Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Retroperitoneal Perforation of Colon Cancer, A Rare Cause of Diagnostic Wandering, about A Case and Literature Review
*Corresponding author: Nguele Ndjota, Department of Visceral Surgery, University Hospital of Libreville, BP: 10941 Libreville/Gabon.
Received: November 09, 2023; Published: November 22, 2023
DOI: 10.34297/AJBSR.2023.20.002735
Summary
Introduction: Colonic perforation is a rare complication of colon tumors. It is the source of an alarming digestive picture. The authors therefore report the case of perforated right colon cancer in the retroperitoneum, emphasizing the misleading clinic and its management.
Observation: 52-year-old patient from the countryside for the management of non-febrile right flank and iliac fossa pain. This picture indicated a right inguinal hernia cure in a local medical center without clinical improvement despite well-conducted analgesia and antibiotic therapy. Examination, on admission, noted apyrexia, abdominal meteorism, iliac abdominal and right flank tenderness. Biology noted the absence of hyperleukocytosis. Ultrasound suspected appendicular peritonitis and complementary abdominal CT was a retroperitoneal abscess. On exploratory laparotomy, serohematic effusion, agglutination of slender loops in the right iliac fossa covering abundant fecaloid retroperitoneal effusion was noted. The patient’s instability justified the interruption of the procedure after retroperitoneal aspiration-drainage and a transverse ileocolonic anastomosis. The patient was followed up on postoperative day 10 for a right hemicolectomy revealing a posterior caecal perforation. The postoperative period was complicated by suppuration of the wound and the discharge was authorized on day 10 of the recovery. Histological analysis of the specimen showed invasive liberkunian adenocarcinoma on colonic diverticulosis. The patient was secondarily referred to oncology for adjuvant chemotherapy.
Conclusion: Retroperitoneal perforation of digestive cancer is exceptional, which may explain the non-conforming therapeutic attitudes encountered in the patient. Imaging plays a major role in this process and guides the surgeon.
Keywords: Cancer, Colon, Perforation, Retroperitoneum
Introduction
The perforation of the colon corresponds to a solution of continuity of the colonic wall whose origin is variable. This is a rare complication of colon cancer compared to tumor occlusion [1]. Perforation of the colon can occur in patients with acute colonic occlusion and would be the consequence of ischemia and parietal necrosis, which is more common in the cecum. It may also be related to tumor ulceration through the colonic wall. This perforation usually causes the fecal contents to leak into the free peritoneal cavity. The resulting clinical picture is noisy: stercoral peritonitis, a source of septic shock and death in the absence of adequate management. This condition therefore requires, as soon as the diagnosis is made, curative surgery after optimal resuscitation and broad-spectrum antibiotic therapy. The authors report the case of perforated right colon cancer in the retroperitoneum, emphasizing the symptomatic pauci clinic and its management.
Observation
The patient was a 52-year-old patient, with no history, who had come from Bouée, a secondary town in northeastern Gabon, for the management of pain of the right iliac fossa (FID) and flank. This isolated pain, without fever, had been progressing for more than 2 weeks. She had prompted a consultation at the local medical Center where the diagnosis of symptomatic inguinal hernia was made, and the patient was operated on. Postoperatively, he was put on antibiotics and analgesics. The persistence of the pain motivated the patient to consult in Libreville on the 7th postoperative day. On admission, the examination noted apyrexia, asthenia grade II of the WHO, unquantified weight loss, abdominal meteorism, abdominal defense predominant in FID and in the right flank. The hypothesis of acute appendicitis complicated by an abscess was suspected. At the paraclinical level, the complete blood count noted leukocytes at 6000/mm3, anemia at 7g/dL, and positive C-Reactive Protein at 200mg/L. Moderate impairment of renal function was noted with a normal field assessment (retroviral serology and blood glucose). Abdominal ultrasound suspected appendicular peritonitis.
Complementary abdominal Computed Tomography (CT) was in favor of a predominant retroperitoneal fluid and airborne collection in the right flank and FID, right perirenal. It referred to a retroperitoneal abscess without specifying its etiology. Low-grade bilateral pleurisy was noted on chest x-ray. In front of the blackboard, we had indicated an exploratory laparotomy and open drainage. The surgical procedure consisted of a median xiphopubic laparotomy under general anesthesia. She found intraperitoneal serohematic effusion, reactive ileocecal appendicitis, agglutination of ileal loops in the flank, and in FiD with a right mesocolic necrotic closet (Figure 1).

Figure 1: Intraoperative view with right mesocolic cupboard (yellow arrow) collapsed by suction cannula.
His collapse revealed a retroperitoneal, purulent and fecaloid effusion abundant as evidence of a posterior perforation of the right colon. We performed aspiration followed by retroperitoneal drainage. A sample of the pus was taken for bacteriological analysis. A trilateral ileocolonic shunt associated with drainage was performed as a first-line treatment due to the patient’s hemodynamic instability. Postoperatively, the patient was put on triple antibiotic therapy consisting of cefepime, metronidazole and gentamicin. High-protein oral feeding was allowed from the second day (D2) postoperatively. A follow-up thoraco-abdominal CT scan performed on D9 showed regression of the right retroperitoneal effusion (Figure 2) and bilateral pleurisy.
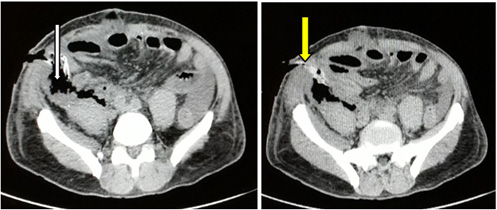
Figure 2: J9 abdominal CT scan, showing a retro pneumoperitoneum (white arrow) and the exteriorized drain (yellow arrow).
The patient was admitted to the operating room on day 11. Intraperitoneal effusion, retroperitoneal residual purulent effusion (Figure 3) was not noted and was followed by a right hemicolectomy. The surgical specimen had a perforation of the posterior wall of the cecum (Figure 4).
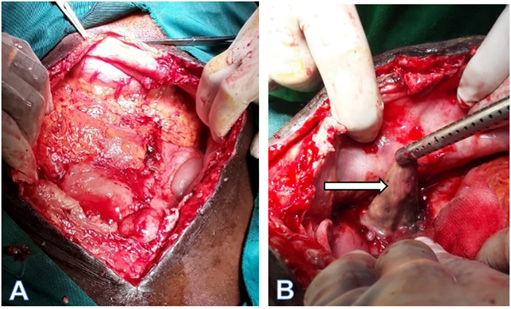
Figure 3: intraoperative images on D11 (rework).Has. At opening, there is no free intraperitoneal effusion. B. Retroperitoneal pus aspiration (white arrow).
The post-operative medical treatment was repeated identically after this retake. The postoperative outcome was complicated by an infection of the surgical wound with Acinetobacter Baumannii, intermediate to cefepime but sensitive to ofloxacin, justifying the modification of the antibiotic treatment. The exit was allowed on D10 after the resumption. The patient was seen again one month after the operation with good healing of the surgical wound (Figure 5).
Histological analysis of the specimen, hampered by inflammation of the mesocolon, revealed a grade 2 invasive liberkunian adenocarcinoma classified as pT4a pNx pMx with lymphatic emboli occurring on colonic diverticulosis. The limits of surgical excision were healthy. The secondary discussion of the case at the multidisciplinary consultation meeting indicated that adjuvant chemotherapy was well tolerated by the patient.
Discussion
Colonic perforation accounts for 20% of emergencies caused by colorectal tumors after occlusions [1]. When perforation occurs at the tumor site, peritoneal contamination is usually localized, whereas near the tumor (diastatic perforation), the digestive contents spread throughout the cavity. It then leads to generalized peritonitis and septic shock [1,2]. Posterior perforation of the colon related to cancer is a localized form, rarely reported in the literature, with about fifteen cases cited since the first description in 1983 [3]. The digestive contents spill into the retroperitoneum as in our case and explains a less noisy a specific clinic revealed by lumbar back pain [4] associated or not, with abdominal meteorism [5], thigh pain [5,6], or even necrosis of the thigh [7]. This could explain, apart from the absence of imaging, the wandering or misdiagnosis in this pathology [5] and the inappropriate surgery performed by the first practitioner in our case. At the paraclinical, the gold standard for the diagnosis of colonic perforation of tumor origin is abdominal computed tomography [1,8]. It can be used to identify pneumoperitoneum or retro pneumoperitoneum or focal parietal thickening. These signs were not described in our case marked only by retroperitoneal effusion. However, in general, in the absence of a CT scan, in front of a clinic with a strong suspicion of perforation, ultrasound or x-ray of the abdomen without preparation can be used as a first-line treatment [9]. In this indication, abdominal ultrasound appears to have better sensitivity than ASP [10]. In our practice, which is too often lacking in CT scans, the realization and interpretation of these two diagnostic means should be mastered by enough practitioners. Although strongly recommended, CT scans should never delay patient management. The crushing nature of the picture should systematically make biology look for an immuno-depressant condition (HIV infection, diabetes, etc.).
Regarding treatment, in the case of perforation on colonic carcinoma, antibiotic therapy targeting mainly gram-negative bacilli and anaerobic bacteria is always proposed [1], combined with optimal pre, per and post operative resuscitation. The surgical approach here remains guided by the surgeon, dominated in the literature by laparotomy with a less frequent use of laparoscopy [11]. According to Crowder and Cohn, [12] “the surgical management of perforation and peritonitis or abscess resulting from perforation must take precedence over that of cancer.” This therefore suggests a two-stage surgery as described by Tsukuda, et al., [13], and usually imposed by clinical instability related to fluid-electrolyte imbalance, bacterial proliferation, pre-existing comorbidities, or unfavorable local conditions. In this observation, the procedure was shortened due to hemodynamic instability. Faced with this, the surgical team must keep in mind the interest of limiting damage to the patient, the “damage control”. This concept is now extended to non-traumatic surgical emergencies [1], with peritonitis [14] at the forefront. This allows an emergency to be carried out and the major intervention to be postponed. Here, the instability warranted drainage of the collection in the first place and a secondary right hemicolectomy. In an adverse context, [1] recommend a hemicolectomy followed by a terminal ileostomy. However, under optimal conditions, in the case of a right colonic perforation, a hemicolectomy is recommended followed by anastomosis [11]. These procedures are suggested if no significant increase in operating time is required [1].
Conclusion
Retroperitoneal abscess as an initial manifestation of perforated colon carcinoma is rare. This rare complication explains, in the absence of imaging, a diagnostic error or even inappropriate surgery. As a matter of urgency, it requires drainage of the abscess followed by a cold hemicolectomy, a right hemicolectomy plus ileo- colonic anastomosis. Awareness of this possible complication of colon cancer by doctors, and surgeons in particular, will lead to improved diagnosis and refinement of treatment.
Acknowledgments
None.
Conflicts of Interest
None.
References
- Pisano M, Zorcolo L, Merli C, Stefania Cimbanassi, Elia Poiasina, et al. (2018) 2017 WSES guidelines on colon and rectal cancer emergencies: obstruction and perforation. World J Emerg Surg 13(1): 36.
- Zielinski MD, Merchea A, Heller SF, You YN (2011) Emergency management of perforated colon cancers: how aggressive should we be? J Gastrointest Surg 15(12): 2232-2238.
- Maglinte DDT, Pollack HM (1983) Retroperitoneal abscess: A presentation of colon carcinoma. Gastrointest Radiol 8(1): 177‑1
- Yamada T, Ikeya T, Ogawa T, Minoru Nakano, Hidemi Ogura, et al. (2002) A hemophagocytic syndrome-like condition after emergency colectomy for perforated colon cancer: report of a case. Surg Today 32(3): 278‑2
- Ruscelli P, Renzi C, Polistena A, Alessandro Sanguinetti, Nicola Avenia, et al. (2018) Clinical signs of retroperitoneal abscess from colonic perforation. Medicine 97(45): e13176.
- Montori G, Di Giovanni G, Mzoughi Z, Cedric Angot, Sophie Al Samman, et al. (2015) Pneumoretroperitoneum and Pneumomediastinum Revealing a Left Colon Perforation. Int Surg 100(6): 984-988.
- Takakura Y, Ikeda S, Yoshimitsu M, Takao Hinoi, Daisuke Sumitani, et al. (2009) Retroperitoneal abscess complicated with necrotizing fasciitis of the thigh in a patient with sigmoid colon cancer. World J Surg Oncol 7(1): 74.
- Zissin R, Hertz M, Osadchy A, Even Sapir E, Gayer G (2008) Abdominal CT findings in nontraumatic colorectal perforation. Eur J Radiol 65(1): 125‑1
- Imuta MK, Awai Y, Nakayama YM, Asao C, Matsukawa T, et al. (2007) Multidetector CT findings suggesting a perforation site in the gastrointestinal tract: analysis in surgically confirmed 155 patients. Radiat Med 25(3): 113-118.
- Chen SC, Yen ZS, Wang HP, Lin FY, Hsu CY, et al. (2002) Ultrasonography is superior to plain radiography in the diagnosis of pneumoperitoneum. Br J Surg 89(3): 351-354
- Yang XF, Pan K (2014) Diagnosis and management of acute complications in patients with colon cancer: bleeding, obstruction, and perforation. Chin J Cancer Res 26(3): 331‑3
- Crowder Jr VH, Cohn Jr I (1967) Perforation in cancer of the colon and rectum. Dis Colon Rectum 10(6): 415-420.
- Tsukuda K, Ikeda E, Miyake T, Yoko Ishihara, Hiroyuki Watatani, et al. (2005) Abdominal wall and thigh abscess resulting from the penetration of ascending colon cancer. Acta Med Okayama 59(6): 281‑28
- Person B, Dorfman T, Bahouth H, Osman A, Assalia A, et al. (2009) Abbreviated emergency laparotomy in the non-trauma setting. World J Emerg Surg 4: 41.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.