Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Evaluation of the Relationship between Type and Amount of Fat Consumption in the Diet and Functional Ovarian Cysts in Females of Reproductive Age
*Corresponding author: Mojdeh Abolmolouki, Department of Anesthesiology, Shahid Bahonar Hospital, Afzalipour Faculty of Medicine, Kerman University of Medical Sciences, Kerman, Iran.
Received: October 02, 2023; Published: October 12, 2023
DOI: 10.34297/AJBSR.2023.20.002698
Abstract
Purpose: To evaluate the relationship between the type and amount of dietary fat and functional ovarian cysts (FOC) in women of reproductive age.
Materials and methods: After conducting ultrasonography for FOC on several women, we enrolled 40 case and 40 control individuals. A common food frequency questionnaire (FFQ) was used. As the studied variables had abnormal distribution we used Mann-Whitney test for comparison of data. Odd’s ratio calculated for meaningful results using logistic regression.
Results: Most of the studied variables were not significantly different between two groups. Total fat (case median= 70.85; range= 37.28 to 508.82 and control median= 87.79; range= 15.58 to 320.79 grams) were meaningfully different (p= 0.03). The vitamin E, alpha-tocopherol, Mono-unsaturated fats, Poly-unsaturated fats, Linoleic acid, and Linolenic acid were more frequent in food resources of control group than case group (p< 0.05). But, Vitamin A, carotenoids, and Lutein were higher in food resources of the case group (p< 0.05). The food’s vitamin E (OR= 0.9164) and alpha-tocopherol (OR= 0.8966) seem to be protective against FOC whereas lutein (OR= 1.0002) may be a significant risk factor for it.
Conclusions: Therefore, certain lipids may be real risk factors of FOC. Anyhow, to obtain a clear view in this regards, controlled trials or cohort investigations should be performed with a more potent evaluating tool instead FFQ.
Short Condensation
Keywords: Functional ovarian cysts (FOC), Fat, Food frequency questionnaire (FFQ), Body mass index (BMI)
Introduction
Ovarian cysts are sacs, with or without fluid, located inside the ovary or on its surface [1]. A prevalent gynecological disorder among females of reproductive age is functional ovarian cysts (FOCs) [2]. The American Gynecological & Obstetrical Society reports that FOCs have a prevalence of 7%, and approximately 1 in 25 women become symptomatic [3]. The cause of ovarian cysts remains unknown, but environmental factors and lifestyle are thought to play a role in their development [4].
Ovarian cysts are categorized into functional and non-functional types. Follicular, corpus luteum, and luteinizing cysts are the functional types of ovarian cysts, while non-functional ovarian cysts include endometriosis cysts, polycystic ovaries, hemorrhagic ovarian cysts, dermoid cysts, adenoma cysts, sclerosing stromal tumors of the ovaries, ovarian mucinous adenoma cysts, and cysts originating from the borderline of paraovarian tumors [5]. FOCs are benign ovarian cyst masses that occur in women of reproductive age, and their size rarely exceeds 8cm [6]. When FOCs are hormonally active, they can cause pelvic pain, pain during sexual intercourse, irregular menstruation, pain during movement, the feeling of pressure on the rectum and bladder, abdominal distension, and urinary or digestive symptoms [7]. When FOCs are large, painful, and persistent, surgical intervention is necessary, and in some cases, ovariectomy may be required [8].
In a cross-sectional study, Chiaffarino and colleagues showed that approximately 4-7% of women who underwent ultrasonography had ovarian cysts with a diameter larger than 30mm [9]. While many functional ovarian cysts heal spontaneously, some require surgical intervention, leading to discomfort, increased risks of intervention, and higher treatment costs [10]. Considering that functional cysts are the most common types of ovarian cysts and that an increase in their size can lead to complications such as twisting, tearing, bleeding, pain, and psychological and physical impacts, it is necessary to study this group of cysts more than others [11].
According to current studies, dietary habits may be associated with the occurrence of ovarian cysts. Therefore, given the high prevalence of ovarian cysts and their consequences, this study aims to investigate the relationship between the type and amount of dietary fat consumption and FOCs in females of reproductive age who visited a sonography center in Kerman city, located in the central part of Iran, in 2019.
Materials and Methods
This case-control study included eighty women who visited an ultrasound center in Kerman city, located in the central part of Iran, during 2019. The inclusion criteria were women aged 15 to 49 years who had ultrasound findings available and provided consent to participate in the study. The exclusion criteria were a history of acute gynecological conditions, use of medications for hyperlipidemia, and history of ovarian cyst surgery. The participants were referred to the ultrasound center for various reasons, but all received an abdominal and pelvic ultrasound, solely pelvic, uterus, and ovaries sonography. After obtaining consent to participate in the study, the women underwent ultrasound with the probe placed on the abdomen in the anatomical location of the ovaries. The physician carefully monitored for the presence of any ovarian mass or cyst. The sonographer measured the size of the ovaries and any existing mass and recorded the dimensions of the cyst, a brief history of the patient, primary diagnosis, and the type of observed cyst. Patients who underwent vaginal ultrasound were also examined for ovarian cysts. Forty patients with functional ovarian cysts detected by ultrasound were included in the case group, and forty women in the same age group with normal ovarian cysts based on the pelvic ultrasound were included in the control group. Demographic data (age, employment status, education level) and anthropometric indicators (height, weight, and body mass index) were recorded.
Following ethical considerations, eligible individuals completed a previously validated and reliable food frequency questionnaire (FFQ) [12]. The amount of dietary fat was measured using a semi-quantitative FFQ.
Using a FFQ and related calculations, we determined the total sugar content (mainly glucose, galactose, fructose, sucrose, lactose, and maltose) and the elemental content (specifically phosphorus, magnesium, zinc, copper, manganese, selenium, fluoride, chromium, sodium, potassium, iron, and calcium) for each type of food resource. The contents of fat- and water-soluble vitamins, including vitamins A (and carotenoids), D, E (and alpha-tocopherol), K, vitamin C, and the vitamin B family (B1-B3, B5, B6, B7, B9, B12), were calculated for each case and control participant. The total fiber (soluble and insoluble), protein, lipid, and calorie contents of each person’s nutritional regimen were measured using the FFQ and related files. Additionally, we estimated the lipid ingredients that each person potentially receives from any type of food resource, including cholesterol, saturated fats, monounsaturated fatty acids, polyunsaturated fatty acids, oleic acid, linoleic acid, linolenic acid, eicosapentaenoic acid, docosahexaenoic acid, trans-fatty acids, lutein, caffeine, and lycopene. We also calculated the odds ratio for significant variables. This study was approved by the Ethics Committee of Kerman University of Medical Sciences (IR.KMU.AH.REC.1398.042).
Statistical Analysis
We conducted statistical analysis using SPSS software version 22 and MedCalc version 15.8. Quantitative variables were presented as mean ± standard deviation, and qualitative variables were presented as number (percentage). The normality of data was assessed using the Kolmogorov-Smirnov and Shapiro-Wilk tests. As the data did not follow a normal distribution, differences were compared using the Mann-Whitney U test. We used the chi-square test for qualitative variables and logistic regression to estimate the odds ratio (OR) for assessing the risk factors of functional ovarian cysts. We only performed estimations for significantly different variables when comparing case and control individuals, and we considered p-values less than 0.05 as statistically significant.
Results
The study participants had a mean age of 29.4±9.7 years, with the case and control groups having mean ages of 28.3±8.4 and 30.6±10.5 years, respectively (p=0.291). The case group had equal percentages of elementary education (40%), diploma (47.5%), and academic education (12.5%). Job status showed that 55% of the case group and 65% of the control group were stay-at-home spouses (Table 1).

Table 1: Comparison of demographic characteristics between the studied groups.
Note*: *Independent samples t-test.
Anthropometric indicators, such as height and weight, demonstrated no significant differences between the case and control groups. The height of the case (median=159; range=143 to 173cm) and control (median=159; range=148 to 185cm) groups were not significantly different (p=0.561). Additionally, the average weight of the case (median=64.75; range=47 to 90kg) and control (median=64; range=38 to 91kg) groups did not differ significantly (p=0.773). The body mass index (BMI) of the case group (median=24.84; range=19 to 37kg/m2) and control group (median= 25.31; range=15 to 39 kg/m2) were also not significantly different (p=0.59). Therefore, BMI did not serve as a distinguishing risk factor between the two groups. The frequency of individuals with BMIs within specified ranges did not vary significantly between the case and control groups (p=0.759). The case group had 10% with a lean status and a BMI less than 19.8 kg/m2, 42.5% with a BMI between 19.8-25 kg/m2, 10% with a BMI between 25-30 kg/ m2, and 37.5% with a BMI greater than 30 kg/m2. The control group had 5% with a lean status and a BMI less than 19.8 kg/m2, 37.5% with a BMI between 19.8-25 kg/m2, 12.5% with a BMI between 25- 30 kg/m2, and 45% with a BMI greater than 30 kg/m2.
Results showed that the median total fat consumption in the case group was 70.85g (range=37.28 to 508.82g), whereas it was 87.79g (range=15.58 to 320.79g) in the control group (p=0.03). However, there was no significant difference between the case (median= 22.34; range=8.19 to 188.15) and control (median=28.42; range=3.87 to 115.32) groups in terms of saturated fatty acid consumption (p=0.083). Mono-unsaturated fatty acids (MUFA) consumption in the case (median=22.49; range=12.93 to 187.7) and control (median=29.635; range=5.87 to 105.67) groups were not significantly different (p=0.95). Similarly, there was no difference in the intake of polyunsaturated fatty acids (PUFA) between the case (median=11.75; range=7.84 to 94.39) and control (median=18.225; range=4.58 to 54.29) groups (p=0.71).
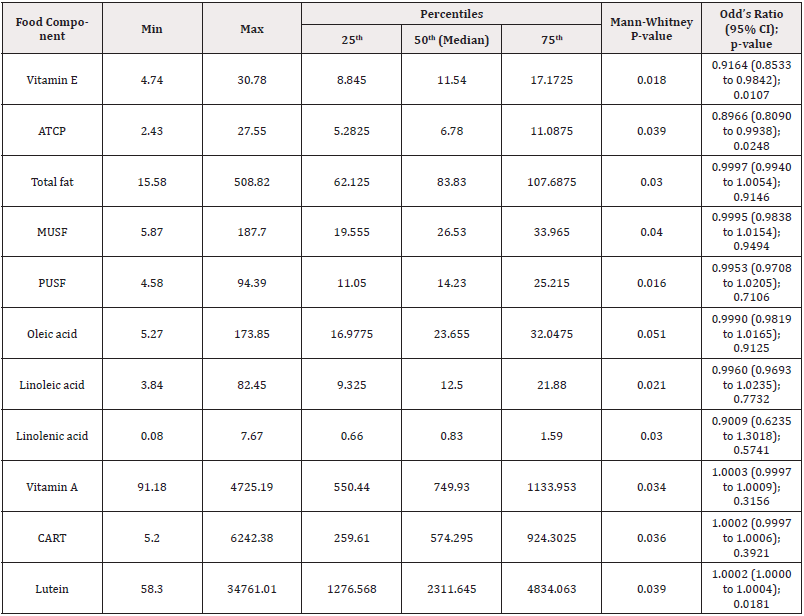
Table 2: Comparison of demographic characteristics between the studied groups.
Note*: ATCP: Alpha-tocopherol; CART: Carotenoids; MUSF: Mono-unsaturated fats; PUSF: Poly-unsaturated fats.
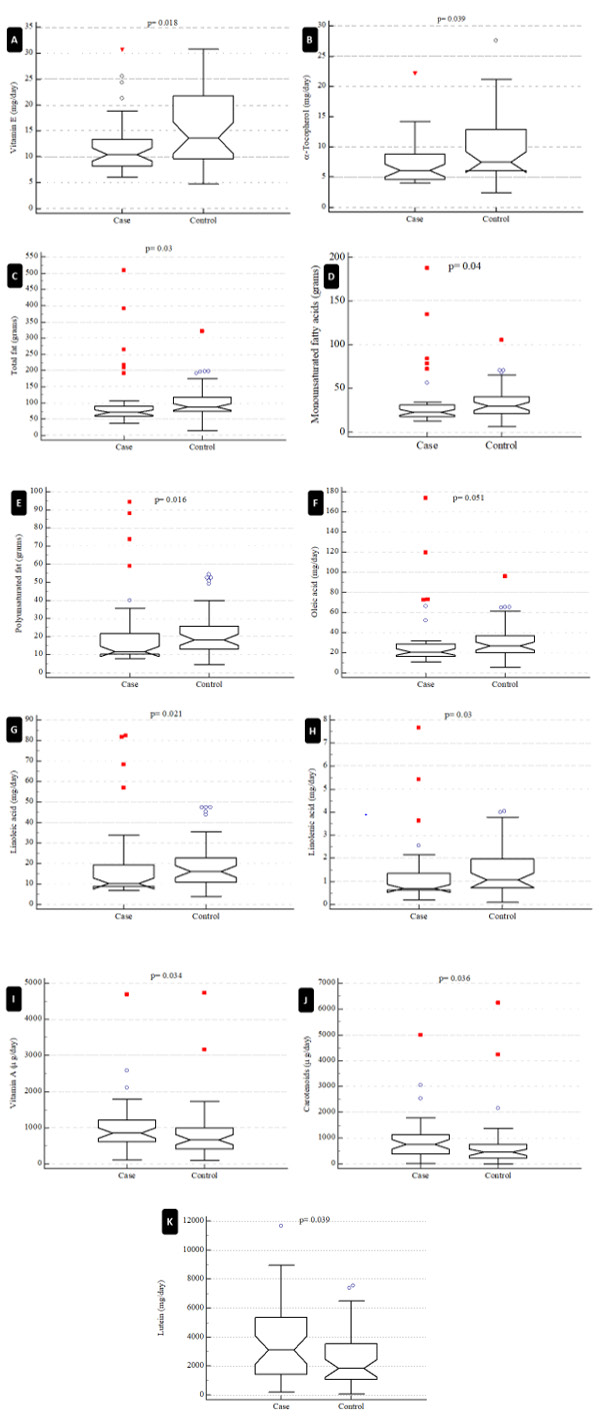
Figure 1: The study compared case (ovarian cyst) and control (without ovarian cyst) individuals and calculated p-values using the Mann-Whitney statistical test for various variables, including vitamin E (A), alpha-tocopherol (B), total fat (C), monounsaturated fats (D), polyunsaturated fats (E), oleic acid (F), linoleic acid (G), linolenic acid (H), vitamin A (I), carotenoids (J), and lutein (K). The p-value for oleic acid was near to significant (p=0.051), but all other variables showed significant differences between case and control groups.
Logistic regression analysis was used to estimate the odds ratios (OR) to determine the risk factors for FOC. The estimation was performed only for variables that differed significantly between the case and control groups (Table 2). Figure 1 shows a comparison of food contents that were significantly different between the case (ovarian cyst) and control (without ovarian cyst) groups. The control group’s food resources were expected to have higher amounts of vitamin E, alpha-tocopherol, total fat, MUFA, PUFA, linoleic acid, and linolenic acid than those in the food resources of the case group. Conversely, vitamin A, carotenoids, and lutein were found to be significantly higher in the case group’s food resources. Oleic acid content was nearly significantly higher in the control group compared to the case group. The other contents of food resources, including sugars, minerals, proteins, and lipids, did not differ significantly between the case and control groups (Figure 1, Table 2).
Using the OR estimation, it was found that only three food ingredients had meaningful ORs for FOC among the significantly different variables between the case and control groups (Table 2). Food’s vitamin E (OR=0.9164; 95% CI=0.8533 to 0.9842; p=0.0107) and alpha-tocopherol (OR=0.8966; 95% CI=0.8090 to 0.9938; p=0.0248) showed a protective effect against FOC, whereas food’s lutein (OR=1.0002; 95% CI=1.0000 to 1.0004; p=0.0181) was identified as a risk factor for FOC. The other variables in Table 2 did not appear to be risk factors for FOC.
Discussion
Although overweight and obesity are established risk factors for FOC, the BMI did not differ significantly between the case and control groups in our study. We aimed to investigate why this was the case, given the prevalence of obesity and other non-communicable diseases among women of reproductive age. The average BMI was 25.85 kg/m2 in the case group and 25.2 kg/m2 in the control group. However, as both groups exceeded the upper limit of normal BMI (24.9), we concluded that they were both at risk of FOC. Moreover, due to the high frequency of overweight and obesity among Iranian women of reproductive age, our study population may not have had a homogeneous distribution, rendering it unsuitable for evaluating the impact of BMI on FOC.
The aim of this study was to investigate the relationship between the type and quantity of food consumed by reproductive-aged females with (case) and without (control) FOC who visited an ultrasound center in Kerman city in 2019. Our results revealed significant differences in certain lipids and lipid-soluble vitamins in the routine nutritional regimen of the two groups.
The present study found no significant difference in BMI between the case and control groups, although obesity and overweight are established risk factors for FOC. FOCs are among the most common gynecological diseases worldwide, and their prevalence is influenced by lifestyle and nutritional factors, which are also risk factors for other non-communicable diseases [4,13,14]. Given the high prevalence of overweight and obesity among Iranian women of reproductive age [6], it is noteworthy that 20 (50%) case and 23 (57.7%) control participants in our study had a BMI above 24.5 kg/ m2. This suggests that our study population may not be suitable for evaluating the impact of BMI on FOC due to its uneven distribution.
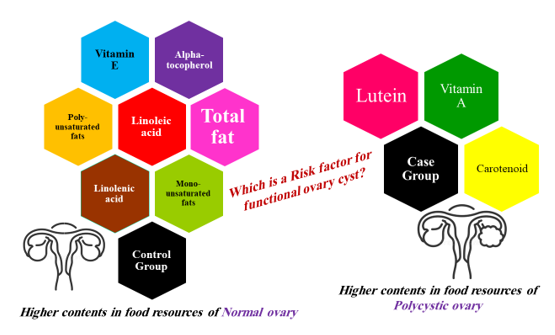
Nutrition and diet can influence the levels and types of sex hormones and binding proteins in the blood circulation, as well as the metabolism of prostaglandins and ovarian function [15]. Therefore, we conducted a detailed evaluation of the lipid types in the food resources consumed by the participants. Our results revealed that the food resources of the control group had significantly higher amounts of total fat, vitamin E, alpha-tocopherol, monounsaturated fats, polyunsaturated fats, linoleic acid, and linolenic acid compared to those of the case group. Conversely, the food resources of the case group had significantly higher amounts of vitamin A, carotenoids, and lutein. We concluded that food resources with higher carotenoid, vitamin A, and lutein contents may be involved in the mechanisms leading to cyst production, suggesting that cyst development may require higher intake of these nutrients through food resources. However, further evidence is required to reach a definitive conclusion, such as through controlled trials.
Certain studies have suggested an increased risk of ovarian cancer associated with higher fat intake, although the results are dependent on the type of fat consumed [2]. For instance, a study by Britton et al. on women aged 17 to 74 in the United States found that higher consumption of vegetable oils and polyunsaturated fats was associated with an increased likelihood of multiple endometriosis, serous, and teratoma occurrence [16]. Dietary fats can affect insulin, insulin-related growth hormones, and prostaglandin metabolism, which in turn can influence ovarian function [17]. However, other studies have reported different findings regarding the relationship between fat consumption and FOC. For example, Douglas et al. found no significant difference in mean fat consumption between women with and without FOC [18]. In our study, total fat, vitamin E, alpha-tocopherol, monounsaturated fats, polyunsaturated fats, linoleic acid, and linolenic acid were higher in the control group, with vitamin E and alpha-tocopherol having a protective effect against FOC. There is significant variation in the findings of studies on the relationship between fat consumption and FOC across different regions of the world.
We suggest that the use of FFQ as a tool to evaluate dietary components’ intake should be re-evaluated in each geographical area. Dietary habits are highly diverse worldwide, and the quality of nutritional components can vary substantially across different dietary regimens.
Alves and colleagues have suggested that exposure of estrogen receptors (ER) to high levels of free fatty acids can cause alterations and impairment of their activity [19]. According to Valckx et al., the absorption of dietary fatty acids in individuals may be associated with reproductive function by altering ovarian movement, follicular development, corpus luteum function, and uterine status [20]. In the study by Jahangirifar and colleagues, the consumption of total fatty acids, saturated fatty acids, polyunsaturated fatty acids, monounsaturated fatty acids, linoleic acids, and oleic acids was associated with a reduced fertilization rate [21]. However, our study found that the consumption of total fats, linoleic acid, linolenic acid, and vitamin E or tocopherol was lower in FOC patients than in normal women. It should be noted that although the control group consisted of non-FOC women at the time of the study, they may be at risk of developing FOC in the future.
Tafazoli, et al., [2] found that there was a non-significant difference in fat consumption between women with and without FOC [2]. However, in our study, the total fat consumption by the control group was significantly higher than that of women with FOC. We did not observe any association or difference between the protein content of the diet in the case and control groups, which contradicts some studies that suggest a link between meat consumption and ovarian cancer [22]. Note that meat contains saturated fat and could be a potential risk factor for FOC [23].
Several studies have demonstrated a strong relationship between increasing BMI and morbidity and mortality. Obesity affects insulin sensitivity and insulin resistance in patients with ovarian cysts [24]. Women with a higher BMI can produce more estrogen from steroids in adipose tissue, which has a positive effect on LH production and a negative effect on FSH production. Moreover, an increase in LH levels can cause hyperplasia of the ovarian stroma and an increase in androgen production, ultimately leading to the anovulation cycle in women [13]. Therefore, adopting a proper diet and engaging in appropriate physical activity to lose weight improves insulin levels, insulin resistance, and reduces androgenization, leading to improved ovulation. [11]. However, we suggest that all the evidence in this regard requires repeatable results to draw a clear direction for the prevention and management of FOC.
In our study, the average contents of vitamin A, carotenoids, and lutein in the foods consumed by the case group were significantly higher than those of the control group. Additionally, women without polycystic ovaries had a dietary regimen with significantly higher contents of vitamin E and alpha-tocopherol, total fats, monounsaturated fats, polyunsaturated fats, linoleic acid, and linolenic acid (Figure 2). Heterogeneous lifestyles and methods of food preparation may alter the pure effect of each nutritional resource on metabolism, hormonal, and physiological or pathological mechanisms. For example, in Iran, sheep meat is well-grained and mixed with potatoes and spices, and then grilled over charcoal flames, whereas in Europe, meat is prepared as steak. The use of different spices, flame sources, oils, and other additives can dramatically alter the contents of food ingredients. Nevertheless, investigating an outcome such as FOC, which is a disease with multiple risk factors, requires robust evidence to identify a precise cause.
Conclusion
The present study found that Iranian women with FOC had significantly higher levels of vitamin A, carotenoids, and lutein in their diets than those with healthy ovaries. Furthermore, higher levels of vitamin E and alpha-tocopherol in the diet appeared to be protective against FOC. BMI was a confounding factor in our study since at least 50% of the case or control individuals had a BMI above the normal range. Therefore, in selecting study groups, this confounding variable should be interpreted with caution. It is noteworthy that controlled trials or cohort investigations with larger sample sizes may provide better insight into the findings reported here. However, we believe that using a more robust tool than FFQ could yield better results, and this remains a significant challenge for future research in this field.
Data Availability
The data of this study are available under journal request or permission.
Acknowledgement
None.
Conflict of Interest
None.
References
- Grimes DA, Jones LB, Lopez LM, Kenneth F Schulz (2011) Oral contraceptives for functional ovarian cysts. Cochrane Database of Systematic Reviews 9: CD006134.
- Tafazoli M, Fazeli E, Dadgar S, Mohsen Nematy (2016) The association of the dietary fat and functional ovarian cysts in women of reproductive age referring to three hospitals in Mashhad, Iran, 2014. International journal of community-based nursing and midwifery. 4(2): 148-156.
- Rice LW, Lockwood CJ, Phipps M, John O L Delancey, Ronald D Alvarez, et al. (2019) The American Gynecological and Obstetrical Society—reinvigorating for the 21st century. American Journal of Obstetrics and Gynecology 220(4): 365. e1-365. e3.
- Mimoun C, Fritel X, Fauconnier A (2013) Épidémiologie des tumeurs ovariennes présumées bé Journal de gynécologie obstétrique et biologie de la reproduction 42(8): 722-729.
- Steinkampf MP, Hammond KR, Blackwell RE (1990) Hormonal treatment of functional ovarian cysts: a randomized, prospective study. Fertility and sterility 54(5): 775-777.
- Ahmadi R, Alinavaz M, Asgari V (2012) Biomedical Importance of Diet in Ovarian Cysts Occurrence in North-Western Iran. Journal of Medical and Bioengineering (JOMB): 1(1).
- Chen Y, Ahsan H, Parvez F, Geoffrey R Howe (2004) Validity of a food-frequency questionnaire for a large prospective cohort study in Bangladesh. British journal of nutrition 92(5): 851-859.
- Chiuve SE, Rexrode KM, Spiegelman D, Giancarlo Logroscino, JoAnn E Manson, et al. (2008) Primary prevention of stroke by healthy lifestyle. Circulation 118(9): 947-954.
- Chiaffarino F, Parazzini F, Surace M, Vito Chiantera, Carlo La Vecchia, et al. (2003) Diet and risk of seromucinous benign ovarian cysts. European journal of obstetrics & gynecology and reproductive biology 110(2): 196-200.
- Britton J, Westhoff C, Howe G, M D Gammon (2000) Lactose and benign ovarian tumours in a case–control study. British journal of cancer 83(11): 1552-1555.
- Butler W (2000) Nutritional interactions with reproductive performance in dairy cattle. Animal reproduction science 60: 449-457.
- Mohseni Takalloo S, Mirmiran P, Hosseini Esfahani F (2014) Dietary fat intake and its relationship with serum lipid profiles in tehranian adolescents. Journal of Food and Nutrition Research 2(6): 330-334.
- Mimoune N, Kaidi R, Azzouz MY, Safia Zenia, Mohamed Hocine Benaissa, et al. (2017) Investigation on diagnosis and metabolic profile of ovarian cysts in dairy cows. Kafkas Univ Vet Fak Derg 23(4): 579-586.
- Sasidharan JK, Patra MK, Singh LK, Abhishek C Saxena, Ujjwal K De, et al. Ovarian cysts in the bitch: An update. Top Companion Anim Med 43:100511.
- Palmisano BT, Zhu L, Eckel RH, John M Stafford (2018) Sex differences in lipid and lipoprotein metabolism. Mol Metab 15: 45-55.
- Britton JA, Westhoff C, Howe G, M D Gammon (2000) Diet and benign ovarian tumors (United States). Cancer Causes Control 11(5): 389-401.
- Yakar S, Nunez NP, Pennisi P, Pnina Brodt, Hui Sun, et al. (2006) Increased tumor growth in mice with diet-induced obesity: impact of ovarian hormones. Endocrinology 147(12): 5826-5834.
- Douglas CC, Norris LE, Oster RA, Betty E Darnell, Ricardo Azziz, et al. (2006) Difference in dietary intake between women with polycystic ovary syndrome and healthy controls. Fertil Steril 86(2): 411-417.
- Alves J, Bertolini M, Bertolini L, CMG Silva, D Rondina (2018) Lipotoxicity: impact on oocyte quality and reproductive efficiency in mammals. Animal Reproduction 12(2): 291-297.
- Valckx SD, Leroy JL (2015) The effect of maternal metabolic health and diet on the follicular fluid composition and potential consequences for oocyte and embryo quality. Handbook of Fertility: Elsevier: 35-44.
- Jahangirifar M, Taebi M, Nasr Esfahani MH, Motahar Heidari Beni, Gholam Hossein Asgari (2021) Dietary fatty acid intakes and the outcomes of assisted reproductive technique in infertile women. J Reprod Infertil 22(3):173-183.
- Bosetti C, Negri E, Franceschi S, C Pelucchi, R Talamini, et al. (2001) Diet and ovarian cancer risk: a case‐control study in Italy. Int J Cancer 93(6): 911-915.
- Parazzini F, Viganò P, Candiani M, Luigi Fedele (2013) Diet and endometriosis risk: a literature review. Reprod Biomed Online 26(4): 323-336.
- Akamine EH, Marçal AC, Camporez JP, Mara S Hoshida, Luciana C Caperuto, et al. (2010) Obesity induced by high-fat diet promotes insulin resistance in the ovary. J Endocrinol 206(1): 65-74.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.