Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
4R Method to Dealing with Patient Initiated Harassment: A Medical Student Workshop
*Corresponding author: Neha Madangarli, Resident Physician, Department of Psychiatry, University of Tennessee, USA.
Received: December 19, 2023; Published: January 05, 2024
DOI: 10.34297/AJBSR.2024.21.002798
Educational Objectives
By the end of this activity, learners will be able to:
a) Understand the prevalence of workplace harassment as it pertains to different levels of training in the healthcare field.
b) Feel encouraged to report the issue, regardless of perceived severity.
c) Learn practical strategies to respond to patient initiated sexual harassment.
d) Recognize available resources and strategies to address encounters and emotionally process experience.
Abstract
A. Introduction: Sexual harassment is a common phenomenon occurring in the clinical setting with patients being the most common source. Students are often educated about responding to sexual harassment coming from superiors or colleagues but are unaware how to respond to patients. They often feel that they are overreacting when reporting or simply do not know how to report.
B. Methods: The method is summarized by the 4 R’s: respond, report, reflect, react. This method gives practical strategies on how to respond to and report sexual harassment and emphasizes the need to reflect on emotional responses as well as the need to react properly when witnessing the act. The workshop is designed to be interactive with a standardized patient encounter followed by a lecture.
C. Results: Participants on average gave positive feedback for the workshop. The level of instruction and realism of the scenario were rated to be better than average, and most students stated that the workshop should be offered again.
D. Discussion: The 4R method builds on previously published methods of dealing with patient initiated sexual harassment. It gives practical strategies for responding with variations depending on comfortability level while also focusing on tone and body language. It also emphasizes the need for victims to emotionally process encounters and for bystanders to check in again with victims after some time. This resource can be used for pre-clinical medical students but can also be adapted to any healthcare profession and level.
Introduction
Gender based discrimination (GBD) is defined as unequal or disadvantageous treatment of an individual or group of individuals based on their gender. Sexual harassment, characterized by unwelcome conduct or advances based on a person’s sex or appearance, is a form of illegal gender-based discrimination. Studies conducted by the Massachusetts General Hospital Gender Equity Task Force showed that the most common source of gender-based discrimination amongst internal medicine, anesthesia, and surgery residents was from patients [1]. Women were significantly more likely to experience GBD, however less than 5% of total respondents formally reported their encounters. Furthermore, a study in 2019 interviewing Canadian medical students showed 807 incidents of sexual harassment from 188 students, with the victims being predominantly female [2]. These students also answered that they often did not report the issue as they did not know how, did not want to draw attention to themselves, or did.
not think anything would come of it. A meta-analysis of 253 studies of workplace violence also showed that 42.5% of participants reported experiencing non-physical workplace violence with one of the most common forms being sexual harassment [3].
Patients are one of the most common sources of sexual harassment with common forms being inappropriate comments about appearance, capabilities, or the patient’s relationship to the healthcare provider [4]. Medical students are taught skills to interact with patients early in their training. Many schools have students learn clinical and interprofessional skills with standardized patient actors, such as delivering bad news and working with an interpreter. Students are also often taught how to deal with sexual harassment in the workplace, as such coming from their peers and colleagues. However, medical schools commonly do not address patient initiated sexual harassment. And in the event such probabilities are addressed, students report that they are not given practical strategies to respond or report [4].
Previous models of responding to patient initiated sexual harassment progressed from focusing on reporting the issue to responding to it in real time. To our knowledge, there are three models in MedEdPORTAL [5,6]. The ERASE model published in 2019 teaches the fact that mistreatment from patients will occur and that all learners should be involved in the decision-making process for the next step [6]. This model focuses on the role of the supervising physician rather than practical strategies for responding for the learners themselves. The Stop, Talk, and Roll method published in 2020 focuses on strategies that students can use to remove themselves from a hostile situation and report to a supervisor [5].
It also encourages students to actively learn how to diffuse such situations by observing their supervisors. While this model provides students with guidelines both on how to protect themselves and how to seek counsel from a supervisor, it does not educate students on practical responses to address the issue with patients directly. The Tools for Responding to Patient Initiated Sexual Harassment published in 2021 provides strategies for all healthcare providers to respond to patients in real time [4]. This method utilizes “I” statements and clear separation of intent from content to help educate patients on proper physician-patient communication. The 4R workshop also focuses on direct forms of communication to address patient behavior.
Unlike the Tools for Responding to Patient Initiated Sexual Harassment workshop, this workshop goes one step further to emphasize the importance of emotional processing and checking in with self and others after such encounters.
The medical student workshop and 4R method was created to emphasize the need for pre-clinical student training in responding to patient initiated sexual harassment (PISH). Like previous models, this method focuses on the usage of “I” statements and separation of harasser and comment to address patient behavior. The 4R method also focuses on students’ emotional responses during and after the encounter. This workshop moves away from the previously used role playing and small group activity format and towards a standardized patient format. Previous studies have shown that learning communication and patient management skills by standardized patients to be significantly more effective than conventional academic training and small group seminars [7,8]. Furthermore, usage of standardized patients allows for students to have a better understanding of their natural emotional response to PISH. Like earlier models, the 4R Method workshop utilizes scripted responses to help patients better understand the role of trainees in the healthcare team [4,9]. The workshop also emphasizes the importance of bystander intervention [4,6] but addressed the need for bystanders to check back in with the learner after a short period of time to allow for emotional processing. After participating in the workshop, all learners will have developed a step-by- step process for responding in real time, reporting the issue, and reflecting on the encounter.
Methods
This workshop aimed at teaching medical students’ strategies for responding to patients and reporting the encounter, however the methods can be applicable to any healthcare worker. This medical student authored method and workshop emerged after the principal author experienced multiple encounters of PISH while in medical school. Upon conferring with peers and other healthcare personnel, it was evident that this was a common occurrence and that most peers did not know how to or when they should respond. We reviewed the existing institution curriculum and found sparse education on practical methods to respond to PISH. Study of existing models provided ample methods of responding and reporting, however failed to address different levels of comfort in responding to PISH as well as the need for emotional processing after an encounter. The method draws.
upon previous models [4,5] for methods to respond during an encounter. Furthermore, it is inspired by the ERASE model method6 for bystander intervention strategies. The 4R Method consists of the four actions that must be taken by learners in the event of experiencing or witnessing PISH. The actions are detailed below:
A. Respond to the act
a) Use “I” statements when correcting a patient’s behavior.
b) Separate the intent from the action.
c) Emphasize that focusing on the patient’s needs and remaining professional is in the patient’s best interest.
d) Respond according to your comfort level (with two variations of responses detailed based on comfort level)
e) Pay attention to tone and body language to empower and protect yourself while responding.
B. Report the act
a) Report to the next level of authority along the hierarchy of the medical institution. If not given the appropriate resources or support, move up the chain of command.
b) Always report an encounter. It will help the institution protect its students from any action taken by the patient or their family. And it will also help remove learners from potentially toxic learning situations.
C. Reflect on the act
a) Take time to understand the encounter and any emotional responses.
b) Know that it is never the learner’s fault.
c) Ask for help when needed! Be willing to use the mental health resources provided by the school.
D. React when witnessing the act
a) Check in with my colleague.
b) Reassure them that you support them in all their actions and can help.
c) Check in again after a short period of time so that they can process the encounter.
The ideal workshop facilitators would include a panel that consists of a medical student currently in clinical rotations or a resident physician, a member of student affairs administration, and a representative of the school’s mental health and counseling service team. The format of the workshop consists of two parts: (1) a standardized patient encounter during which students experience PISH and (2) a post encounter discussion panel detailing the 4R method and highlighting each institution’s available resources.
Timeline of the workshop is as detailed: (total time of 2 hours):
A. 1 hour: standardized patient encounter
a) 15 minute per encounter
B. 1 hour: workshop discussion panel
a) 5 min: introduction, ground rules, and learning objectives.
b) 10 min: background and research
c) 5 min: reaction to PISH and issues with current training
d) 5 min: ERASE model
e) 5 min: Stop, Talk, and Roll model.
f) 10 min: Iowa Toolkit model
g) 15 min: 4R model
h) 5 min: closing, post workshop survey completion
Contents of the sessions are contained in the appendices with Appendix A being the facilitator’s guide. At the beginning of the workshop, students were told about the structure of the workshop and as well as the purpose of the session. Students were informed that they are to undergo a patient encounter where they will experience some unwanted interactions, however they were not told any other specifics to preserve the authenticity of their reactions. In the effort to create an environment where students can experience a common form of PISH without being emotionally triggered, the encounter entailed learners obtaining a blood pressure check from the patient
Learners were told that they are “very pretty/ handsome,” at the start of the encounter as well as that their “touch feels really good,” while obtaining the blood pressure (as entailed in Appendix E). Students were also informed before their encounter that they are allowed to tell the standardized patient they do not want to proceed with the encounter at any point during the session and will be provided with a video of the same scenario. This option was designed in a way so that students with previous traumas do not have to relive them while not having to reveal this information to their classmates.
Upon completion of the patient encounters, the workshop discussion began with ground rules intended to keep the workshop a safe space. Facilitators highlighted real examples of PISH that have occurred to them and encouraged students to speak with them privately if needed. The lecture was guided by PowerPoint slides (Appendix B) and started with definitions of terms used as well as supporting research about PISH in the medical field.
Students were then asked to reenact a sample scenario that modeled the patient encounter that they had completed. They were then asked to volunteer information about how they naturally responded and how they felt in that moment. Facilitators reviewed the most common reactions as well as some safety guidelines that should always be considered.
Next, facilitators reviewed the existing models of dealing with clinical place harassment. Afterwards, students were taught the 4R method during which practical strategies as well as coping mechanisms were discussed. At this point, the institution’s resources were highlighted, and all members of the panel contributed their expertise. Finally, facilitators wrapped up the second portion of the workshop by reiterating take home points as well as the 4R method actions. At the end, students were asked to fill out a post-workshop survey.
We delivered the workshop over three sessions (each session lasting 2 hours in length) at an academic medical center in May 2022. Sessions were attended by first year medical students and served as one of their patients- based learning activities. The sessions were led by author of the 4R method (who was a fourth-year medical student at the time).
Finally, to evaluate the workshop, students filled out a post workshop survey with a Likert style questionnaire (for ex. 5 = excellent, 1 = terrible). The survey included questions about the quality of the workshop, value of the lessons taught, and realism of the scenario (Appendix C). Students also answered qualitative questions about their experience as studies have shown such open-ended questions allow for researchers to gain context to participants’ answers and perspectives [10].
Results
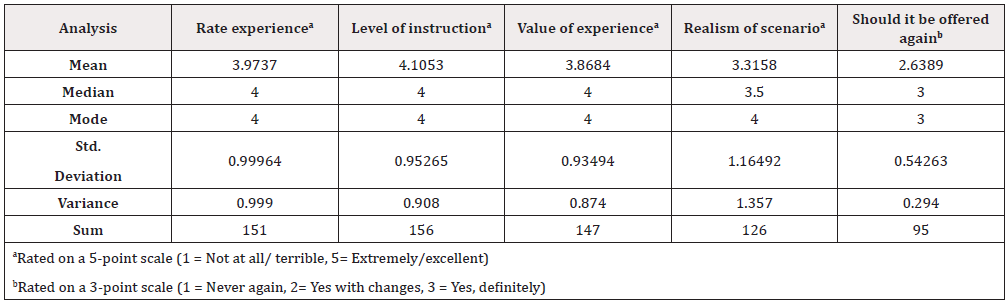
A total of 201 pre-clinical students participated in the workshop, however only 38 students filled out the voluntary post workshop survey. The low survey completion rate limited the scope for statistical analysis. In general, students had a better than average opinion about various aspects of the workshop. The experience was rated close towards the “Good” mark (mean = 3.97) as were the level of instruction (mean = 4.11) and value of the experience (mean = 3.87). The question of “How realistic was the scenario?” was marked closer to average (mean = 3.32) while most students answered that the workshop should either be offered again or be offered again after making changes (mean = 2.64) (Table 1).
Qualitative feedback from students was mixed but overall positive. Responses to the question regarding the part that students enjoyed most focused on the practical responses given during the lecture. Responses to the two remaining questions (what could be improved and what else participants would like to share) focused on the changes that could be made to the patient encounter. While students found it useful, they were not sure if the scenario chosen was the most apt or impactful for the lesson. Multiple responses also focused on the fact that the patient encounter would be more useful after the lecture or should be taken out entirely as they felt it to be triggering.
Discussion
The 4R method worked to educate pre-clinical students by raising awareness of PISH and by providing skills to respond. It emphasized the lessons introduced by earlier methods and expanded on the importance of tone and body language, comfortability in responding, and the need for emotional processing. The 2-hour workshop was initially geared towards pre-clinical medical students but can be used for any healthcare student or personnel.
Overall, the workshop was received well by the inaugural class at the medical institution. However, reviews by students and standardized patients brought attention to areas that could be improved for future workshops. First, some students noted that it would be more useful to have standardized patient interaction at the end to have practice after learning techniques for responding. They stated that understanding their natural reaction was not necessary as most students have already experienced harassment. Furthermore, standardized patient actors noted that while the provided script was designed in a way as to not trigger any students, it did little to accurately display the degree of sexual harassment experienced in the clinical field. The actors stated that it was difficult to simulate an accurate scenario when they were not able to go off the script. While moving the standardized patient encounter to the end of the workshop is an easy solution, the issue of the prompts is harder to navigate.
The examples of harassment in the prompts cannot be so intense as to cause students any emotional or mental distress. Moreover, students cannot feel as though they have been sexually harassed during the workshop therefore limiting the examples of sexual harassment that can be used. This can be addressed, however, by allowing the standardized patients to respond as they see fit during future workshops and by warning students ahead of time about the full premise of the patient encounter as well as their options to opt out. Those who wish to continue with the activity will be able to practice their skills and those who do not wish to participate can tell the standardized patients upon entering the room. This will allow for the standardized patient actors to simulate a real scenario to the best of their ability while protecting students from resurfacing traumas.
There were several limitations to the study. The workshop was presented to one class of pre-clinical students at the academic medical institution and therefore requires repeat and trial with more participant pools. Furthermore, we were not able to measure the students’ change in response to PISH after the lecture portion of the workshop.
as compared to their initial patient encounter. Finally, we were not able to ascertain the participants’ capabilities and knowledge after a period of time and while in clinical settings. This was because the surveys were conducted right after the workshop session and because the students were not set to enter the clinical field for another year.
Future workshop sessions are needed to further evaluate the 4R method and its usefulness in the clinical setting. These sessions will aim to incorporate standardized patient encounters before and after the lecture to fully evaluate the impact of the lecture as well as to give students a chance to practice the skills that they have learnt. Workshop facilitators should also aim to send surveys to participants after a short period of time to measure the knowledge retention after the workshop period. Students in future workshops should also receive a 4R method handout to serve as reference material when needed (Appendix D). Sharing this method and workshop with other medical institutions will allow study of the relevance and effectiveness of the 4R method on a broader scope.
Finally, future workshops can also adapt this work to be applicable to other healthcare fields.
We hope that the 4R method not only builds upon the lessons and strategies taught by past methods, but also addresses barriers to responding to and processing PISH encounters in the clinical field. While more workshop sessions will allow for the method to be adjusted as needed, we sincerely believe that our training guide will be useful to educators and medical institution administrators looking to educate their students and employees about patient-initiated mistreatment.
Conflict of Interest
None.
References
- McKinley SK, Wang LJ, Gartland RM, Westfal ML, Costantino CL, et al. (2019) "Yes, I'm the Doctor": One Department's Approach to Assessing and Addressing Gender-Based Discrimination in the Modern Medical Training Era. Acad med 94(11): 1691-1698.
- Ph Phillips SP, Webber J, Imbeau S, Quaife T, Hagan D, et al. (2019) Sexual Harassment of Canadian Medical Students: A National Survey. EClinicalMedicine 7: 15-20.
- Liu J, Gan Y, Jiang H, Li L, Dwyer R, et al. (2019) Prevalence of workplace violence against healthcare workers: a systematic review and meta-analysis. Occup environ med 76(12): 927- 937.
- Hock LE, Barlow PB, Scruggs BA, Oetting TA, Martinez DA, et al. (2021) Tools for Responding to Patient-Initiated Verbal Sexual Harassment: A Workshop for Trainees and Faculty. MedEdPORTAL 17: 11096.
- San Sandoval RS, Afolabi T, Said J, Dunleavy S, Chatterjee A, et al. (2020) Building a Tool Kit for Medical and Dental Students: Addressing Microaggressions and Discrimination on the Wards. MedEdPORTAL 16: 10893.
- Wilkins KM, Goldenberg MN, Cyrus KD (2019) ERASE-ing Patient Mistreatment of Trainees: Faculty Workshop. MedEdPORTAL 15: 10865.
- Reger GM, Norr AM, Rizzo AS, Sylvers P, Peltan J, et al. (2020) Virtual Standardized Patients vs Academic Training for Learning Motivational Interviewing Skills in the US Department of Veterans Affairs and the US Military: A Randomized Trial. JAMA Netw Open 3(10): e2017348.
- Herbstreit F, Merse S, Schnell R, Noack M, Dirkmann D, et al. (2017) Impact of standardized patients on the training of medical students to manage emergencies. Medicine 96(5): e5933.
- Bryan AF, Bryan DS, Matthews JB, Roggin KK (2020) Toward Autonomy and Conditional Independence: A Standardized Script Improves Patient Acceptance of Surgical Trainee Roles. J Surg Educ 77(3): 534-539.
- Cleland JA (2017) The qualitative orientation in medical education research. Korean J Med Educ 29(2): 61-71.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.