and the School of Health faculty. Financial interest or funding was not used for the research.
References
- World Health Organization. (n.d.-b). Patient safety. World Health Organization.
- World Health Organization. (n.d.-a). Framework for action on Interprofessional Education & Collaborative Practice. World Health Organization.
- Patient safety - OECD. (n.d.-b).
- Hall P, Weaver L (2001) Interdisciplinary education and teamwork: A Long and Winding Road. Med Educ 35(9): 867-875.
- Bendowska A, Baum E (2023) The significance of cooperation in interdisciplinary health care teams as perceived by Polish medical students. Int J Environ Res Public Health 20(2): 954.
- Berduzco Torres N, Choquenaira Callañaupa B, Medina P, Chihuantito Abal, L A Caballero, et al. (2020) Factors related to the differential development of inter-professional collaboration abilities in medicine and nursing students. Front Psychol 11:432.
- Costello M, Prelack K, Faller J, Huddleston J, Adly S, et al. (2017) Student experiences of interprofessional simulation: Findings from a qualitative study. J Interprof Care 32(1): 95-97.
- Lee W, Kim M, Kang Y, Lee YJ, Kim SM, et al. (2020) Nursing and medical students’ perceptions of an interprofessional simulation-based education: A qualitative descriptive study. Korean J Med Educ 32(4): 317-327.
- McGill M, Felton A M (2007) New global recommendations: A multidisciplinary approach to improving outcomes in diabetes. Prim Care Diabetes 1(1): 49-55.
- Vatn L, Dahl BM (2021) Interprofessional collaboration between nurses and doctors for treating patients in surgical wards. J Interprof Care 36(2): 186-194.
- Hojat M, Gonnella JS, Nasca TJ, Fields SK, Cicchetti A, et al. (2003) Comparisons of American, Israeli, Italian and Mexican physicians and nurses on the total and factor scores of the Jefferson Scale of attitudes toward physician-nurse collaborative relationships. Int J Nurs Stud 40(4): 427-435.
- Machitidze M, Goshadze N (2023) Attitude toward continuing medical education and professional development of emergency medical personnel - cross-sectional study of physicians and nurses. European Scientific Journal ESJ 19(9): 1.
- Makino T, Shinozaki H, Hayashi K, Lee B, Matsui H, et al. (2013). Attitudes toward Interprofessional Healthcare Teams: A comparison between undergraduate students and alumni. J Interprof Care 27(3): 261-268.
- Rahayu SA, Widianto S, Defi IR, Abdulah R (2021) Role of pharmacists in the interprofessional care team for patients with chronic diseases. J Multidiscip Healthc 14: 1701-1710.
- Wei SY, Chang YY, Mau LW, Lin MY, Chiu HC, et al. (2010) Chronic kidney disease care program improves quality of pre-end-stage renal disease care and reduces medical costs. Nephrology (Carlton) 15(1): 108-115.
- Johns TS, Yee J, Smith Jules T, Campbell RC, Bauer C (2015) Interdisciplinary Care Clinics in chronic kidney disease. BMC Nephrol 16: (1).
- Frankel A, Haraden C, Federico F, Lenoci Edwards J (2017) A Framework for Safe, Reliable, and Effective Care. White Paper. Cambridge, MA: Institute for Healthcare Improvement and Safe & Reliable Healthcare.
- Tan TC, Zhou H, Kelly M (2017) Nurse-Physician Communication - An Integrated Review. J Clin Nurs 26(23-24): 3974-3989.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.