Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Enhancing the Family Physician Competency in Epidemic management through Continuous Medical Education and (CME) and Continuous Professional Development (CPD)
*Corresponding author: Maka Kurashvili, PhD student of Public Health Doctoral Program, The University of Georgia, Georgia.
Received: September 21, 2023; Published: September 29, 2023
DOI: 10.34297/AJBSR.2023.20.002685
Abstract
Epidemics and pandemics pose significant challenges to public health systems worldwide, underscoring the pivotal role of family physicians in epidemic management and prevention. This article explores the roles and imperative of enhancing family physician competency in epidemic management through Continuous Medical Education (CME) and Continuous Professional Development (CPD). The literature review discusses the critical role of family physicians in early detection, diagnosis, treatment, and prevention of epidemic outbreaks. Various modes of CME and CPD, such as conferences, workshops, online courses, and peer learning, are explored in the context of their efficacy in enhancing family physician competency. Challenges and barriers to accessing CME and CPD are analyzed, including time constraints, financial limitations, and access to resources. Recommendations are offered to overcome these challenges and promote a culture of lifelong learning among family physicians; offer a variety of CPD opportunities to cater to the diverse needs and preferences of family physicians; Healthcare institutions should provide financial support, grants, and incentives to participate in CPD and CME activities; Provide flexible scheduling options for CPD activities, allowing them to balance their professional responsibilities with their learning goals; Encourage family physicians to collaborate and share their experiences and knowledge with peers; Peer learning can be a valuable component of CPD, facilitating the exchange of best practices and innovative approaches to epidemic management; Regularly evaluate the impact of ongoing education on family physician competency. In conclusion, this article underscores the indispensable role of Continuous Medical Education (CME) and Continuous Professional Development (CPD) in equipping family physicians with the knowledge and skills necessary for effective epidemic management. It advocates for increased investment and support for family physician training, emphasizing that a well-prepared healthcare workforce is essential for safeguarding public health in the face of epidemic threats.
Keywords: Family physician, CME, CPE, Pandemic preparedness
Abbreviations: CME: Continuous Medical Education; CPD: Continuous Professional Development
Introduction
The world is no stranger to the recurrent challenges posed by epidemics and pandemics. The past century alone has witnessed the devastating consequences of infectious diseases, from the Spanish flu of 1918 to the more recent COVID-19 pandemic. In the face of such global health threats, the healthcare community, and in particular, family physicians, plays a pivotal role in epidemic management and prevention. Family physicians serve as the frontline guardians of community health [1]. Public health reports, including those following SARS and H1N1, outline the goals for primary care pandemic response plans (egg, contribute to screening, testing, treating, surge capacity, and vaccination), but do not explicitly include actionable plans describing family physician roles [2-4]. They are often the first point of contact for individuals seeking medical care, making them uniquely positioned to detect, diagnose, and mitigate the spread of infectious diseases. The critical role of family physicians in epidemic control cannot be overstated, as they bridge the gap between patients and public health interventions to effectively respond to these challenges, family physicians must continually update their knowledge, skills, and practices [3]. This imperative for lifelong learning forms the foundation of Continuous Medical Education (CME) and Continuous Professional Development (CPD). In Georgia, unlike other medical specialties, family doctors are not obligated to participate in Continuous Medical Education (CME) and Continuous Professional Development (CPD) programs. A doctor’s certificate in family medicine is permanent [5]. The aim of our investigation was to study the role and functions of family physicians in the management and prevention of epidemics in Georgia. The article presents a fragment of the results from the doctoral research project titled ‘Primary Health Care: The Multifunctional Role of Family Doctors in Epidemic Management and Prevention.’ This research is conducted as part of the Public Health Doctoral Program at the School of Health Sciences, University of Georgia. An important part of the research was devoted to the collection and further analysis of the information about CME and CPD of family doctors.
Specifically, we investigated the following aspects: Doctor’s Perspectives on CME and CPD; The opinion of doctors regarding CME and CPD; Frequency of their participation in educational and professional workshops and trainings; Their activities to prevent the diseases in general and SARS Cov-2 virus infection; Use and attitude of IT technologies; Their participation in the patient education in general and during the COVID- pandemic. This article based on original research as part of doctoral research project and explores the essential relationship between CPD, CME and epidemic management in the realm of family medicine. It delves into the evolving health care landscape and highlights the necessity for family physicians to embark on a journey of lifelong learning to respond effectively to emerging health crises. Throughout this exploration, we examined the critical role family physicians play in early detection, containment, and prevention of epidemic outbreaks. We delved into the diverse modes of CME and CPD available to family physicians, exploring their efficacy in enhancing competency. We addressed the challenges and barriers faced by these healthcare professionals in accessing ongoing education and provided recommendations to overcome these obstacles. Future pandemic plans require greater integration of primary care to ensure the delivery of an effective and coordinated pandemic response. Strengthening pandemic preparedness requires a broader reconsideration and better understanding of the central role of primary care in health system functioning [6].
Study Design and Methods
The research was conducted in primary healthcare settings in Tbilisi, Georgia. We conducted a cross-sectional study, utilizing a special structured questionnaire, among family doctors, patients, and primary healthcare setting managers. By analyzing the responses to the questionnaire, we were able to investigate the role of Continuous Medical Education (CME) and Continuous Professional Development (CPD) among family doctors in patient healthcare during epidemics. The presented research has yielded significant results, conclusions, and recommendations concerning CME and CPD for family doctors. A total of 298 family doctors (n=298) from 35 primary healthcare settings, 396 beneficiaries (n=396) of the same centers, and 17 primary healthcare managers (n=17) participated in the study. We explored the attitudes of family doctors and primary healthcare managers regarding this issue through in-depth interviews.
Statistics
Data were treated using the software SPSSv.22.0 (Chicago, Illinois, USA). Categorical parameters are presented by percentages. Statistical significance was assessed by the Chi2-test. p<0.05 was considered as the criterion of statistical significant significance of the studied parameters.
Results
Doctors aged 51-60 and > 60 years were significantly more prevalent among different age groups of family doctors (67.1%; Chi2=55.74, df=3, p<0.001). 99.3% of the family doctors who participated in the study were certified (Chi2=290.05, df=1, p<0.001). Family doctors with 10 years or more of experience significantly prevailed (90.9%; Chi2=445.01, df=2, p<0.001). 89.0% of family doctors who participated in the study serve more than 1000 beneficiaries (Chi2=205.11, df=3, p<0.001); daily load of 91.6% family doctors was more than 10 patients (Chi2=110.26, df=2, p<0.001). Analyzing the frequency of participation of family doctors in educational and professional events, it was found that there were significantly more doctors who were at least partially familiar with CME and CPD programs for family doctors (97.7%; Chi2=301.01, df=2, p<0.001 (Figure1).

Figure 1: Distribution of the responses to the question Q9 - “How often do you get acquainted with educational programs for family doctors?” (n=298).
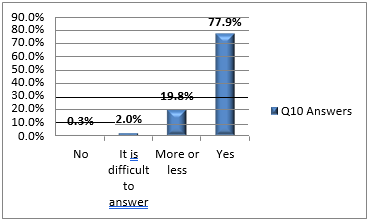
Figure 2: Distribution of the responses to the question Q10 - “Do you keep up with medical news through medical journals and articles?” (n=298).
There was high prevalence of the doctors who were at least partially informed about the medical news through medical journals and scientific articles (97.7%; Chi2=471.69, df=3, p<0.001; Figure 2). Additionally, there was high prevalence of the doctors who were at least partially informed about updated guidelines and protocols for diagnosing and treating diseases through websites (99.0%; Chi2=427.66, df=2, p<0.001).
The results of analysis showed a significant number of doctors interviewed in the survey about the main functional role of the family doctor. The reason for patient referral to the family doctor was obtaining the permission for the referral to another doctor-specialist, which definitely does not correspond to the functional role of the family doctor (93.0%; Chi2=127.34, df=2, p<0.001).
The responses from family doctors regarding patient services during the epidemic were particularly interesting. A clear majority of doctors noted a significant increase in patient adherence (68.4%; Chi2=319.18, df=3, p<0.001). There was significant high prevalence of the family doctors who answered that the hospitalization cases did not increase in the beneficiaries with chronic diseases during COVID-19 (SARS-CoV- 2) pandemic (74.2%; Chi2=152.87, df=3, p<0.001). A significant number of physicians (76.2%) included in the study reported 10 or more phone consultations each day related to the COVID-19 infection.
The answers were obtained by more in-depth questions about the level of awareness of family doctors and about the hospitalization data of their own beneficiaries in the case of a diagnosed SARS-CoV-2 viral infection. The results showed that 38.6% of the respondents did not have information about the cases of hospitalization (Chi2 = 274.40, df=6, p< 0.001). 57.4% of respondents (Chi2=396.63, df=5, p<0.001) did not have information about cases of hospitalization of beneficiaries with confirmed COVID-19 SARSCoV- 2 bypassing the family doctor.
Of the respondents, 96.0% (Chi2 = 251.93, df=1, p<0.001) indicated that family doctors provided information about the need to vaccinate against COVID-19 (Figure 3). However, the immunization results were reported to be very low, with 73.8% of the same doctors confirming that slightly more than 10% of their beneficiaries had been vaccinated against COVID-19.
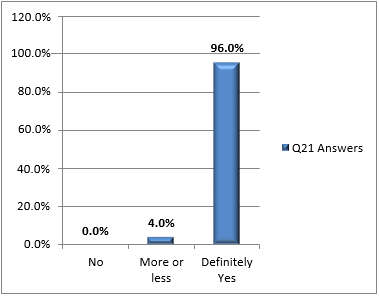
Figure 3: Distribution of the responses to the Q21 - “Did you provide your beneficiaries with the information about the need to vaccinate against COVID-19 (SARS-CoV-2)?” (n=298).
Very noteworthy results were obtained by the analysis of patient responses. Beneficiaries of 25-35- and 35-55-years’ age groups of same healthcare settings were mostly involved in the study (Chi2=109.29, df=3, p<0.001), mostly females (82.3% Chi2=165.49, df=1, p<0.001) and high educational level (University; 90.9%l Chi2=592.24, df=2, p<0.001).
The percentage of patients reporting daily contact with their family doctor was remarkably high (77.3%; Chi2=592.24, df=2, p<0.001). in contrast, the percentage of the patients reporting no contact with a family doctor or the percentage of the patients reporting daily contact with a family doctor was significantly lower (14.6%; Chi2=346.61, df=2, p<0.001). The number of patients who reported more than 3 visits to the family doctor during the year turned out to be remarkably low (37.3%; Chi2=108.08, df=3, p<0.001).
During the survey, we were interested in whether the time allotted for the patient consultation has changed due to the epidemic; The specified responses options included: the standard 15 minutes allotted for consultation, as well as 15-25 minutes and more than 25 minutes. The percentage of answers corresponding to the consultation time of 15-25 minutes prevailed significantly (52.5%; Chi2=113.15, df=2, p<0.001).
The percentage of patients reporting an increase in the number of the visits to the family doctor was significantly lower (23.7%), while 48.5% of respondents noted the same number of the visits (Chi2=41.88, df=2, p<0.001).
The percentage of patients who considered the information provided by the doctor about their diseases to be exhaustive was 56.1%. When we combine the number of patients who believed that doctors provided too little information about their diseases (17.7%) and/or preferred to check this information elsewhere (26.3%), a significant difference still remained (Chi2=96.42, df=2, p<0.001). We also asked a separate question to analyze patients’ opinions about the reliability of diagnoses made by family doctors. It was prevalent that a certain percentage of patients trusted their doctors (Chi2=100.06, df=2, p<0.001). However, when we combine those who do not trust doctors as much (10.1%) and the patients who engaged in verifying doctors’ diagnoses (40.9%) and compare it with the percentage of patients with complete trust (49.0%), we did not observe a significant difference.” According to the patients, the percentage of physicians providing the explanations of the need/importance of the prescribed laboratory and instrumental examinations significantly prevailed (76.8 %; Chi2=336.42, df=2, p<0.001).
In order to study the safety of medical treatment, we asked patients about their awareness about the expected side effects, discomfort or complications of prescribed medications or manipulations. According to the patients, the percentage of beneficiaries partially provided by the information about the side effects, possible complications and expected discomfort of the prescribed medications and/or manipulations from the family doctors was significantly high (58.6%; Chi2=127.27, df=2, p<0.001). The rate of doctors providing the complete information is quite low (28.3%).
The percentage of the patients satisfied with the professional level of the family doctor prevailed significantly (48.5%; Chi2=46.97, df=2, p<0.001). However, if we combine the percentages of the unsatisfied beneficiaries and the patients who had difficulty to answer, and compare it with the percentage of satisfied patients, null hypothesis was not rejected (non-significant difference). The percentage of patients who made a visit to a family doctor due to referral to another specialist is significantly high (73.2%). Taken alone, this response is indicative of very low confidence in the family physician. Analyzing the answers to selected questions to assess the preventive role of the family doctor, it was found that the percentage of beneficiaries who undergo preventive examinations is significantly high (52.5%; Chi2=51.52, df=3, p<0.001). However, if we combine the rates of patients who was not examined (11.6%) or rarely had preventive examinations (35.9%) and compare the rates of patients who have at least once a year such examinations (29.8%), the significant difference was no longer apparent. It was significantly high the percentage of patients who noted that the visit to the family doctor did not depend on the presence of seasonal viruses (60.1%; Chi2=130.24, df=2, p<0.001). It was also significantly high the percentage of non-fully vaccinated (anti-COVID-19 vaccine) patients (59.6%), and significantly low the percentage of fully-vaccinated patients (26.3%; Chi2=28.24, df=3, p<0.001). Significantly high was the percentage of non- -vaccinated (anti-seasonal flu vaccine) patients (66.1%), and significantly low the percentage of fully vaccinated patients (19.7%; Chi2=65.82, df=3, p<0.001). The percentage of patients who received comprehensive information about the need of vaccination against COVID-19 (SARS-CoV-2-) was 73.2% (Chi2=85.49, df=1, p<0.001).
The quality of patients’ satisfaction is indicated by the following result: the percentage of patients who recommended a friend, relative, or family member to register at their primary health care setting, in one way or another, 54.5%; Chi2=150.24, df=2, p<0.001) which prevailed. However, when we combine the patients who answered ‘No’ or had difficulty answering and compare them with the percentage of patients who agreed, the significant difference was no longer observed. The percentage of patients who expressed satisfaction at various levels with the quality of service provided by family doctors in the primary setting was significantly high (Chi2=46.71, df=1, p<0.001; Figure 4). However, when we combine the patients who were not satisfied and desired better services (‘unsatisfied’) and compare their number with the satisfied and very satisfied (‘satisfied’) patients, we observe that the percentage of ‘unsatisfied’ is significantly higher than the percentage of ‘satisfied’ (Figures 4,5).”

Figure 4: Distribution of surveyed patients according to answers about the satisfaction by the quality of services of primary care settings.
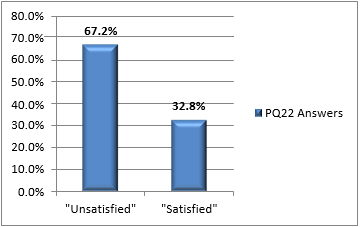
Figure 5: Distribution of surveyed patients about the quality of services of primary care settings after grouping the responses (“unsatisfied” and “satisfied”).
The percentage of patients (92.4%) who refer to the educational clips in the lobby and corridors of the family medical center is remarkably high. We obtained important results for the evaluation of Continuing Medical Education (CME) and Continuous Professional Development (CPD) during the survey of primary health care center managers. In particular, the percentage of primary health care centers where doctors received periodic training, workshops, and seminars was significantly high (76.5%; Chi2=14.24, df=2, p=0.001). The percentage of primary health care centers where doctors participated in such events once per year was 11.8%. However, it should be noted that participation in these events was not significantly financially supported by these settings. Specifically, 52.9% of managers noted that they did not provide financial support for doctors, while 47.1% confirmed financing of CME and CPD events (Chi2=0.06, df=1, p=0.808, NS) For Continuing Medical Education (CME) and Continuous Professional Development (CPD), it is crucial for doctors to participate in national or international thematic conferences and present reports. As a result of our survey, we found that managers who confirmed that doctors participate in national and international scientific conferences with their own funds amounted to 64.7% (Chi2=7.88, df=1, p=0.019). Regarding periodic medical information (printed or electronic), unfortunately, it was discovered that clinic managers either do not possess or are not aware of a unified database or library of medical journals and articles, which could assist family doctors in staying updated with the latest medical news (Chi2=3.47, df=3, p=0.325, NS).
However, all managers stated that the center is equipped with PCs, doctors possess computer skills, have access to web sources, and can obtain the necessary information.”
For the management of the COVID-19 pandemic, a state standard (protocol) for the management of the clinical condition against COVID-19 (SARS-COV-2) was developed for doctors of primary health care centers. During the study we were interested in how effectively the doctors fulfilled these standards and in what type of trainings and workshops they participated (Table 1). The difference between the responses was not significant.
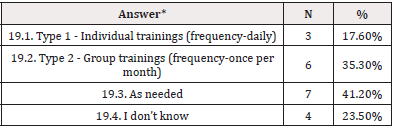
Table 1: Distribution of the managers according to the answers nQ19.
Note*: *Chi2 = 2.0, df=3, p=0.572 (NS).
Combining responses related to managers’ awareness (19.1 and 19.2, n=6) and lack of awareness (19.3 and 19.4, n=11), and Chi2-test treatment showed that the difference between these groups was also non-significant (Chi2=1.47, df=1, p=0.225, NS).
The answers to this question are relatively controversial in relation to the answers obtained to the question about the CPD of family doctors; 88.2% of managers answered that training, workshops, seminars are held for doctors from time to time.
Based on the answers we received from doctors about CME and CPD we evaluated the new variable -”level of CME-CPD”, which represents the sum of the answer scores.

Figure 6: The “level of CME-CPD” vs. Q18 - “Can you name the percentage of your beneficiaries were hospitalized with confirmed COVID-19 (SARS-CoV-2) bypassing a family doctor?”
The level of CME-CPD vs. Q18. The relationship between the level of Continuing Medical Education (CME) and Continuous Professional Development (CPD) and the responses to Question 18 (Q18) did not show a significant association with hospitalization for a confirmed COVID-19 (SARS-CoV-2) diagnosis bypassing a family doctor. It is worth noting the response option ‘I don’t know.’ A total of 57.4% of respondents had no information about hospitalization cases (Figure 6).
The “level of USG-UPG” vs. Q17. The distribution of CME-CPD levels and responses to the question Q17 are plausible but did not demonstrate a significant association with hospitalization for a confirmed diagnosis of COVID-19 (SARS-CoV-2) through a family doctor. It’s worth noting the indicator corresponding to the response ‘I don’t know.’ In fact, 38.6% of respondents lacked information about cases of hospitalization (Figure 7).”
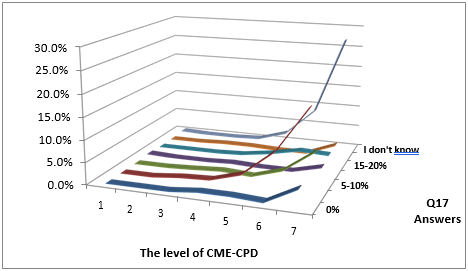
Figure 7: The “level of CME-CPD” vs. Q18 - “Can you name the percentage of your beneficiaries were hospitalized with confirmed COVID-19 (SARS-CoV-2) by a family doctor?”
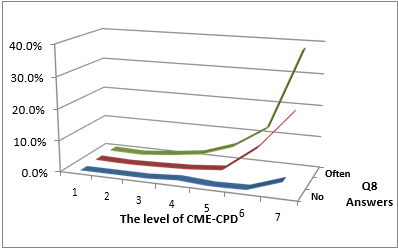
Figure 8: The “level of CME-CPD” vs. Q8 - “Do you carry out preventive consultations with your patients?”
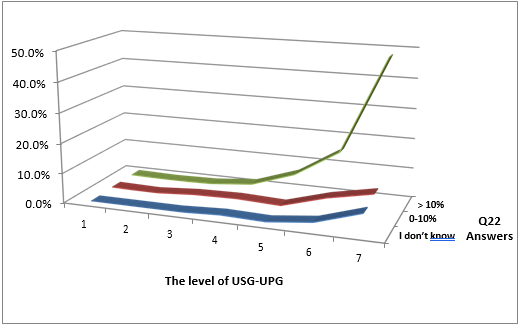
Figure 9: The level of USG-UPG vs. Q22 - “Can you name the percentage of your beneficiaries vaccinated against COVID-19 (SARS-CoV-2)?”
The distribution according to the” level of CME-CPD” and the answers to the Q18 question was not significant and did not show a significant association with the frequency of the preventive consultations with patients (Figure 8).
The “level of USG-UPG” vs. Q22. The relationship between the ‘level of USG-UPG’ and Question 22 (Q22) had a significant character, but it did not show a significant association with the possession of information about those vaccinated against COVID-19 (SARSCoV- 2, Figure 9).
Recommendations
Based on our original research, we created recommendations for primary care providers, family physicians and public health authorities.
Primary care providers should be actively involved in epidemic management and prevention, as they are often the first point of contact for patients and communities.
Primary care providers should also be aware of the local and national guidelines and protocols for epidemic management and prevention and adhere to them in their practice. They should coordinate with other health professionals and authorities to ensure timely and effective response to epidemic outbreaks.
Family Physicians should be able to identify, diagnose, treat, and refer suspected cases of epidemic diseases, as well as provide health education and counseling to their patients and families; Continuously update their knowledge and skills on epidemic management and prevention through CME and CPD activities.
Public health authorities should recognize and support the vital role of primary care providers in epidemic management and prevention. They should provide them with adequate resources, training, and incentives to participate in CME and CPD activities. They should also facilitate communication and collaboration among primary care providers and other stakeholders in the health system.
Conclusion
This article has underscored the significance of Continuous Medical Education (CME) and Continuous Professional Development (CPD) as the cornerstone of enhancing the family doctor’s competencies in addressing these crises.
As the frontline guardians of community health, family doctors hold a unique position in detecting and responding to infectious diseases, thereby safeguarding public health. The journey of lifelong learning, embodied by CME and CPD, is the key to ensuring that family doctors possess the knowledge, skills, and adaptability necessary to confront the unpredictable nature of epidemics.
In summary, family physicians are not only the first line of the defense in managing epidemics but also as the guardians of hope. Through continuous professional development, they can stand prepared to face the unknown with knowledge, resilience, and compassion.
References
- Starfield B, Shi L, Macinko J (2005) Contribution of primary care to health systems and The Milbank Quarterly 83(3): 457-502.
- M Mathews, L Meredith, Dana Ryan, Lindsay Hedden, Julia Lukewich, et al. (2023) The role of family physicians during a pandemic health care management Healthc Manage Forum 36(1): 30-35.
- Davis D, O'Brien MA, Freemantle N, Wolf FM, Mazmanian P Taylor Vaisey A (1999) Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA 282(9): 867-874.
- Harvey BJ The issue of public Can Fam Physician 55(11): 1057-1059.
- G Beria, V Surguladze, T Giorgadze (2020) Problematics and importance of continuing medical education in Health Policy, Economics & Sociology 2019: 5(2).
- M Mathews, D Ryan, Lindsay Hedden, Julia Lukewich, Marshall EG, et al. (2023) Strengthening the integration of primary care in pandemic response plans: a qualitative interview study of Canadian family physicians. Br J Gen Pract 73(730): e348- e355



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.