Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Prognostic Factors Influencing the Survival of Patients with Brain Metastases from Lung Cancer
*Corresponding author: Imane Ouafki, Medical Oncology Department, Hassan II University Hospital, Fez, Morocco.
Received: November 20, 2023; Published: November 28, 2023
DOI: 10.34297/AJBSR.2023.20.002745
Abstract
Introduction: The occurrence of brain metastases (BM) in patients with primary lung cancer, present at diagnosis or appearing later, is a frequent situation and constitutes a clinical entity known to have a poor prognosis: in 30 to 50% of non-small- cell lung cancers(NSCLC) , mostly adenocarcinomas.They impact overall survival and quality of life. Management is specific depending on the histology, the number of BM, whether or not they are symptomatic, life expectancy and clinical stage (oligometastatic or multimetastatic).
Materials and Methods: This is a monocentric, retrospective observational study,including patients with NSCLC in the medical oncology department , at the Hassan II university hospital in Fez.Between January 2009 and January 2019, we evaluated the prognostic factors influencing the survival of patients with BM from NSCLC.Among the 489 NSCLC cases collected, 80 patients met the inclusion criteria.
Conclusion: At the end of this study, the age, the performance status (PS) less than 2, encephalic radiotherapy, absence of extracranial metastases and female sex were associated with better survival. However, this association was statistically insignificant.
Keywords: Factors, Prognosis, Cancer, Lung, Brain, Metastases, Survival
Introduction
Lung cancer is the most common male cancer and represents the leading global cause of cancer mortality. It’s a big provider of brain metastases (BM). In fact, it is the origin of 40–50% of all BM [1]. The increase in survival and improvement in quality of life, due to progress in systemic and local treatment, increases its incidence [2]. Smoking is the main causal factor. The management of lung cancer with BM is specific, very heterogeneous and depends on several elements. The primary objective of this work is to analyze the prognostic factors associated with better survival in this very heterogeneous patient population. The secondary objectives aim to determine the frequency of BM in NSCLC; describe its clinical and anatomo-pathological aspects; evaluate the therapeutic means and finally assess the results of the treatments received.
Materials and Methods
Our study is observational, retrospective, monocentric. This work is based on analysis of patient files followed for NSCLC in the medical oncology department, of the Hassan II University Hospital in Fez. The non-opposition of patients to the use of their data was verified before analysis by signing consent enlightened. Between January 2009 and January 2019, we evaluated the prognostic factors influencing the survival of patients with BM of NSCLC. Among the 489 cases of NSCLC collected, 80 patients with BM were included. Inclusion criteria were: age over 18 years; a primary non-small cell lung cancer and the presence of BM. The exclusion criterion was non-consent of the patient. Eligible patients were searched from: the database of the information system, by selecting patients treated for cerebral localization; the hospital register of the medical oncology department at CHU Hassan II in Fez; medical files from the medical oncology department at CHU Hassan II in Fez. The data are entered using Excel software, then analyzed by SPSS version 20 software. The significance level was set at p<0.05 for all statistics tests. The description of the population focused on the distribution of age and sex, calculation of means, frequencies and 95% confidence intervals (95% CI). A univariate analysis is carried out to evaluate the prognostic value of PS, age, sex, presence of extra cranial metastases and the therapeutic modalities of these latest. The follow-up median is calculated from the date of the last news (i.e., the last consultation for living patients, i.e. the date of death for dead patients) in relation to the date of diagnosis. Progression-free survival (PFS) is calculated from the date of start of treatment to the date of progression or death. Overall survival (OS) is estimated from the date of diagnosis to the date of death (date of last news).
Results
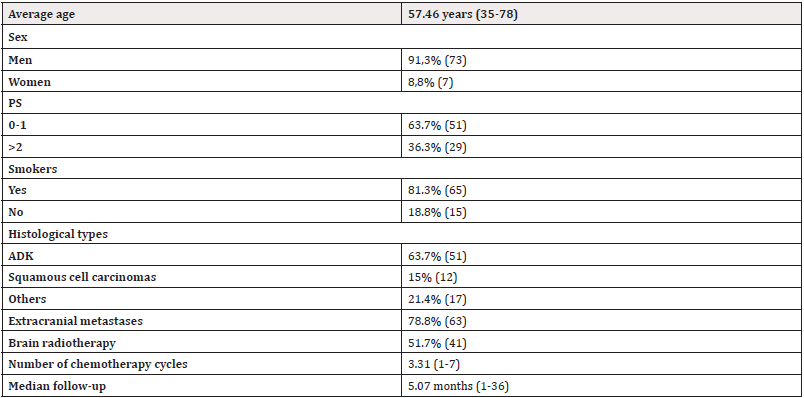
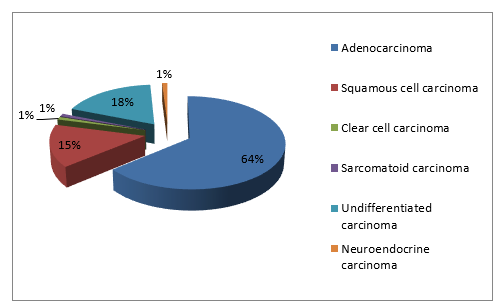
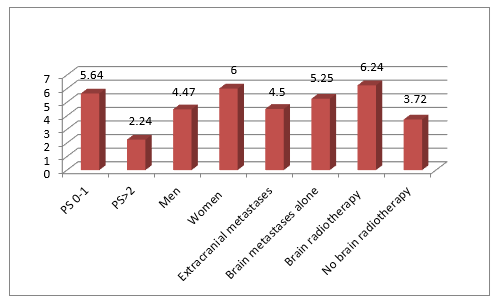
Among the 489 NSCLC cases analyzed, 80 patients (16.3%) developed BM. Average age was 57 years. A male predominance (91.3%) was noted with one gender male/female ratio of 10.4%. Smoking patients represented 81.3%. A performance status (PS) between 0-1 was found in 63.7% of patients. An adenocarcinoma was noted in 63.7% (Figure 1). The majority had extracranial metastases (78.8%). A chemotherapy based on platinum salts was administered in 57.5% of cases, with a number of cycles between 1 and 7 cures. 51.7% were treated with brain radiotherapy including only one patient who had undergone surgery before irradiation. The median follow-up was 5.07 months (range 1-36 months) (Table 1). Median PFS was 4.59 months (range 1-30 months) and the median OS was 4.62 months (range 0-36 months).Patients with a PS between 0-1 had better PFS (5.07 vs 3.57 months, p= 0.38; 95% CI[-1.954, 4.945]) and OS (5.64 vs 2.84 months, p= 0.09; 95% CI[-0.468,6.056]).We observed an improvement in survival with brain radiotherapy (PFS = 5.26 vs 4.33 months, p= 0.62; 95CI [-4.773,2.914] and OS = 6.24 vs 3.72 months; p=0.23; 95% CI [6.689,1.658]).In the presence of extra-cranial metastases the PFS was 4.47months vs 5.33 months in case of BM alone (p= 0.71; 95% CI [-3.857,5.576]) and OS at 4.5 months vs 5.25 months respectively (p= 0.73; 95% CI [-3.857,5.576]). Furthermore, men had a lower survival compared to women (PFS = 4.45 vs 5.50 months; p=0.65; 95% CI [-5.765, 3.660] and OS=4.47 vs 6 months; p=0.57; 95% CI [6.998,3.935]) (Figures 2,3). The survival analysis according to age was carried out by a simple linear regression which revealed an inverse association between these two variables as long as survival decreases with increasing age, but not statistically significant. (PFS: Beta = -0.274; p = 0.072 and OS: Beta = -0.136; p = 0.336).
Discussion
Lung cancer continues to be the leading cause of cancerrelated deaths worldwilde, with a higher prevalence of BM (19.9%) compared to other malignancies. It causes 40% of BM, all primitives combined [3]. NSCLC represent nearly 85% of lung cancers. The most common forms are: adenocarcinoma (ADK), squamous cell carcinoma, neuroendocrine tumors (small cell carcinoma, large cell carcinoma and carcinoid tumors) and large cell carcinoma. As for small cell lung cancer (SCLC), they represent nearly 15% of lung cancers [4]. More than 30% of patients with NSCLC develop BM (10 to 25% are synchronous and 50% to 80% are metachronous)) [5,6]. While in our series 16.3% had BM. In cases of NSCLC that are immediately metastatics, BM are present in 26.8% of cases of ADK, and in 15.9% of cases of squamous cell carcinoma [7]. Our patients had an average age of 57 years, males, smokers and ADK for the majority. A large number of studies have shown that smokers have a 15 to 30 times higher risk of developing lung cancer compared to non-smokers. There is also sufficient evidence to conclude that exposure to second-hand smoke, commonly known as passive smoking, can cause lung cancer [8]. Several other factors have been described as risk factors for lung cancer, including exposure to asbestos, arsenic, radon, and polycyclic aromatic hydrocarbons, unrelated to tobacco. Hypotheses about indoor air pollution (coal stoves and cooking fumes) have been relatively linked to an increase in non-tobacco-related lung cancer among women in some countries [9,10]. There are sometimes multiplicative interactions between tobacco and these other risk factors for lung cancer [9]. The management of lung cancer with BM is specific, very heterogeneous and depends on several prognostic factors: Histology including NSCLC (presence of mutations or not) and SCLC; the number of brain metastases: ≤ 3-5 lesions or > 3-5 lesions; symptomatic nature or not; life expectancy: ≤ 3 months or >3 months; clinical situation: oligometastatic, synchronous (primary bronchial tumor in place), metachronous (primary tumor treated) and multimetastatic. Prognosis of NSCLC patients with BM is poor. Three clinical trials from the Radiotherapy Oncology Group (RTOG) were pooled to result in Recursive Partitioning Analysis (RPA). This RPA is a prognostic index using patient age, Karnofsky Performance Status (KPS), control of primary tumors and extracranial metastases to define 3 categories of disease with a median survival ranging from 2.3 to 7.1 months [11]. Retrospective data were used to design the Diagnosis-Specific Graded Prognostic Assessment (DS-GPA) (available free at BrainMetGPA.com) [12]. Recently a series of GPA studies showed that for lung cancer with BM, significant prognostic factors for survival were age, KPS, extracranial metastases, and number of brain metastases. This made it possible to individualize four classes of diseases, with a median survival ranging from 3 to 14.8 months [12]. A retrospective study demonstrated a survival benefit in patients presenting alterations of the EGFR genes (Epidermal Growth Factor Receptor) and ALK (Anaplastic Lymphoma Kinase), compared to those without oncogenic modifications. The incorporation of the effect of molecular data on survival in these patients led to the creation of the new Lung-molGPA, for better management [13]. In our series, age was inversely associated with survival and patients with a PS between 0-1 had better survival, in accordance with the literature. Furthermore, men had a lower survival compared to women. An improvement in survival was noted in the absence of extra-cranial metastases in agreement with the data from the studies reported. The therapy is multimodal, combining local treatments (surgery and/or radiotherapy), systemic treatments and supportive care. The challenge is to improve survival and quality of life often impaired by neurological repercussions. The role of surgery in the treatment of single BM is well defined and remains possible in case of multiple BM. Surgical indications and additional treatments must be discussed on a case-by-case basis, keeping quality of life as the objective [8]. In our context, only one patient had a resection of his brain metastasis before irradiation. Total brain radiotherapy quickly improves the symptomatology and cerebral control, but with limited indications today. We observed an improvement in survival with brain radiotherapy in our patients in the same sense of the literature. Stereotactic Body Radiation Therapy (SBRT)have completely replaced brain irradiation both for patients suffering from existing metastases than for those who have been resected. Its relevance in terms of conservation of cognitive functions remains to be clearly demonstrated but the demand is increasingly strong [14]. None of our patients were able to benefit from the stereotactic radiotherapy due to its unavailability in our center. The effectiveness of systemic treatments by chemotherapy, targeted therapies and immunotherapy may be different between extra-cerebral locations and brain, due to the blood-brain barrier. The latter, although altered in the presence of BM, is not completely permeable [15]. For this work, we were not able to update our database regarding the presence of EGFR mutation or ALK rearrangement, which constituted an information bias that did not allow to evaluate survival in this population group. Nevertheless, in our institution, the search for these anomalies is done systematically in metastatic patients who subsequently receive targeted therapy appropriate to their oncogenic addiction. The prognosis of the disease remains poor with a median survival varying from 3 to 15 months [12], it can reach up to 47 months in patients presenting an EGFR or ALK alteration [13]. Overall survival in our series had reached 36 months with a median of more than 4.5 months. This result remains consistent with literature.
Conclusion
The poor prognostic factors historically described are the absence of control of the primary tumor, performance status: KPS >2, age ≥60 years, number of BM≥3, non-ADK type histology, absence of molecular alteration (EGFR/ALK).We checked the presence of association between the risk factors studied including age, female gender, PS < 2, brain radiotherapy, absence of extracranial metastases on the one hand, and better survival on the other hand, without statistical significance. These results are probably due to the retrospective study design which is accompanied by several types of selection and information bias.
Conflict of interest
The authors declare no conflict of interest.
Author Contributions
Imane Ouafki is the main author of this work. She did the initial writing of the article and integrated all the corrections. She contributed to improving the form and content of the text. She generally enriched this clinical study. All authors read and approved the final version of the manuscript.
Ethical and Regulatory Aspects
The non-opposition of patients to the use of their data has been verified before analysis by signing informed consent.
References
- Blibech H, Moatemri Z, Dabboussi S, Mhamdi S, Aichaouia C, et al (2017). Métastases cérébrales du cancer du poumon : facteurs pronostiques.Revue des Maladies Respiratoires. 34(Supplement): A83.
- Faguer R, Terminassian A, Hureaux J, Soulié P, Jadaud E, et al (2012). Prise en charge chirurgicale des métastases cérébrales des cancers bronchopulmonaires. Revue des Maladies Respiratoires Actualités 4(6): 550-557.
- Tabouret E, Bauchet L, Carpentier AF (2013). Brain metastases epidemiology and biology. Bull Cancer. 100(1): 57-62.
- Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG (2015). WHO Classification of tumours of the lung,pleura, thymus and heart pp. 7.
- Ulahannan D, Khalifa J, Faivre Finn C, Lee SM (2017) Emerging treatment paradigms for brain metastasis in non-small-cell lung cancer: an overview of the current landscape and challenges ahead. Ann Oncol. 28(12): 2923-2931.
- Patchell RA (2003) The management of brain metastases. Cancer Treat Rev. 29(6): 533‑5
- Cagney DN, Martin AM, Catalano PJ, Redig AJ, Lin NU et al (2017). Incidence and prognosis of patients with brain metastases at diagnosis of systemic malignancy: a population-based study. Neuro-Oncol 19(11): 1511‑15
- Youlden DR, Cramb SM, Baade PD, Peter D (2008) The international epidemiology of lung cancer: geographical distribution and secular trends. J Thorac Oncol 3(8): 819- 831.
- Dixsaut G (2013). Cancer broncho-pulmonaire, nouvelle approche épidé Revue des Maladies Respiratoires Actualités. 5(5): 581-590.
- Malhotra J, Malvezzi M, Negri E, Vecchia L, Boffetta P (2016). Risk factors for lung cancer worldwide. Eur Respir J 48(3): 889-902.
- Gaspar L, Scott C, Rotman M, Asbell S, Phillips T, et al. (1997) Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 37(4):745-751.
- Sperduto PW, Kased N, Roberge D, Xu Z, Shanley R, et al. (2012) Summary Report on the Graded Prognostic Assessment: An Accurate and Facile Diagnosis-Specific Tool to Estimate Survival for Patients With Brain Metastases. J Clin Oncol 30(4): 419‑4
- Sperduto PW, Yang TJ, Beal K, Hubert Pan, Paul D Brown, et al. (2016) The effect of gene alterations and tyrosine kinase inhibition on survival and cause of death in patients with adenocarcinoma of the lung and brain metastases. Int J Radiat Oncol Biol Phys 96(2): 406-413.
- Latorzeff I, Antoni D, Gaudaire Josset S, Feuvret L, Tallet Richard A, et al. (2016) Radiothérapie des métastases céré Cancer Radiother 20(suppl): S80-S87.
- Le Rhun É, Dhermain F, Noël G, Reyns N, Carpentier A, et al. (2015) ANOCEF guidelines for the management of brain metastases. Cancer Radiother 19(1): 66‑71.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.