Mini Review 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Mesenchymal Stem Cell Exosomes in the Treatment of Spinal Cord Injuries
*Corresponding author: Yuyu Sun, Nantong Third Hospital Affiliated to Nantong University, Nantong, 226001, China.
Received: December 09, 2023; Published: December 13, 2023
DOI: 10.34297/AJBSR.2023.20.002766
Abstract
Spinal cord injury (SCI) often leads to sensory or motor dysfunction in the affected area below the level of injury, and in severe cases, it can even be life-threatening. Unfortunately, due to the spinal cord’s limited ability to regenerate, there is currently no effective treatment strategy available for SCI patients. However, recent research has focused on the potential therapeutic benefits of mesenchymal stem cell exosomes (MSC-Exos). MSC-Exos as the main form of paracrine action by MSCs, enabling the transportation of bioactive molecules across cell barriers. This phenomenon allows MSC-Exos to modulate crucial physiological functions such as immunosuppression, tissue repair, and angiogenesis. In this paper, we aim to review the immune microenvironment of SCI, explore the characteristics of MSC-Exos, and discuss their potential applications in the treatment of SCI. Lastly, we address the limitations and shortcomings of MSC-Exos in the context of SCI therapy.
Keywords: Mesenchymal stem cells, Exosomes, Spinal cord injury, Therapy
Introduction
Neuronal death, axonal and myelin necrosis occurs after SCI, leading to an extensive inflammatory response, which further exacerbates the secondary injury [1]. MSC improves motor function and increases neuronal survival after SCI [2], and its exosomes promote tissue damage repair, vascular regeneration, reduce inflammatory cell infiltration, attenuate myelin deletion and axon degeneration, and increase the number of neurons surviving [3], thus reducing the degree of damage to the spinal cord tissue and improving motor and sensory functions after SCI, and the combined application of its biomaterials, such as hydrogel, resulted in the longer duration of the action of MSC-Exos, and a more significant therapeutic effect. The MSC-Exos described herein is considered to be the best non-cellular treatment currently available to improve the local microenvironment after SCI and to promote neuronal and axonal regeneration after injury as well as functional recovery after injury.
MSC-Exos
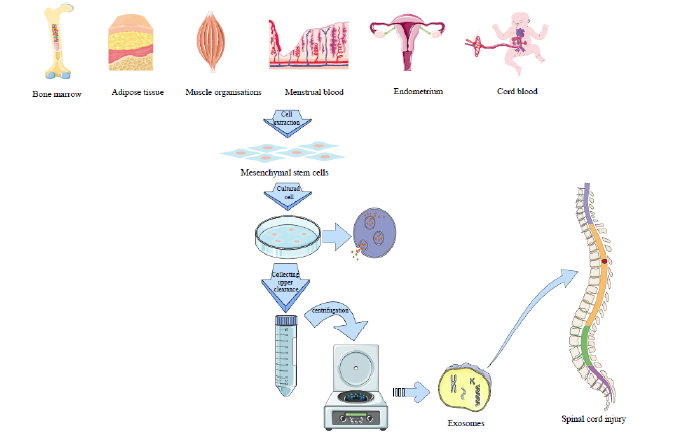
MSC-Exos serve as the primary vehicles for exerting MSC paracrine secretion. These exosomes carry abundant genetic information from MSCs and, due to their small size and high mobility, establish a stable bio signalling pathway for transmitting biomolecules throughout the entire organism [4]. Additionally, MSC-Exos have the capability to modulate various biological processes, such as apoptosis, fibrosis, angiogenesis, inflammatory response, cell regeneration, and immunity (Figure 1).
Application of MSC-Exos in SCI Treatment
Currently, there is a growing research interest in inhibiting the acute inflammatory response of SCI, improving cellular edema, promoting local blood vessel regeneration, inhibiting demyelination of spinal cord tissues, and promoting axon regeneration as hot spots focused in SCI treatment research.
MSC-Exos have been shown to significantly reduce the risk of the body’s immune response and target the site of injury. They also alleviate the local inflammatory response, attenuate myelin de-sheathing and axonal degeneration, and reduce the expression levels of inflammatory factors. MSC-Exos promote macrophage polarization from the M1 phenotype to the M2 phenotype [5], decrease the number of A1-type astrocytes, and modulate the local immune microenvironment [6]. Furthermore, they increase the number of residual neurons, neuronal synaptic branches, and promote axon regeneration in both the central and peripheral nervous systems after neurological injuries [7]. Lastly, MSC-Exos have been found to improve limb motor function [8].
The exosomes extracted by low oxygen pretreatment of MSCs are more numerous and more readily taken up by target cells in the injured area. Its treatment of SCI resulted in a smaller area of spinal cord lesions, a greater number of neurons surviving, and more pronounced functional recovery. Exosomes obtained through low oxygen pretreatment of MSCs are abundant and are easily internalized by target cells in the injured region [9]. Treatment with these exosomes led to reduced spinal cord lesion size, increased neuronal survival, and enhanced functional recovery in SCI.
Exosomes Combined with Biomaterials for the Treatment of SCI
To address the issue of exosomes’ unstable duration of action in organisms, researchers combine them with biomaterials, which serve as carriers and facilitate their functions. Natural biomaterials can be composed of proteins found in the extracellular matrix (ECM). ECM-based biomaterials typically undergo faster in vivo degradation and have lower mechanical strength. Synthetic biomaterials are typically more adjustable compared to natural biomaterials [10,11]. Currently, the primary biomaterials used in spinal cord injury (SCI) treatment are biodegradable hydrogels. These hydrogels fill the lesion cavity after in situ injection of SCI [12] and provide a sustained release of exosomes to the local area of SCI, resulting in a longer duration of action and a more significant therapeutic effect than ordinary exosomes [13].
Conclusion
MSC exosomes offer significant advantages in the treatment of SCI, as an effective drug carrier, they can bypass the cerebral spinal cord barrier. Exosomes secreted from MSCs pre-treated with hypoxia can additionally enhance the therapeutic effect. By combining biomaterials with exosomes, the biological half-life of exosomes can be prolonged, ensuring a more stable therapeutic effect.
Despite the significant potential of exosomes in SCI treatment, numerous challenges persist in applying exosome therapy in clinical settings. These challenges include identifying the appropriate source of exosomes, establishing standardized preparation procedures, and determining the optimal mode of administration, frequency of injection, and dosage. The majority of current research on exosomes for SCI involves animal experiments, predominantly using rodents. However, the relatively small size and robust survivability of rodent spinal cord tissue present differences compared to the larger human spinal cord tissue, which also exhibits anatomical disparities and distinct immune response mechanisms. Hence, it is crucial to conduct studies using non-human primates. While the therapeutic efficacy of exosomes in SCI is undeniable, the investigation of post-treatment complications associated with exosomes remains deficient, and the precise repair mechanism by which exosomes alleviate damage has not been thoroughly elucidated. Consequently, caution is warranted in applying exosomes to clinical settings at this stage.
Acknowledgment
This work was supported by Nantong Science and Technology Project (MS22022012, MS12021039); Nantong Municipal Commission of Health and Family Planning (MS2022062) and Large Instruments Open Foundation of Nantong University (KFJN2301).
Conflicts of Interest
None.
References
- Fan L, Liu C, Chen X, Zheng L, Zou Y, et al. (2022) Exosomes-Loaded Electroconductive Hydrogel Synergistically Promotes Tissue Repair after Spinal Cord Injury via Immunoregulation and Enhancement of Myelinated Axon Growth. Adv Sci 9(13): e2105586.
- Wu Q, Wang Q,, Li Z, Li X, Zang J, et al. (2018) Human menstrual blood-derived stem cells promote functional recovery in a rat spinal cord hemisection model. Cell Death & Disease 9(9): 882.
- Liu W, Wang Y, Gong F, Rong Y, Luo Y, et al. (2019) Exosomes Derived from Bone Mesenchymal Stem Cells Repair Traumatic Spinal Cord Injury by Suppressing the Activation of A1 Neurotoxic Reactive Astrocytes, J Neurotrauma 36(3): 469-484.
- Chen L, Qu J, Xiang C (2019) The multi-functional roles of menstrual blood-derived stem cells in regenerative medicine, Stem Cell Res Ther 10(1): 1-10.
- Sun G, Li G, Li D, Huang W, Zhang R, et al. (2018) hucMSC derived exosomes promote functional recovery in spinal cord injury mice via attenuating inflammation. Mater Sci Eng C Mater Biol Appl 89: 194-204.
- Fan B, Wei Z, Feng S (2022) Progression in translational research on spinal cord injury based on microenvironment imbalance. Bone Res 10(1): 35.
- Lopez-Verrilli MA, Caviedes A, Cabrera A, Sandoval S, Wyneken U, et al. (2016) Mesenchymal stem cell-derived exosomes from different sources selectively promote neuritic outgrowth. Neuroscience 320: 129-139.
- Khan NZ, Cao T, He J, Ritzel RM, Li Y, et al. (2021) Spinal cord injury alters microRNA and CD81+ exosome levels in plasma extracellular nanoparticles with neuroinflammatory potential. Brain Behav Immun 92: 165-183.
- Liu W, Rong Y, Wang J, Zhou Z, Ge X, et al. (2020) Exosome-shuttled miR-216a-5p from hypoxic preconditioned mesenchymal stem cells repair traumatic spinal cord injury by shifting microglial M1/M2 polarization. J Neuroinflammation 17(1): 47.
- Shahriari D, Koffler JY, Tuszynski MH, Campana WM, Sakamoto JS (2017) Hierarchically Ordered Porous and High-Volume Polycaprolactone Microchannel Scaffolds Enhanced Axon Growth in Transected Spinal Cords. Tissue Eng Part A 23(9-10): 415-425.
- Kaplan B, Merdler U, Szklanny AA, Redenski I, Guo S, et al. (2020) Rapid prototyping fabrication of soft and oriented polyester scaffolds for axonal guidance. Biomaterials 251(2020): 120062.
- Vismara I, Papa S, Rossi F, Forloni G, Veglianese P (2017) Current Options for Cell Therapy in Spinal Cord Injury. Trends Mol Med 23(9): 831-849.
- Li L, Zhang Y, Mu J, Chen J, Zhang C, et al. (2020) Transplantation of Human Mesenchymal Stem-Cell-Derived Exosomes Immobilized in an Adhesive Hydrogel for Effective Treatment of Spinal Cord Injury. Nano Lett 20(6): 4298-4305.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.