Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Critical Hypokalemia: A Complex Clinical Journey
*Corresponding author: Leonard Ranasinghe MD, Professor of Emergency Medicine and the Director of the Fourth-Year Medical students, California Northstate University College of Medicine, Elk Grove, California, USA.
Received: October 26, 2023; Published: November 14, 2023
DOI: 10.34297/AJBSR.2023.20.002728
Abstract
Hypokalemia, characterized by low potassium levels in the blood, is a condition that can have severe consequences for patients, including cardiac arrhythmias and muscle weakness. Extreme hypokalemia, although rare, can lead to paralysis, cardiac arrest, and even death. The purpose of this project is to better understand hypokalemia, its presentation, and how it impacts different organ systems in the body. We will do this by analyzing a unique case of extreme hypokalemia. We will provide a concise framework for managing patients with similar presentations.
Keywords: Severe hypokalemia, Diuretics, Electrolyte imbalance
Introduction
Hypokalemia is a common presenting condition in which serum potassium levels are lower than normal, defined as less than 3.5mEq/L. Most patients with hypokalemia have mild to moderately low potassium levels and do not present as critically ill. Severe hypokalemia affects how electrical signals are transmitted in the body and is often life-threatening. Hypokalemia may present with nonspecific symptoms including but not limited to heart palpitations, constipation, fatigue, hypotension, lightheadedness, arrhythmias, polyuria, polydipsia, muscle weakness, spasms, twitches, and cramps [1].
Case Presentation
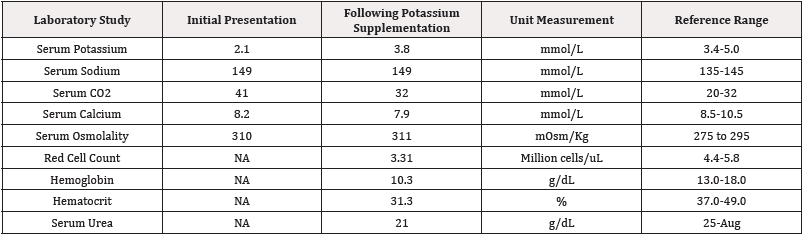
Table 1: Blood test result on initial presentation and following potassium supplementation.
IG: intervention group; CG: control group
This patient is a 71-year-old male with a history of hypertension, stage 3CKD, MGUS, and recurrent hypokalemia. The patient presented to the Emergency Department after his primary care physician, and cardiologist advised him to go to the emergency room when his potassium level fell to 1.8mmol/ L (normal 3.4-5.0mmol/L). The patient denied any symptoms, including chest pain, weakness, dizziness, and heart palpitations. In addition, he had moderate hypertension. EKG performed in the Emergency Department showed peaked T waves and prolonged QTc, with occasional PVCs. Otherwise, the EKG indicated a normal rate and sinus rhythm. The patient reported that he was started on the diuretic hydrochlorothiazide (12.5 mg once a day) and had increased urgency to urinate. Physical exam indicated that the patient was alert and oriented times 4, with no focal neurological deficits, S1/S2 heart sounds heard, regular rate and rhythm, no jugular venous distention, and no other notable pertinent findings during his presentation at the emergency department (Table 1).
A clinical concern for hypokalemia secondary to hydrochlorothiazide use was suspected thus, the medication was discontinued, and the patient was started on intravenous potassium. The patient was admitted to telemetry with continued potassium supplementation and repeat labs to assess his electrolytes. Upon further assessment, hydrochlorothiazide was discontinued. After being in telemetry for four nights his potassium was stabilized, and the patient was discharged. He was discharged with 20mEq of potassium, four times a day for four weeks. Additionally, he was advised not to continue taking the hydrochlorothiazide following his discharge with plans to follow up with his cardiologist and an outpatient nephrology consult.
Discussion
Hypokalemia is a medical condition characterized by low levels of potassium in the blood, defined as less than 3.5mEq/L, which can lead to various clinical manifestations such as muscle weakness, cramping, and cardiac arrhythmias [2]. Electrolyte imbalances may present with nonspecific symptoms, including but not limited to heart palpitations, constipation, fatigue, hypotension, lightheadedness, polyuria, polydipsia, spasms, and twitches [3]. This condition affects how electrical signals are transmitted in the body and heart and severe hypokalemia can be life-threatening. Hypokalemia is more common in hospitalized patients. However, it is still an important differential diagnosis for emergency department physicians. Several studies have investigated hypokalemia’s role in exacerbating electrolyte imbalance, its risk factors, and diagnostic approaches [4,5]. For instance, a study found that among hospitalized patients hypokalemia was present in 51.6% of cases, with older age, chronic kidney disease, and the use of diuretics significantly associated with its development [4]. Furthermore, another study revealed that Electrocardiogram (ECG) changes, such as ST-segment depression and T-wave inversion, were frequently observed in patients with hypokalemia, highlighting the importance of ECG monitoring in diagnosing and managing the condition [5] (Figure 1).
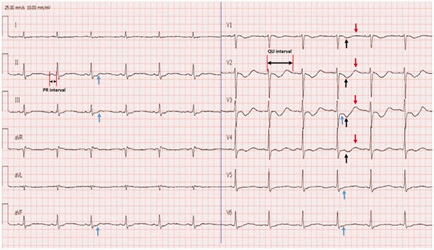
Figure 1: ECG of hypokalemic patient.
Note*: black arrows indicate T wave inversion. Blue arrows indicate ST depression [5].
Hypokalemia has substantial implications for patient outcomes and requires prompt recognition and appropriate interventions. Extreme hypokalemia is rare. Severe hypokalemia often presents with paralysis, cardiac arrest, and may lead to death if urgent medical attention is not provided [6]. However, in this case, the patient presented with no obvious symptoms, highlighting that symptoms alone are not a sufficient marker of clinically significant hypokalemia. Several studies have documented extreme hypokalemia’s incidence and clinical implications [1,7]. A previous study reported that severe hypokalemia, defined as potassium levels below 2.5mEq/ L, was associated with a 2.7-fold increase in mortality risk among hospitalized patients [1]. Similarly, a separate study found that extreme hypokalemia was a common complication among patients with renal tubular acidosis and was associated with poor outcomes [7]. This case was important due to its severity, with the patient’s potassium level upon hospital arrival at a low of 1.8mmol/L. Additionally, discerning the potential etiology of the patient’s hypokalemia, whether medication-induced or kidney or endocrine disease complications, added a layer of complexity in optimizing this patient’s treatment. Currently, the standard for treating hypokalemia is based on close monitoring of serum potassium levels to guide adjustments in intravenous potassium dosing. Failure to address the etiology of hypokalemia after potassium replacement may lead to recurrent episodes and adverse outcomes [8]. For example, a study demonstrated that potassium depletion caused by diuretic therapy could result in severe hypokalemia, particularly among patients with heart failure [9]. Another study reported that hypokalemia induced by laxative abuse could lead to severe muscle weakness and rhabdomyolysis [10].
The most probable cause of hypokalemia seen in this patient is secondary to hydrochlorothiazide use. Hydrochlorothiazide is a widely used blood pressure medication that acts on the distal convoluted tubules, inhibiting the sodium chloride cotransporter, thus having a diuretic effect and loss of potassium in the urine [11]. Discontinuing this medication, immediately starting intravenous potassium supplement, and discharging the patient with oral potassium supplementation was the most appropriate treatment. However, it has been found that the use of low-dose hydrochlorothiazide can prevent cases of hypokalemia from occurring [12]. Upon examining the effects of hydrochlorothiazide on potassium levels, it was found that the high dose of 122.5mg produced a mean 0.7mEq/L reduction in serum potassium while the low dose of 12.5mg caused no change, with both producing significant reductions in diastolic blood pressure [12]. These findings make it possible to restart low-dose hydrochlorothiazide treatment when potassium levels are stabilized. This patient’s current medications were lisinopril (40mg daily), terazosin (5mg every evening) and hydrochlorothiazide (12.5mg daily). Lisinopril and hydrochlorothiazide can have opposing effects on potassium levels, with lisinopril increasing potassium levels and hydrochlorothiazide decreasing them.
When evaluating a patient with severe electrolyte abnormalities such as severe hypokalemia, on a prescribed diuretic, it is important to understand its indication and whether potassium-sparing diuretics are more appropriate. This includes ensuring medication compliance through quality longitudinal care outside of the emergency room and confirming the medication name, indication, and dosage in the medical record. To discharge a patient with confidence, understanding the medication indication, adherence, and patient comprehension is key. Ultimately, close outpatient follow-up and a partnership with the patient’s primary care provider and outpatient specialists are imperative to ensure complete understanding of the patient’s diagnoses and medical decision making for further management. Continued treatment of this patient in the hospital with other anti-hypertensive drugs, with an emphasis on correct dosing, as discussed, and consideration of his serum electrolyte abnormalities, adds to a treatment framework based on rapid improvement of serum potassium levels being the top treatment priority to prevent other medical complications. This approach aims to minimize discontinuing any of the patient’s medications. This adds to the complexity of weighing appropriate treatment options.
This case being secondary to medication use allows us to start initial treatment by immediately discontinuing the medication causing the electrolyte abnormality. However, treatment approaches aimed at stopping the medication causing hypokalemia may easily lead to supplementing potassium to the point of overshooting potassium levels, creating a hyperkalemic status. Repeated monitoring of potassium and other electrolyte levels adds a layer of difficulty when treating hypokalemia. Managing hyperkalemia can become complicated by numerous variables. One of the most prominent ones is the inverse relationship between sodium and potassium. Due to this, it is crucial to monitor sodium and other electrolyte levels when treating hypokalemia and vice versa. Another possible complication that may arise when attempting to adjust potassium levels are rebound electrolyte disturbances [13]. Specifically, treating hyperkalemia with a potassium binder can potentially dramatically decrease the potassium level under the normal range or disturb another electrolyte level [14]. While potassium binders oftentimes exchange sodium for potassium, such as with sodium polystyrene sulfonate (Kayexalate [SPS]) and sodium Zirconium Cyclosilicate (ZS-9) [14], there are other binders that use a different mechanism. Patiromer, for example, exchanges calcium for potassium instead of sodium [15].
With potassium, sodium, and calcium being three essential electrolytes, it is crucial to pay attention to all those levels to initiate appropriate treatment for hypokalemia without disturbing another electrolyte [16]. This case provides a framework for managing future patients with a similar presentation. Two factors that complicated this patient’s treatment were the severity of the hypokalemia and its reoccurring nature. Both factors may increase the risk for morbidity and mortality [1]. Understanding that this patient’s hypokalemia had a probable etiology of medication side effects allows us to highlight the need for a thorough medication review as a basis for standard treatment of extreme hypokalemia. Repeated monitoring of patient serum potassium levels is equally important to take into consideration and should be the basis for standard of care in these cases. Addressing underlying medical conditions and hospital-based complications is additionally imperative for optimal patient outcomes. Specifically, current practice has placed an emphasis on subsequent serum potassium testing, suggesting that a delay in time to subsequent testing has an impact on in-hospital mortality. Additionally, the achievement of normokalaemia is a good prognostic indicator of positive patient outcomes [8]. The pattern of potassium level testing, which was four times during his four-day hospital stay in our case in addition to the achievement of normokalaemia with a potassium level at discharge of 3.8mmol/L, has been found to be linked to adequate clinical management in extreme hypokalemia [8].
Conclusion
Hypokalemia is a medical condition that may result in poor patient outcomes. Extreme hypokalemia, while rare, is a serious complication requiring prompt recognition and management. Through extensive research, various studies have investigated the prevalence, risk factors, diagnostic approaches, underlying mechanisms, and clinical implications of hypokalemia and extreme hypokalemia. Understanding the underlying causes and consequences of extreme hypokalemia is critical for this condition’s timely diagnosis and management. This case report aims to contribute to the existing body of knowledge on how to manage, recognize, and treat potassium deficiency by documenting this case of severe hypokalemia. Ultimately, managing electrolyte imbalance disorders, such as in this patient’s presentation, is crucial to recognize hypokalemia in the broader field of emergency medicine, ultimately improving patient care and outcomes.
Acknowledgements
None.
Conflict of Interest
None.
References
- Thongprayoon C, Cheungpasitporn W, Hansrivijit P, Mao MA, Medaura J, et al. (2019) Admission Serum Potassium Levels in Hospitalized Patients and One-Year Mortality. Medicines (Basel) 7(1): 2.
- Palmer Biff F (2011) Metabolic complications associated with use of diuretics. Semin Nephrol 31(6): 542-552.
- Kardalas E, Paschou SA, Anagnostis P, Muscogiuri G, Siasos G, et al. (2018) Hypokalemia: a clinical update. Endocr Connect 7(4): R135-R146.
- ÇETİN, Şirin (2021) A study on factors impacting length of hospital stay of COVID-19 inpatients. J Contemp Med 11(3): 396-404.
- Wang X, Han D, Li G (2020) Electrocardiographic manifestations in severe hypokalemia. J Int Med Res 48(1): 300060518811058.
- Castro D, Sharma S (2023) Hypokalemia.
- Kittrawee Kritmetapak, Sadudee Peerapornratana, Nattachai Srisawat, Nicha Somlaw, Narisorn Lakananurak, et al. (2016) The impact of macro-and micronutrients on predicting outcomes of critically ill patients requiring continuous renal replacement therapy. PLoS One 11(6): e0156634.
- Clegg DJ, Cody M, Palmer BF (2017) Challenges in treating cardiovascular disease: Restricting sodium and managing hyperkalemia. Mayo Clin Proc 92(8): 1248-1260.
- Bowling CB, Pitt B, Ahmed MI, Aban IB, Sanders PW, et al. (2010) Hypokalemia and outcomes in patients with chronic heart failure and chronic kidney disease: findings from propensity-matched studies. Circ Heart Fail 3(2): 253-260.
- Mansour R, Mandiga P, Thigpin D (2019) Hypokalemia-Induced Rhabdomyolysis from Budesonide Therapy in Crohn's Disease. ACG Case Rep J 6(8): e00201.
- McKenney JM, Goodman RP, Wright JT, Rifai N, Aycock DG, et al. (1986) The effect of low‐dose hydrochlorothiazide on blood pressure, serum potassium, and Lipoproteins. Pharmacotherapy: 6(4): 179-184.
- Viera AJ, Noah Wouk (2015) Potassium Disorders: Hypokalemia and Hyperkalemia. Am Fam Physician 92(6): 487-495.
- Paltiel O, Salakhov E, Ronen I, Berg D, Israeli A (2001) Management of Severe Hypokalemia in Hospitalized Patients: A Study of Quality of Care Based on Computerized Databases. Arch Intern Med 161(8): 1089-1095.
- (2016) Patiromer (Veltassa) for hyperkalemia. Med Lett Drugs Ther 58(1488): 23-24.
- Fijorek K, Püsküllüoğlu M, Tomaszewska D, Tomaszewska R, Anna Glinka, (2014) Serum potassium, sodium and calcium levels in healthy individuals - literature review and data analysis. Folia Med Cracov 54(1): 53-70.
- Herman LL, Bashir K (2023) Hydrochlorothiazide.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.