Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Primary Ovarian Carcinosarcoma: Case Report and Literature Review
*Corresponding author: Imane Ouafki, Medical Oncology Department, Hassan II University Hospital, Sidi Mohamed Ben Abdellah University, Fez, Morocco.
Received: November 23, 2023; Published: November 28, 2023
DOI: 10.34297/AJBSR.2023.20.002747
Abstract
Primary ovarian carcinosarcoma (OCS) is an extremely rare malignancy constituting less than 2% of ovarian cancers. Formerly known as malignant mixed müllerian tumor, this neoplasia characterized histologically by a double carcinomatous and sarcomatous component, is also classified as homologous or heterologous. Due to the low incidence of the tumor, its management is based on retrospective studies, that’s why patients are usually treated the same as women diagnosed with other subtypes of epithelial ovarian cancer. Treatment consists of optimal cytoreductive surgery combined with platinum-based chemotherapy regimens which has achieved the same survival rates observed in epithelial ovarian cancer. Given the poor prognosis of OCS, median survival does not exceed 18 months. The prognostic significance of the FIGO stage has been previously demonstrated insofar as optimal cytoreductive surgery is associated with improved survival. This study aims to present a case of OCS and focuses on its clinicopathological characteristics. We also assessed therapeutic management and outcomes in these patients, as well as prognostic factors related to survival.
Keywords: Carcinosarcoma, Ovary, Primary, Chemotherapy
Introduction
Ovarian carcinosarcoma (OCS) is an extremely rare malignant tumor representing approximately 1-2% or less of all ovarian cancers [1].This neoplasm previously named as a malignant mixed Mullerian tumor, is derived from the Müller and the Wolff ducts and is composed of a mixture of epithelial, glandular, and mesenchymal elements homologous to the connective tissue supporting the organ in which the tumor is growing, or on the contrary heterologous. Carcinosarcoma is found also in other organs of the genitourinary tract, including uterus, fallopian tubes, breast, and urethra [2]. It is a tumor of postmenopausal women with a poor prognosis since most patients are diagnosed at an advanced stage of the disease. Due to the rarity of carcinosarcoma, its treatment is based mainly on the results of small series of cases and on the management of other histological subtypes of epithelial ovarian cancer. Therefore, optimal surgery is the cornerstone of treatment. Chemotherapy is largely modeled on the recommendations established for epithelial ovarian cancer [3]. Through this clinical case, we report the story of a patient treated for primary ovarian carcinosarcoma by cytoreduction surgery followed by chemotherapy, then optimal complement to the surgical procedure. The clinical and pathological characteristics, as well as the therapeutic modalities and prognostic factors will be discussed.
Patient and Observation
Our patient is a 41-year-old married woman, nulliparous, without notable pathological history. The onset of symptoms goes back six months by pelvic pain aggravated by abdominal distension associated with a hemorrhagic syndrome for which she was transfused with a transfusion accident. A chest x-ray performed had objectified pleurisy, with a normal pleural biopsy. Clinical examination found a hard abdominal mass protruding beyond the umbilicus with a mass bulging in vaginal examination in the Douglas pouch. Pelvic ultrasound showed a normal-sized uterus, a homogeneous endometrium and the presence of a heterogeneous vascularized image, very flexible, probably of ovarian origin. Abdominopelvic magnetic resonance imaging revealed a bilateral ovarian tumor measuring 19cmx17cm for the largest, thrombosis of the proximal part of the inferior vena cava extending to the left external iliac vein and ascites of moderate abundance. During her hospitalization, the patient presented with dyspnea, a computed tomography (CT)angiography was performed confirming a proximal pulmonary embolism, extended to the lobar and segmental bronchi, a voluminous, multiloculated solidocystic formation, poorly limited, occupying the entire pelvis and abdomen, measuring 27x16x28cm in diameter, thrombosis of the left external iliac vein, extending to the ipsilateral common iliac vein, low abundance ascites, with infiltration of the mesenteric fat and thickening of the peritoneal layers more marked in the perilesion (Figure 1).

Figure 1: Thoraco-abdominal-pelvic scan showing a voluminous, multiloculated solido-cystic formation, poorly limited, occupying the entire pelvis and abdomen,measuring 27x16x28cm in diameter,thrombosis of the left external iliac vein, extending to the ipsilateral common iliac vein,low abundance ascites, with infiltration of the mesenteric fat and thickening of the peritoneal layers more marked in the peri-lesion.

Figure 2(a-b): HES histological description: Tumor proliferation arranged in diffuse layers. Tumor cells are medium in size, with a vesicular nucleus and abundant eosinophilic cytoplasm. Several figures of mitosis. The tumor stroma is loose fibrous.
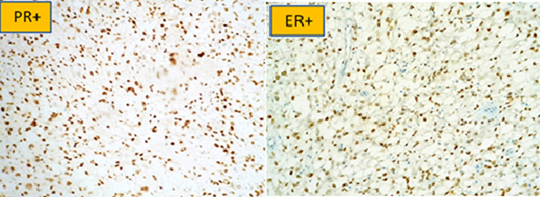
Figure 3: Positivity of progesterone (PR) and estrogenic (ER) hormone receptors in immunohistochemistry.
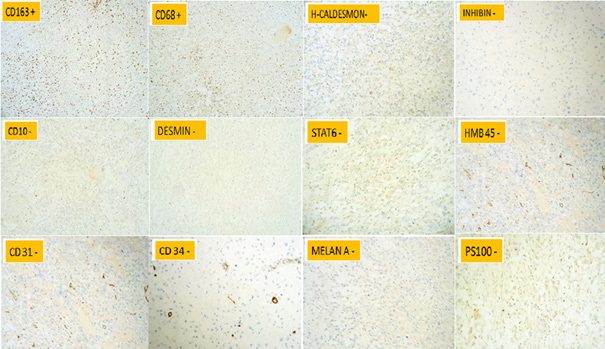
Figure 4b: Other immunohistochemical markers that have contributed to the diagnosis of carcinosarcoma.
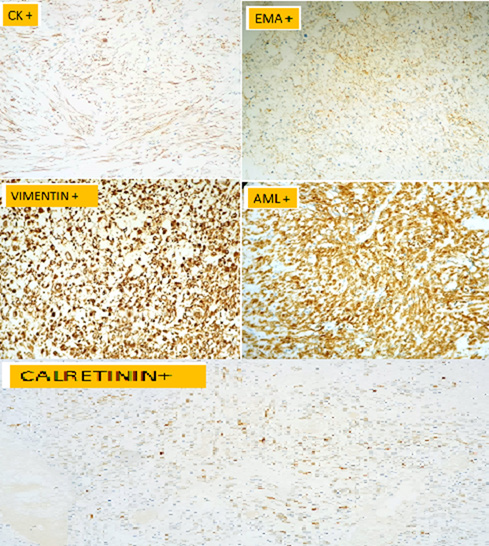
The CA125 was dosed at 320IU/ml. The laparotomy had revealed an ascites of great abundance, aspirated at 4 liters, a sample for cytological examination was taken, on exploration we found an enormous friable mass at the expense of the left ovary adhering to the wall, omentum and uterus, measuring 30cm long axis, adhesiolysis done with fragmentation of the mass. The liver and stomach are smooth without peritoneal carcinoma nodules.-A left annexectomy was performed removing the mass which was fragmented due to the friability. The right appendix was not seen, hidden by adhesions. Omentectomy as well as multiple biopsies were done. The hysterectomy could not be performed due to the adhesions. Pathological examination of the ovarian mass and omentectomy with immunohistochemical study were carried out. The expression of both epithelial markers (Cytokeratin [CK]/ EMA) and mesenchymal markers (Vimentin / AML / Calretinin) allowed us to make the diagnosis of carcinosarcoma (Figures: 2(a,b),3,4(a,b)).
The cytology of the ascitic fluid was inflammatory. The postoperative CA 125 had normalized to 15.90IU/ml. After a normal pre-chemotherapy biological assessment, and the start of an anticoagulation based on low molecular weight heparin, we started a first chemotherapy by the combination of gemcitabine and carboplatin. The tolerance of chemotherapy was marked by three episodes of neutropenia, requiring the addition of granulocyte growth factors. The patient had received a total of six cures and then re-evaluated by a thoraco-abdomino-pelvic CT which showed no signs of recurrence or pulmonary embolism, with a normal CA 125. The surgery was completed by a total hysterectomy with a left annexectomy, pelvic and lumboaortic lymph node dissection, without lymph node involvement. The postoperative CT scan was without abnormalities. The patient remained in good control for eight months, then she presented a local recurrence by two masses of peritoneal carcinoma measuring 78x32mm and 29x15mm associated with a moderate abundance of ascites. The CA 125 went from 4 to 65.86IU/ml. Since the patient’s performance status was still preserved, second-line chemotherapy was started with the discussion of a surgical procedure in the event of a good response to the chemotherapy.
Discussion
Primary OCS is a malignant neoplasm that is both exceptional and aggressive because most patients are diagnosed between the ages of 50 and 70, and 75% are in stage 3 or 4 [4]. Our patient is younger, 41 years old. Carcinogenesis is still controversial with three theories in question: collision, combination and conversion. The collision assumes a biclonal origin following the fusion of two stem cells. Whereas the combination suggests a monoclonal origin but with a cell strain alternately generating epithelial and sarcomatous cell. Finally, the conversion which also pleads for the monoclonal origin but with a carcinomatous stem cell secondarily dedifferentiating into a sarcomatous cell [5]. Currently, immunohistochemical and molecular studies allow carcinosarcoma to be considered as a metaplastic carcinoma with a monoclonal origin (conversion theory). The clinical manifestations are similar to those of epithelial ovarian carcinoma, without particular specificity [6]. It may present with abdominal pain, abdominal distension or pelvic mass most often and sometimes with urinary frequency [7]. The staging applied is that of ovarian carcinomas according to the International Federation of Gynecology and Obstetrics (FIGO) 2014 classifications. Clinical and radiological evaluation frequently underestimate the extent of the disease. The low incidence of OCS explains why there is little data to establish a consensus on its management. The recommendations are based on small retrospective studies. Reason why patients are usually treated the same as women diagnosed with other subtypes of epithelial ovarian cancer [3].
The aim of surgery is to achieve complete staging in early-stage patients and optimal cytoreduction in advanced stage patients. Ovary-type surgery is recommended, including total hysterectomy with bilateral annexectomy, omentectomy, pelvic and lumboaortic lymph node dissection and peritoneal resection with a view to complete resection [3]. The majority of the retrospective series available endorse the role of optimal cytoreduction in OCS surgery in improving survival. A strong correlation has been shown between the size of the tumor residue and the benefit in progression-free survival (PFS) and overall survival (OS) [3]. Histologically, the carcinomatous component often combines a high-grade serous component, grade 3 endometrioid, clear-celled or undifferentiated. Depending on the sarcomatous component, two types are defined: either the sarcomatous component is normally present within the organ, we will then speak of homologous carcinosarcoma, or the component is formed of elements usually absent (cartilage tissue, bone, muscle fibers striated) we will then speak of heterologous carcinosarcoma (the most frequent form) [1]. Regarding chemotherapy, several retrospective studies have validated the use of platinum-based chemotherapy, either carboplatin-paclitaxel or ifosfamide-cisplatin [6]. Platinum-based chemotherapy is the standard systemic adjuvant therapy [3]. A randomized phase III NRG Oncology clinical trial GOG 0261 of paclitaxel plus carboplatin versus paclitaxel plus ifosfamide in chemotherapy-naive patients with stage I-IV, persistent or recurrent carcinosarcoma of the uterus or ovary, concluded that the combination of paclitaxel and carboplatin was not inferior to paclitaxel and ifosfamide in terms of OS. In addition, paclitaxel plus carboplatin had better PFS compared to paclitaxel plus ifosfamide [8]. The difference in survival between the cisplatin and ifosfamide group and the carboplatin and paclitaxel group was not statistically significant. First-line cisplatin and ifosfamide or carboplatin and paclitaxel can achieve survival rates observed in epithelial ovarian cancer [9]. Moreover, patients in poor performance status who cannot withstand double chemotherapy with platinum salts appear to benefit from monochemotherapy, ifosfamide or, possibly, platinumfree combinations such as ifosfamide plus paclitaxel [6].
If the initial surgery is incomplete, platinum-based chemotherapy, either carboplatin-paclitaxel or ifosfamidecisplatin is indicated for at least 6 cycles with rediscussion of the debulking after 3 to 4 cycles [9]. A multicenter study showed that disease free survival (DFS) and OS rates of patients with OCS and ovarian high-grade serous carcinoma seem to be similar whenever optimal cytoreduction is achieved and followed by platinum plus taxane combination chemotherapy [10]. Targeting pathways such as vascular endothelial growth factor (VEGF) may be beneficial in OCS [10]. In addition, anti-VEGFs were accompanied by a clinical benefit in large prospective randomized trials (GOG- 0218 and ICON-7) epithelial ovarian cancer (OC), but not for OCS. The role of intraperitoneal chemotherapy with cisplatin and hyperthermia (HIPEC) is under investigation. HIPEC is a valid treatment option for ovarian cancer, but there are no studies specifically for carcinosarcoma. The combination of intravenous and intraperitoneal chemotherapy is also feasible [10]. OCS is a pathology with a poor prognosis with an estimated 5-year survival rate of 28.2% compared to 38.4% for serous ovarian cancer, regardless of the stage of the disease .Median survival is reported to be less than 18 months [1]. In order to improve this survival, it is necessary to identify the prognostic factors involved. The most significant predictor of survival is the stage at diagnosis. Among the prognostic factors reported in the literature, we distinguish the FIGO stage, age and menopausal status. Optimal cytoreductive surgery has also been shown to prolong survival in these patients. In addition, the type of sarcomatous elements (heterologous versus homologous) is a prognostic factor which has also been validated [7].
Conclusion
OCS is a rare aggressive tumor associated with poor prognosis. Its management is modeled on that of epithelial OC. Optimal surgery remains the cornerstone of treatment for the early stages. Cisplatin based chemotherapy remains the standard adjuvant treatment to surgery. But, also in case of locally advanced or metastatic disease. Hope is in development of targeted therapies with a view to improving the prognosis of this disease. More, clinical trials must be devoted to this pathology in order to establish adequate therapeutic strategies.
Competing Interests
The authors declare that they have no competing interests.
Authors’ Contributions
Imane Ouafki is the principal author of this work. Imane Ouafki did the initial writing of the article, assessed the figures, integrated all the corrections and contributed to the improvement of the form and the content of the text. All authors have globally enriched this clinical case, read and approved the final version of the manuscript for publication.
References
- MA Harris, LM Delap, PS Sengupta, PM Wilkinson, RS Welch, et al. (2003) Carcinosarcoma of the ovary. British Journal of Cancer BJC 88(5): 654 -657.
- Marcela G del Carmen, Michael Birrer, John O Schorge (2012) Carcinosarcoma of the ovary: a review of the literature. Gynecol Oncol 125(1): 271-277.
- J Alejandro Rauh Hain, Michael Birrer, Marcela G Del Carmen (2016) Carcinosarcoma of the Ovary, Fallopian Tube, and Peritoneum: Prognostic Factors and Treatment Modalities. Gynecol Oncol 142(2): 248-254.
- Cantrell LA, Van Le L (2009) Carcinosarcoma of the ovary a review. Obstet Gynecol Surv 64(10): 673-680.
- I Gorai, T Yanagibashi, A Taki, K Udagawa, E Miyagi, et al. (1997) Uterine carcinosarcoma is derived from a single stem cell: an in vitro study. Int J Cancer 72(5): 821-827.
- M S Mano, DD Rosa, E Azambuja, G Ismael, S Braga, et al. (2007) Current Management of Ovarian Carcinosarcoma. Int J Gynecol Cancer 17(2): 316-324.
- Hyun Jin Kim, Hyun Mi Lee, Mi Kyung Kim, Yoo Kyung Lee, In Ho Lee, et al. (2017) Prognostic assessment of sarcomatous histologic subtypes of ovarian carcinosarcoma. Obstet Gynecol Sci 60(4): 350-356.
- Matthew A. Powell, Virginia L. Filiaci, Martee Leigh Hensley, et al. (2019) A randomized phase 3 trial of paclitaxel (P) plus carboplatin (C) versus paclitaxel plus ifosfamide (I) in chemotherapy-naive patients with stage I-IV, persistent or recurrent carcinosarcoma of the uterus or ovary: An NRG Oncology trial JCO 37(15_suppl).
- DA Silasi, J L Illuzzi, M G Kelly, T J Rutherford, G Mor, et al. (2008) Carcinosarcoma of the ovary. Int J Gynecol Cancer 18(1): 22-29.
- Makris GM, Siristatidis C, Battista MJ, Chrelias C (2015) Ovarian carcinosarcoma: a case report, diagnosis, treatment and literature review. Hippokratia 19(3): 256-259.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.