Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
The Confounding Effects of Chronic THC Use: A Case Report
*Corresponding author: Leonard Ranasinghe, Emergency Medicine and Director of Fourth-Year Electives and Sub-Internships, California North state University College of Medicine, Elk Grove, CA, United States of America.
Received: October 25, 2023; Published: October 30, 2023
DOI: 10.34297/AJBSR.2023.20.002719
Abstract
Cannabinoids are known to have clinical significance in relieving GI symptoms, such as nausea and vomiting. However, the increasing incidence of Cannabinoid Hyperemesis Syndrome (CHS), where patients have episodes of cyclic vomiting and abdominal pain, seems to contradict their intended medicinal use. This case report details the observation of CHS in a young woman with a six-month history of GI distress, without any known associated conditions. She visited multiple emergency departments before this visit with no resolution to her condition. Although she initially denied any drug use, her most recent visit to the emergency department revealed a positive urine drug screen for THC. CHS is a rare condition and an uncommon diagnosis, which made this case particularly difficult to diagnose at first glance. While hot showers and baths, topical capsaicin, and other antiemetic medications can help alleviate the symptoms of CHS, there is no established treatment regimen. Thus, the most effective method of resolving the symptoms of CHS is cessation of THC use. This case report is intended to promote awareness of CHS among medical professionals and THC users so that this condition can be recognized and resolved in future cases. Furthermore, it provides a call to focus future research on discovering primary therapeutics and factors that make some patients more susceptible to CHS than others.
Keywords: Cannabinoids, Cannabinoid Hyperemesis Syndrome (CHS), Chronic THC use, Anti- emetics, Topical capsaicin, Marijuana, Endocannabinoid system
Introduction
Although cannabinoids are often used to alleviate symptoms of GI distress, chronic cannabinoid use in both medicinal and recreational users has been found to produce the opposite effect in some cases [1]. When California legalized the use of recreational marijuana in 2016, both primary marijuana usage and the incidence of emergency room visits related to primary marijuana usage increased dramatically as a result [2].
From 2016 to 2019, there was a reported 89% increase in marijuana- related emergency department visits and admissions [2]. In addition to these upward trends in marijuana-related emergency department visits, there has also been observed increases in vomiting and abdominal pain due to marijuana use [3]. Since marijua na is commonly used medicinally as an anti-emetic, its potential to contribute to increased vomiting and GI distress in users is puzzling.
It has been found that some long-term cannabis users can develop Cannabinoid Hyperemesis Syndrome (CHS), causing undesired side effects of vomiting, nausea, cramping abdominal pain, and other GI symptoms due to chronic THC use [4]. CHS is a rare effect of chronic marijuana/cannabinoid usage, characterized by THC use spanning multiple years. It is an enigmatic diagnosis given that medicinal cannabinoid usage is intended to relieve GI symptoms while chronic usage can aggravate these problems. Previous cases have shown symptoms of severe vomiting occurring years after the onset of cannabis use in young patients, where usage began between the ages of 12 and 19 years old [5]. With an increasing number of teens and young adults using marijuana and related products [6,7], cannabinoid users and medical staff alike need to be aware and well-informed of the rare and often unforeseen effects that cannabinoid usage can present.
Case Presentation
A 21-year-old woman presented to the emergency department with a six-month history of nausea, vomiting, and abdominal cramping. During previous emergency department visits for similar symptoms, the patient was treated with Ondansetron for nausea, and Amoxicillin, Omeprazole, and Rifabutin for H. pylori. Despite multiple emergency department visits, no clear resolution was found for her symptoms.
The patient continued to experience sharp, recurring, and burning abdominal pain for the past 3 weeks, with no pain noted prior to the onset 3 weeks ago. At a recent ED visit, she was found to have a variety of abnormal lab results (Table 1) and a negative abdominal ultrasound. To alleviate these symptoms, she was given a GI cocktail and prescriptions for Dicyclomine, Ondansetron, and Omeprazole at home. She was noted to appear comfortable and without distress upon final re-evaluation before discharge (Table 1).
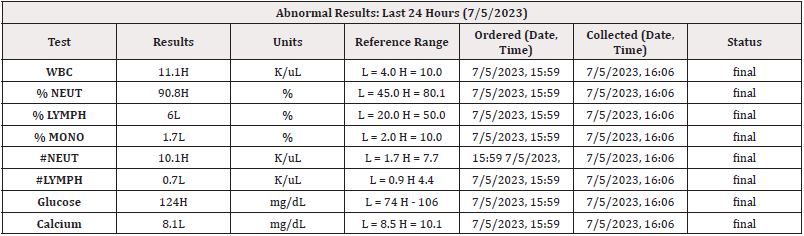
Table 1: Abnormal Lab Results from 7/5/2023.
Note*: WBC: white blood cell count; %NEUT: percentage of neutrophils; %LYMPH: percentage of lymphocytes; %MONO: percentage of monocytes; #NEUT: number of neutrophils; #LYMPH: number of lymphocytes.
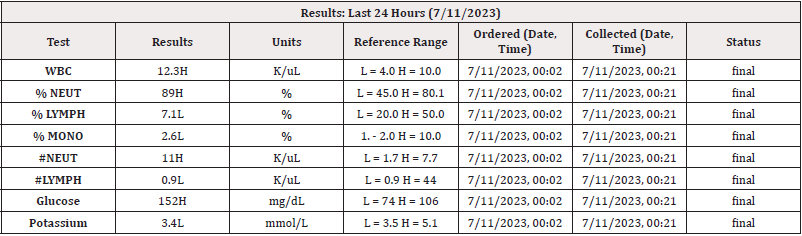
Table 2: Lab Results from 7/11/2023.
Note*: WBC: white blood cell count; %NEUT: percentage of neutrophils; %LYMPH: percentage of lymphocytes; %MONO: percentage of monocytes; #NEUT: number of neutrophils; #LYMPH: number of lymphocytes.
Six days later, the patient returned to the emergency department due to severe abdominal pain and nausea, multiple episodes of vomiting, abdominal cramping, and mild diarrhea after eating pizza 20 minutes prior. Ondansetron taken at home did not help resolve her symptoms. Upon examination, bowel sounds were hypoactive, white blood cell count was slightly elevated, and she was hypokalemic (Table 2). The hypokalemia was treated with one dose of potassium orally (Table 2).
Of interest, a urine drug screen came back positive for THC and amphetamines. Treatment with intravenous Ondansetron offered no relief for her symptoms, but subsequent intravenous doses of 10 mg of Metoclopramide and 25 mg of Diphenhydramine offered complete relief and ultimate discharge with no further nausea or vomiting. At discharge, the patient was advised to stay on a clear liquid diet for the next few days and was prescribed Metoclopramide and Diphenhydramine. Additionally, the patient was informed that chronic THC use can cause the severe and long-term symptoms that she was experiencing. She was advised to seek help, stop using drugs, and potentially enter a drug rehabilitation program. The patient was reportedly receptive to this information and was subsequently discharged.
Pathophysiology
Delta-9-Tetrahydrocannabinol (THC) is one of the primary psychoactive elements of marijuana [8]. THC has an interactive effect on the body’s Endocannabinoid System (ENS), which is specifically mediated by cannabinoid receptors 1 and 2 (CB1 and CB2) located in the central and peripheral nervous systems, as well as in immune cells [9]. This prevalence of cannabinoid receptors in immune cells may explain the increased WBC count and neutrophil count in our patient. The common utilization of THC in treating nausea and vomiting comes from its ability to bind CB1 receptors in the central nervous system (specifically the cerebellum, hypothalamus, and vomiting centre of the medulla) and the peripheral nervous system (specifically the enteric plexus and presynaptic parasympathetic nervous system) [8]. Stimulation of CB1 receptors can inhibit vomiting, but larger doses of THC can lead to blockade and downregulation of CB1 receptors, thus inducing vomiting [8]. In addition, due to the lipophilic nature of cannabinoids, chronic THC use can cause accumulation of THC in cerebral fat, causing severe nausea and vomiting [8].
Another notable mechanism of the CB1 receptor is its involvement in thermoregulatory processes in the hypothalamus [10]. This regulation is dose-dependent: high concentrations of cannabinoids act on CB1 receptors to cause hypothermia due to decreased heat production [10]. Similar to the CB1 receptor, the Transient Receptor Potential Vanilloid 1 (TRPV1) receptor of the ENS has also been observed to produce thermoregulatory effects in the hypothalamus with overstimulation [2]. The TRPV1 receptor is activated by endocannabinoids, as well as nociceptive heat stimulation [11]. Both the CB1 and TRPV1 receptors significantly impact the hypothermic and hyperemesis symptoms associated with CHS, thus providing potential therapeutic targets for this condition.
However, as seen in the literature, patients have had success with many different symptom resolutions including Ketorolac, Pantoprazole, IV fluids, Hydromorphone, Rocephin, and hot showers [12]. Although there is no clearly established treatment method for CHS that results in the most successful outcome, it is evident that the most effective method of symptom resolution is removing the source of the problem through cessation of THC use.
Cannabinoids are also known to interact with many different cytochrome P450 enzymes (CYPs) crucial to metabolism, including CYP2C9, CYP2E1, and CY3A4 [13]. Many common anti-emetic drugs are metabolized by these CYPs. Ondansetron is known to be metabolized by CYP1A2, CYP2D6, and CYP3A4, with CYP3A4 playing the leading role in turnover for this drug [14]. Omeprazole is also known to be metabolized by and inhibit CYP 3A4 [15]. However, the metabolism of dicyclomine is unclear, as it is known to be metabolized by the liver but has not been connected to any CYPs [16].
Discussion
As seen in the present case, Cannabinoid Hyperemesis Syndrome (CHS) was not at the forefront of the differential diagnoses tested, as it is a unique and uncommon diagnosis.
However, due to the increasing number of cannabinoid users and increased incidence of CHS, it is crucial to identify the condition early. This case highlights the necessity of recognizing CHS in order to provide the proper treatment. Although the patient’s history of THC use was initially unknown, the patient’s initial presentation did meet the central criteria of CHS-symptoms occurring for a minimum of 6 months, frequent episodic vomiting and abdominal pain, and short-term relief when cannabis use was stopped [17]. Despite her recurrent presentation of these symptoms, she was still left without a clear diagnosis for 6 months. This is likely because her primary presentation of abdominal pain with recurrent nausea and vomiting is characteristic of many different GI disorders, making an initial diagnosis of CHS difficult and uncommon.
However, a urine drug screen can make this diagnosis more definitive if it comes back positive for THC use, as it did with our patient. The adverse effects of prolonged THC use may also be explained by the increasing percentage of THC available in marijuana products. Before marijuana was legalized in the 1990s, the THC percentage found in most marijuana products was less than 2% [18]. From 1995 to 2017, the average concentration of THC found in marijuana products rose from 4% to 17%, and in states with large marijuana markets, such as California, products with up to 25% THC can be found [13,19]. Thus, the increasing dosage of THC in the marijuana products used by consumers could also be causing the symptoms of chronic THC use to appear with an increased incidence and at earlier ages than expected, as underscored by the diagnosis of CHS in our 21- year-old patient.
One therapy for alleviating the symptoms of CHS is taking hot showers or baths, as it is known that endogenous cannabinoids and CB1 receptors take part in thermoregulatory processes in the hypothalamus [10]. Warm water helps to counteract the effects of CB1 receptor stimulation by decreasing stimulation of the sympathetic nervous system; it can also induce cutaneous vasoconstriction that reduces abdominal pain through diversion of the splanchnic blood vessels [10].
It is evident in the literature that one medication that is able to replicate this warm water effect is topical capsaicin [11]. Capsaicin has high specificity and strong binding capacity to TRPV1 receptor, thus preventing overstimulation and desensitization of the ENS to cannabinoids. Therefore, treatment with capsaicin in cases of CHS can be comparable to the relief felt from patients taking hot showers or baths due to TRPV1 activation [11]. However, it is also important that topical capsaicin can have adverse side effects including burning, itching, redness, and irritation at the application site, along with more general symptoms of coughing, sneezing, throat irritation, pain, and swelling [20]. Nevertheless, it is important for health care services to be aware of topical capsaicin as a potential treatment option for patients with CHS as studies have shown that the medication can provide significant anti-emetic effects [21,22].
As seen in the case presentation, many standard drug regimens were employed in attempts to reduce the patient’s symptoms. Our patient responded well when given Metoclopramide and Diphenhydramine to alleviate her symptoms, while treatment with Ondansetron and Omeprazole provided no relief. Although the reason for the inefficacy of these medications is unclear, it is possible that the patient’s cannabinoid use could have caused the induction of the cytochrome P450 enzymes that metabolize Ondansetron and Omeprazole [13-15].
Conclusion
Cannabinoid Hyperemesis Syndrome (CHS) is an adverse effect of chronic cannabinoid use that usually presents with cyclic episodes of nausea, severe abdominal pain, and vomiting. While CHS incidence has been on the rise in recent years alongside increasing trends in cannabinoid use, it can be hard to diagnose initially because it presents like many other GI conditions. Because of this, medical professionals should have a clear understanding of the patient’s history of present illness and social history (particularly drug use), which would provide indication to perform a drug screen to help diagnose CHS most accurately in patients presenting with relevant GI symptoms. With cannabinoid usage increasing in the adolescent and young adult population, medical professionals must be aware of how CHS presents so that they can accurately diagnose CHS, treat this condition effectively, and educate patients on the potential risks of long-term cannabis use.
Acknowledgements
None.
Conflict of Interest
None.
References
- Hemant Goyal, Umesh Singla, Urvashi Gupta, Elizabeth May (2017) Role of cannabis in digestive disorders. Eur J Gastroenterol Hepatol 29(2): 135-143.
- Neal Doran, David Strong, Mark G Myers, John B Correa, Lyric Tully (2021) Post-legalization changes in marijuana use in a sample of young California adults. Addict Behav 115: 106782.
- Joseph V Pergolizzi, Jo Ann LeQuang, John F Bisney (2018) Cannabinoid Hyperemesis. Med Cannabis Cannabinoids 1(2): 73-95.
- ND Vaziri, R Thomas, M Sterling, K Seiff, MV Pahl, et al. (1981) Toxicity with intravenous injection of crude marijuana extract. Clin Toxicol 18(3): 353-366.
- JH Allen, GM de Moore, R Heddle, JC Twartz (2004) Cannabinoid hyperemesis: cyclical hyperemesis in association with chronic cannabis abuse. Gut 53(11): 1566-1570.
- (2014) Marijuana and Teens. American Academy of Child and Adolescent Psychiatry.
- Marijuana and hallucinogen use among young adults reached all-time high in 2021 (2022). National Institutes of Health (NIH).
- Marvin Louis RY Lu, MD Agito (2015) Cannabinoid hyperemesis syndrome: Marijuana is both antiemetic and proemetic. Cleve Clin J Med 82(7): 429-434.
- S Chayasirisobhon (2020) Mechanisms of Action and Pharmacokinetics of Cannabis. Perm J 25: 1-3.
- John R Richards, Jeff M Lapoint, Guillermo Burillo Putze (2018) Cannabinoid hyperemesis syndrome: potential mechanisms for the benefit of capsaicin and hot water hydrotherapy in treatment. Clin Toxicol (Phila) 56(1): 15-24.
- Magdalene M Moran, Arpad Szallasi (2018) Targeting nociceptive transient receptor potential channels to treat chronic pain: current state of the field. Br J Pharmacol 175(12): 2185-2203.
- Norman Khalid, Muhammad Abdullah, Musa Khalil, Muhammed A Afzal, Mulham Hindawi (2023) Cannabis Hyperemesis Syndrome in a Young Patient: A Case Report and Literature Review. Cureus 15(8): e43868.
- McIntyre C (2022) Cannabinoid Overview. NetCE.
- GlaxoSmithKline (2010) ZOFRAN® (ondansetron hydrochloride) Injection: Prescribing Information.
- Shirasaka Y, Sager JE, Lutz JD, Davis C, Isoherranen N (2013) Inhibition of CYP2C19 and CYP3A4 by omeprazole metabolites and their contribution to drug-drug interactions. Drug Metab Dispos 41(7): 1414-1424.
- (2017) Dicyclomine. National Institute of Diabetes and Digestive and Kidney Diseases.
- Frederick Chu, M Cascella, (2022) Cannabinoid Hyperemesis Syndrome.
- Elizabeth Stuyt (2018) The Problem with the Current High Potency THC Marijuana from the Perspective of an Addiction Psychiatrist. Mo Med 115(6): 482-486.
- Elena Vidrascu (2019) Cannabinoid Hyperemesis Syndrome: Yes, Teens, Smoking Marijuana Too Much CAN Hurt You. JPHMP Direct.
- (2020) Capsaicin. MedlinePlus.
- Vivian Kum, Adrienne Bell, Wei Fang, Elizabeth VanWert (2021) Efficacy of topical capsaicin for cannabinoid hyperemesis syndrome in a pediatric and adult emergency department. Am J Emerg Med 49: 343-351.
- Laurel Dezieck, Zackary Hafez, Albert Conicella, Eike Blohm, Mark JO Connor, et al. (2017) Resolution of cannabis hyperemesis syndrome with topical capsaicin in the emergency department: a case series. Clin Toxicol (Phila) 55(8): 908-913.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.