Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Economic Burden of Malaria and Bilharziasis in Cote D’ivoire: Cases of Households in the City of Korhogo
*Corresponding author: Kouakou Kouadio Clément, Université Félix Houphouët Boigny de Cocody, Cote d’Ivoire.
Received: November 23, 2023; Published: December 04, 2023
DOI: 10.34297/AJBSR.2023.20.002752
Summary
This work evaluates the cost of treating malaria and/or bilharzia in households in Korhogo. As part of our study, data were collected from 728 households in the town of Korhogo on the characteristics (income, consumption, health expenditure, etc.) of households and patients with malaria and/or bilharzia. Statistical analyzes were carried out to analyze the shares of malaria and/ or bilharzia expenditure in health expenditure and total household expenditure in Korhogo. A logistic model was used to identify the determinants and effects of the burden of these two diseases in households in Korhogo town. The results show that in terms of therapeutic choices, modern medicine is the first resort used over self-medication even if the prices of modern medicine drugs are four to five times more than those of traditional medicine. Expenditure on the treatment of malaria and/or schistosomiasis represents the majority of household health expenditure and around a quarter of consumption expenditure. Poor households are the most vulnerable to these diseases.
JEL Classification: I11, I12, I14, I15,
Introduction
Climate warming, accentuated by anthropogenic activities, has harmful effects on humans, particularly on their health. In its report on world health in 2002, the World Health Organization (WHO) shows that in 2000 climate change was responsible for 2.4% of cases of diarrhea in the world and 6% of cases malaria in some middle- income countries. Also, the WHO specifies that the spatio-temporal distribution of vector-borne diseases should expand due to more favorable temperatures, which would lead to changes in the dynamics of communicable diseases. These different modifications amplify the risks of exposure to vector-borne diseases such as malaria and bilharzia [1] which are “water-dependent” conditions representing the two leading global parasitic endemics [2]. These two parasitic conditions occur in various eco-geographic environments including the arid and semi-arid zones of the northern and southern fringes of the Sahel band and mainly affect people in Africa south of the Sahara.
Malaria is a parasitic disease requiring a vector [3]. The parasite is a Plasmodium protozoan and the vector is the female Anopheles insect. The disease is transmitted by a bite from the female Anopheles mosquito (mainly between sunset and sunrise), whose reproduction requires blood, water and heat. Endemic in 104 countries, malaria is one of the main global public health problems weighing on economies [4] and the population at risk is estimated at 3.4 billion [5], or % of the 2014 population.
In 2012, malaria caused 627,000 deaths (a margin of uncertainty between 473,000 and 789,000) with 90% recorded in Africa [6], mostly among children. In endemic African countries, malaria represents 25 to 35% of consultations, 20 to 45% of hospital admissions and 15 to 35% of hospital deaths. Master 2 thesis in Economics 2nd of development specialty health economics By BALLE Ando Honorate Larissa While malaria is a disease that can be perfectly prevented and treated, its transmission continues to progress throughout the world, and constitutes a very heavy burden, particularly for sub-Saharan African countries.
Bilharzia, also called schistosomiasis, is a chronic disease caused by parasitic worms (trematodes) of the genus Schistosoma. Infection occurs when parasite larvae, released by freshwater gastropods, enter a person’s skin through contact with infested water. There are two main forms of schistosomiasis: intestinal and urogenital. Bilharzia can cause severe acute infections and unusual problems up to paralysis. In 2011, more than 243 million people needed treatment for bilharzia. But only 28.1 million people were treated with 90% of these people living in African countries and in particular in the poorest sections of the populations. Bilharzia causes more than 200,000 deaths per year in sub-Saharan Africa [6].
If Côte d’Ivoire and particularly the town of Korhogo was already exposed to these diseases due to its equatorial climate, the climate changes of recent years have favored their development.
In this city, Malaria and Bilharzia exist with varying levels of endemicity. The prevalence of malaria from hospital sources was around 37% in 2011. Regarding Bilharzia, this region has an average prevalence of nearly 30% [7-9].
Malaria and bilharzia have an impact on household living conditions, particularly when individuals are continually exposed to them. And according to the theory of human capital, a deterioration in the state of health has repercussions on the productivity of the active population and therefore on production, wages and income [10,11]. Thus, investments in health have direct effects on productivity, and therefore on economic growth. This situation then justifies the intervention of public or private organizations to fight against these two diseases.
In Côte d’Ivoire, despite the creation of national programs to combat these two diseases, the management of malaria and bilharzia remains a burden for households, particularly those in the town of Korhogo for whom access to health services health can come at the expense of other essential goods and services.
This situation justifies the present study which focuses on the assessment of the economic burden represented by malaria and schistosomiasis for households in the town of Korhogo. It aims to provide answers to the following research question: What is the impact of the cost of treating malaria and bilharzia on the living conditions of households in the town of Korhogo. More specifically:
a) What are the costs of seeking care in the event of malaria and/or bilharzia in households in Korhogo?
b) What are the therapeutic routes for households in Korhogo in the event of Malaria?
c) What are the effects of health expenditure for malaria and bilharzia on the living conditions of households in Korhogo?
Determining the Economic Burden of Disease
The economic burden is calculated using the methodology proposed by the World Health Organization (WHO) to determine catastrophic health expenditure. According to this, a household faces catastrophic expenditure if its total health expenditure is greater than or equal to 40% of its capacity to pay, capacity calculated from total expenditure and food expenditure adjusted to the size of the household. household. In our case, these are direct health payments in the event of malaria and/or Bilharziasis which must not exceed 40% of the households’ ability to pay. The different variables used to calculate catastrophic expenses in the event of malaria are:
Direct Payments for Malaria and/or Bilharzia (oop)
Direct payments refer to payments made by households when they use health services in the event of the occurrence of these diseases.
Household Consumption Expenditure (exp)
Household consumption expenditure includes monetary payments and in-kind expenditures for all goods and services, as well as the value of self-consumption.
Food Expenditure
Household food expenditure corresponds to the amount spent on all types of food by households, plus the value of family production that is consumed by the household.
The Poverty Line and Household Living Expenses
Household living expenses correspond to the minimum amount required to maintain a basic standard of living in society. The poverty line used in the analysis corresponds to living expenses. The poverty calculation method will be done using a poverty threshold based on basic food expenses to estimate the living expenses required by a household.
Household Ability to Pay (ctp) and Out-of-Pocket Payment Burden (oopctp)
A household’s ability to pay corresponds to a household’s non-subsistence expenses. However, some households may have food expenses below their living expenses. This indicates that these households have expenditures below the poverty line calculated for the country. This can happen, for example, when food expenses declared in the survey do not take into account subsidies, vouchers, self-consumption.
Catastrophic Health Expenses (Catastrophic)
A household faces catastrophic expenses when its out-of-pocket health payments are greater than or equal to 40% of its ability to pay, or in other words, its living expenses. This 40% threshold may change depending on the situation in the country considered. In the case of our study, we will use this threshold. The variable to designate catastrophic health expenditure is constructed as a dummy variable, which takes the value 1 when the household has faced catastrophic expenditure and the value 0 when the household has not faced catastrophic expenditure.
Impoverishment (impoor)
A non-poor household is impoverished by health payments when it falls below the poverty line after making these payments. The impoor variable takes the value 1 if a household is impoverished, and 0 otherwise: impoorh = 1 if exph ≥ seh and exph–ooph < seh impoorh = 0 otherwise.
Data Collection
As part of a transdisciplinary framework, the study required the collection of economic, sociological, anthropological, bio-statistical, entomological and parasitological data. Our data come from a cross-sectional survey with a representative sample drawn at three stages from urban households in the city of Korhogo.
The sampling frame is the General Population and Housing Census file (RGPH98) which provided us with the list of Enumeration Areas (ZD) and the number of households in the city of Korhogo by district.
Data collection lasted 12 days and took place from June 15, 2014 to July 27, 2014 following a random drawing of 728 households in the town of Korhogo. The three (03) degree sample was drawn as follows:
a) At first level we drew 29 districts of the city of Korhogo.
b) At the second level, we made an allocation of the ZDs proportionally to the number of households in the neighborhoods.
c) At the third stage, in each ZD drawn, 13 randomly selected households were surveyed.
Assessment of Treatment Costs and Analysis of the Burden of Malaria and Bilharzia in Korhogo Households
Therapeutic itineraries and cost of treatment in the event of Malaria and/or Bilharzia. Out of a total of 728 households studied, 38% of them claimed to have had at least one (1) member of their household become ill with malaria and/or bilharzia during the selected periods. We were able to register 602 patients including 596 cases of malaria and 6 cases of Bilharzia. These different patients returned to households as follows:
a. 272 households with cases of malaria patients.
b. 3 households with cases of Bilharzia patients and
c. 3 households with cases of Malaria and Bilharziasis patients.
The main recourse for patients is the hospital (53.0%), followed by self-medication with drugs (18.3%). Recourse to a healer or a traditional practitioner as first choice in the event of illness is very low. Only 2.3% of patients studied use these remedies as their first choice for treatment.
By grouping the remedies into three categories depending on the type of treatment: Modern medicine (hospital, clinic, private dispensary, private practice, informal practice, nurse or doctor in the informal sector), traditional medicine (recourse to a healer, recourse to a traditional practitioner) and self-medication (self-medication with plants and self-medication with medications), we note that:
Modern medicine is the first resort used by most patients (63.6%) but only 1 in 3 Bilharzia patients use it as their first resort. Approximately a third (30.9%) of patients use self-medication as their first choice of care, with specifically half (50.0%) of Bilharzia patients preferring this remedy as their first choice of care. As for traditional medicine, it attracts far fewer patients (2.3%) than self-medication and modern medicine.
If Bilharzia patients are generally satisfied from their first use of care, 10.1% of malaria patients had recourse to a second therapeutic choice. Among these patients, 63.3% had previously chosen self-medication but given the persistence of malaria, they turned to other therapeutic choices. 16.7% of patients had also initially preferred the care of modern medicine but subsequently chose to treat themselves with traditional medicine or self-medication with plants. It goes without saying that the costs of analyses, medications and consultations have contributed to the abandonment of modern medicine (Table 1).
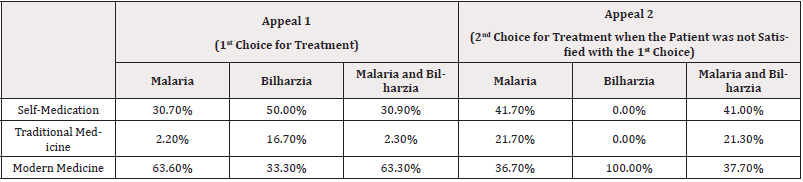
Table 1: Distribution of patient care recourses in the event of malaria and/or Bilharzia.
*Source: Survey data and our calculations
In Korhogo, the average household health care expenditure is 13,055 FCFA per month. The cost of recourse in the event of malaria and/or Bilharzia represents the majority of health expenditure (83.4%) for these households. Indeed, for 73.5% of households having incurred expenses for malaria and/or bilharzia care, the costs of this care represent their entire health expenditure. The average direct cost of household health expenditure for modern medicine is 24,640 FCFA in the case of malaria and 16,000 FCFA in the case of bilharzia. In addition, the average costs of consultation and medication when using modern medicine are higher than those of traditional medicine. For traditional medicine, the average direct cost of care is 4,000 FCFA for malaria and 2,000 FCFA for bilharzia.
As for the cost of self-medication, the direct costs of care are approximately equal to the cost of traditional medicine, 4,130 FCFA for malaria and 2,000 FCFA for bilharzia.
The costs of illnesses are widely different depending on whether it is traditional medicine, modern medicine or self-medication (Table 2).

Table 2: Cost of recourse in the event of malaria and/or Bilharzia.
*Source: Survey data and our calculations
These pathologies, in addition to the direct costs noted above, have affected households through indirect costs. Thus 59.0% of patients stated that the disease had a negative impact on their activity. Indeed, during the period of illness, individuals who carry out a paid activity based on the days of activity, such as commerce, not only lose money because of their condition but are also obliged to use their savings to pay for themselves. cure. The average number of days of activity lost by patients is 9 days.
Some patients (56.0%) also stated that the impact of the disease was manifested through the activities of members of their household. In reality, for very young patients, one member or several members of the household stop carrying out their activities for the duration of the illness to take care of them.
Conclusion
Malaria, although a major health and development problem, has been the subject of little research devoted to the economic burden aspect. Our study, which adds a stone to the building, shows that Malaria and/or Bilharzia patients from households in Korhogo do not turn to traditional medicine as a first resort but rather to modern medicine followed by self-medication, Two out of three patients choose to turn to modern medicine and only 2.4% of patients resort to treatment using traditional medicine. This can be explained by the implementation of health policies to take care of cases of patients, particularly malaria. This idea finds its extension in the perception of patients who affirm at 89.3% that modern medicine is more effective for this type of care. Households in this case are ready to afford care for malaria and/or bilharzia which represent the majority of household health expenditure (83.4%). Households that resort to self-medication or modern medicine have a greater chance of being in a situation of malaria burden than households that have no recourse in the event of illness. This is perfectly explained since when the individual has no recourse, he does not spend while the cost of self-medication can be explained by the fact of trying several medications, which increases expenses.
In particular, malaria is the main reason for household health care expenditure. Also, health expenses in the event of Malaria constitute a burden for 20.2% of households in Korhogo who have incurred healthcare expenses. Specifically, out-of-pocket payments for malaria care constitute a real burden for one in four poor households. The risk of being in a situation of economic burden from Malaria is in fact greater among poor households.
Paradoxically, the relative result of the reduction in the risk of household exposure to the burden of Malaria when the size of the household increases can be interpreted by the contribution to the expenses of the different members of the household. Looking more closely, especially taking into account the specificities of households, it becomes obvious that when the size of the household is high, contributions to general expenses decrease given the fact that these households are often polygamous and composed of distant relatives who most of the time do not approach the head of household in the event of illness.
Concerning the number of patients which has an effect on the burden of illness, this is obvious because the unit cost per patient, aggregated at the household level, increases household expenses proportionally.
Acknowledgement
None.
Conflict of Interest
None.
References
- Kumaresan Jacob, Sathiakumar Nalini (2010) Climate change and its potential effects on health: a call for integrated action. Bull World Health Organ 88(3): 163.
- Hotez Peter J, Kamath Aruna (2009) Neglected Tropical Diseases in Sub-Saharan Africa: Review of Their Prevalence, Distribution, and Disease Burden. PLoS Negl Trop Dis 3(8): e412.
- Gentilini (1993) Tropical Medicine. Flammarion, 4th edition, Paris, pp. 635.
- Sachs J, Malaney P (2002) The economic and social burden of malaria. Nature 415: 680-685.
- WHO (2014) Report on World Health Statistics.
- WHO (2013) Schistosomiasis: Status Report 2001-2011 and Strategic Plan 2012-2020, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland.
- Kouakou J (2000) Situation of schistosomiasis in Côte d' In: Chippaux JP (ed.): The fight against schistosomiasis in West Africa. Paris, IRD, Coll. Colloques et Séminaires.
- Yapi Y, OJT Briët, S Diabate, P Vounatsou, E Akodo, et al. (2005) Rice irrigation and schistosomiasis in savannah and forest areas of Côte d' Acta Trop 93(2): 201-211.
- Cecchi P, Baldé S, Yapi YG (2007) Intermediate host molluscs for schistosomiasis in small dams. In: Sharing water. The small dams of Côte d'Ivoire (ed.) Cecchi P, Latitudes 23. Paris: IRD Editions pp. 175-189.
- Becker Gary S (1965) A Theory of the Allocation of Time. Economic journal pp. 493-517.
- Grossman M (s.d.) On the Concept of Health Capital and The Demand for Health. Journal of Political Economy 80(2): 223-255.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.