Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
A-45-Years-Old Woman with Solitary Pulmonary Nodule and Rib Erosion Due to Hemangioma: History is Always Crucial!
*Corresponding author: Khin Phyu Pyar, Professor and Head/Senior Consultant Physician, Department of Medicine/ Department of Nephrology, Defence Services Medical Academy, No. (1) Defence Services General Hospital (1000-Bedded), Yangon, Myanmar.
Received: January 05, 2024; Published: January 12, 2024
DOI: 10.34297/AJBSR.2024.21.002810
Summary
A solitary pulmonary nodule with rib erosion underneath is malignant until proved otherwise. The patient was 45years old nonsmoker presented with cough off and on for 3years. Chest radiograph and CT scan revealed a mass in right upper chest with erosion of the 4th rib. She underwent resection of tumor including 4th rib; the histology was compatible with haemangioma of the rib. She had history of a small nodular lesion over dorsum of her left hand for two years; and the excisional biopsy revealed haemangioma.
Keywords: Solitary pulmonary nodule, Rib erosion, Haemangioma
Opinion
A Solitary Pulmonary Nodule (SPN) is defined as a round or oval opacity smaller than 3cm in diameter that is completely surrounded by pulmonary parenchyma with no other pulmonary abnormalities present. On the other hand, pulmonary lesions with a diameter larger than 3cm are classified as pulmonary masses; they have a higher possibility of being malignant. Five percent of SPN were bronchogenic carcinoma particularly it was situated in upper lobe [1]. SPN is an uncommon finding in chest radiograph; it is seen in 0.1-0.2% of chest imaging [2]. Being a several diagnostic dilemma on SPN, it requires MRI, PECT scan, biopsy and PCR studies in addition to CT scan and bronchoscopy [3]. The etiology of SPN may be benign or malignant. Rib erosion favors neurogenic tumor [4]. Differentials for benign lesions include carcinoid, sarcoidosis, amyloid, hamartomas, infections (TB and non-TB mycobacteria), round atelectasis, granulomatosis with polyangiitis, rheumatoid arthritis, vasculitis, arteriovenous malformations, cyst, harmatoma, neurofibroma and intrapulmonary lymph nodes [1]. Malignant tumors may arise from lung or non-pulmonary origin; it may be secondary metastasis [5-9].
Haemangioma is a benign vascular tumor. It is usually slow growing in nature. It may be asymptomatic and is detected as a mass lesion in chest radiograph. Approximately 25% of people with hemangioma present in persons in the fifth decade of life. The organ commonly involved are skin, liver, eye and central nervous system; it typically arises in the subcutis of the distal extremities of young people [10]. However, it can involve skeleton system especially in flat bone like skull bone and vertebral body; and it rarely affects the ribs.
Pulmonary hemangiomas have a broad range of clinical presentations depending on the location, size and number of lesions. Pulmonary lesion may present as respiratory symptoms, pressure symptoms, hemoptysis, hemothorax due to rupture into pleural cavity [11,12]. Involvement of both lungs was seen; it presented as multiple nodule in lung [11,13,14]. Rarely it mimicked metastasis as nodular lesions in both lungs and liver [15].
Case Report
A 45-years- old woman had cough with mucoid expectoration off and on for 3years. Physical examination revealed occasional crackles over right lung. She had mild pallor; cushingoid face; blood pressure 140/90mmHg; heart rate 60/min; no lump in both breast; no lymphadenopathy; and, no organomegaly. She was lifelong non-smoker. She was a known case of SLE since 22years of age. She had generalized oedema as initial symptom and renal biopsy was reported as endocapillary proliferative glomerulonephritis. She was on methyl prednisolone 16mg three times a week and mycophenolate mofetil. She also had hypertension for 5years and controlled well with losartan 50mg OD, aldectone 25mg OD. Her home blood pressure was 130/90mmHg. She was taking eltroxin 25ug a day as she also had hypothyroid (autoimmune). The patient has been practicing as anesthetist in ICU and operating theatre for 20years.
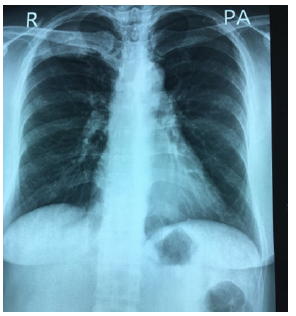
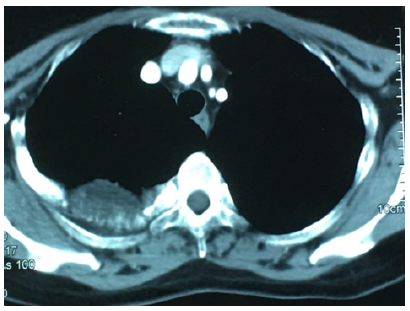
Urine examination was normal. LE cell was negative, Extractable nuclear antigen profile was negative. Serum creatinine and blood urea were normal. Ultrasound abdomen was normal. Chest radiograph showed an ill- defined mass, 3cm in largest diameter at right apical area with erosion of the 4th rib. It is shown in Figure 1. It became larger over 1year as demonstrated in Figure 2. CT scan chest revealed a mass at posteromedial site with the 4th rib erosion Figures 3,4. The other investigations were as follows: hemoglobin 12g%; total WBC count 6.2X109/L; platelets normal. Liver function tests were normal. Lung function test showed normal FEV1; normal FEV1 and FVC ratio. The cholesterol was raised. Her blood group was B Rh negative (Figure 1-4).
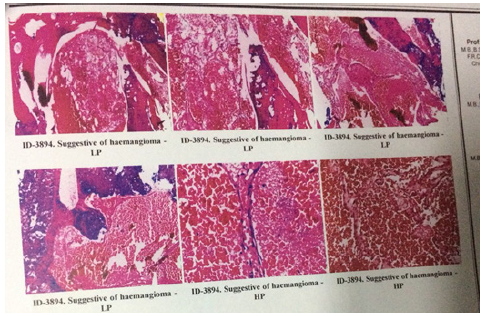
She underwent thoracotomy and rib resection. She had hypotension during surgery and it responded well to steroids and blood transfusion. The post-operative period was uneventful. Histology revealed hemangioma as seen in Figure 5. When the histological result came, the patient said there was a small nodular lesion over dorsum of her left hand which she noticed for two years. The clinical impression was ganglion or implantation dermoid cyst. The excisional biopsy done 3 years ago revealed hemangioma. Figure 6 indicates the site of lesion at left hand (Figures 5,6).
Discussion
Because of high etiological diversity and the potential for malignancy, SPN represent a clinical challenge. Moreover, the prevalence SPN is increasing because of advancement in CT scan. Nearly 5% of incidental SPNs are malignant; and they tend to be located in the upper lobes [1]. Although she is a life-long nonsmoker, the possibility of bronchogenic carcinoma was considered owing to association with rib erosion. Common differential diagnosis on SPN were tuberculous granulomas, vasculitis, lung cancers and hamartomas [1,16]. Although she is a life- long nonsmoker, the possibility of bronchogenic carcinoma was considered owing to association with rib erosion. There were several case series on SPN; nevertheless, none of them had rib erosion [17]. This is one reason for case reporting.
Another possibility of SPN in this case may be due to autoimmune related nodule caused by granulomatosis with polyangiitis, rheumatoid arthritis, vasculitis and SLE. Pulmonary manifestation of SLE is seen in 40-70% of cases, mainly pleural involvement. It may give rise to pulmonary fibrosis and bronchiolitis obliterans. Pulmonary vein vasculitis seen as multiple pulmonary nodule was reported [16]. The most common HRCT findings in SLE were ground glass opacity, interlobular septal thickening, bilateral diffuse infiltrates, and pleurisy/pleural effusion [18]. The likely hood of auto-immune related nodule was also considered in this case because she was known case of SLE. Having negative ENA profile, absence of vasculitis in skin and quiescent renal involvement pointed out less possibility of SLE related nodule.
Furthermore, the possibility of granuloma due to Mycobacterium tuberculosis was also discussed as the patient was immunocompromised state: SLE itself; steroids therapy; and mycophenolate mofetil therapy. Therefore, second differential diagnosis was tuberculous consolidation with underlying tuberculous osteitis of rib. The favorable points for tuberculous granuloma were her occupational exposure as a doctor in Myanmar, high tuberculosis burden country, and immunocompromised state. Sputum for acid fast bacilli was negative. IGRA test was negative. CT chest did not show features of tuberculosis like tree in bud opacities, cavitary lesions with a thick wall, and central hypoenhancing necrotic nodules. In addition, the histology of nodule ruled out tuberculosis.
This patient had SPN with rib erosion. The cause of rib erosion in chest radiograph is malignancy until proved otherwise. Yeom et al suggested that rib erosion favored neurogenic tumor [4]. It was emotionally burdensome for this patient being a doctor- clinician. Although the patient did not have risk factors for bronchial carcinoma, pre-operative diagnosis was malignancy. Therefore, she underwent thoracotomy and excision. Histology was compatible with hemangioma. Benign SPN with rib erosion was never reported before. This is main reason for case reporting.
Haemangioma is a benign vascular tumor; it rarely affects the ribs. This patient had erosion in 4th rib. This is another reason for writing this case. Majority of the patients with hemangioma presented with solitary lung nodule, while 5 patients showed multifocal lesions [19]. One study evaluated the CT and PET-CT features of Solitary Pulmonary Capillary Hemangioma (SPCH) with clinicopathologic correlations. And, they found that SPCH was often incidentally detected in young and middle-aged adults, commonly as an ill-defined part-solid nodule with air bronchogram, perivascular lucency, and fluctuation in size or density on CT and hypometabolism on PET-CT [20,21]. In this case, SPN was situated at right apex; posteromedial lesion. Haseli et al discussed the role of imaging and its strengths and limitations for diagnosing posteromedial chest wall lesions [22].
In this case, the gross inspection of resected rib and mass was soft and not fleshy; thus, it was unlikely to be malignancy. The cross section did not reveal cheesy materials; therefore, it was not tuberculosis. Figure 7 shows cut section. Histology was reported as haemangioma. When the histological result came, the patient said there was a small nodular lesion over dorsum of her left hand which she noticed for two years. The pre-operative impression was ganglion or implantation dermoid cyst. The excision biopsy done 3 years ago revealed haemangioma. Therefore, history is the key in medicine; all the events are always related. The site of lesion on hand was typical site for hemangioma; Duqing pointed out that hemangioma typically arises in the subcutis of the distal extremities of young people [10] (Figure 7).
There was extremely rare report on multiple haemangioma involving both skin and of the internal organs. Combined pulmonary and other organ involvement was mentioned by Diaz Churion [23]; bilateral lung involvement was reported by He [11]. Lung involvement with vascular malformation over calf was seen by Soumil [24]. Review on 44 cases of hemangioma over several decades revealed that only 20% of them had accurate pre-op diagnosis [25]. Therefore, this case rare form.
Conclusion
Pulmonary haemangioma is a very rare cause of a solitary pulmonary nodule with rib erosion. Clinicians should consider multi system involvement if one has haemangioma. History is everything.
Ethical Approval
Our institution does not require ethical approval for reporting cases.
Funding
The authors received no financial support for publication of this article.
Informed Consent
The informed consent for publication in this article was obtained from patient.
Acknowledgements
The authors would like to thank the patient and family for giving consent to this article. Also, to all doctors and nursing team for making great efforts in caring her. The authors acknowledged the following teams: Professor Mg Mg Khin for thoracic surgery, Professor Yu Aye Latt for anaesthesia and the intensive care, Professor Thet Naing, Professor Myint Zaw, Professor Kyaw Zay Ya and Professor Ko Ko Lwin for administrative support.
Declaration of Conflict of Interest
The authors declared no potential conflicts of interests with respect to authorship and publication of this article.
References
- Harzheim D, Eberhardt R, Hoffmann H, Herth FJF (2015) The Solitary Pulmonary Nodule. Respiration 90(2): 160-172.
- Patro M, Gothi D, Sah RB, Vaidya S (2018) An interesting case of incidental solitary pulmonary nodule. Breathe 14(4): e128-e133.
- Masuta P, Amzuta I (2019) Solitary Pulmonary Nodule: A Diagnostic Dilemma. Case Rep Pulmonol 2019: 5242634.
- Yeom YK, Kim MY, Lee HJ, Kim SS (2015) Solitary Fibrous Tumors of the Pleura of the Thorax: CT and FDG PET Characteristics in a Tertiary Referral Center. Medicine 94(38): e1548.
- Xu CH, Zhan P, Yu LK (2013) Solitary pulmonary nodule-a case of peripheral adenocarcinoma with rapid metastasis 5(6): 847-850.
- Yuan D, Zhang JY, Yao YW, Sun HM, Wu GN, et al. (2017) The pulmonary nodule “discovered” by pneumonia: A case report. Transl Lung Cancer Res 6(1): 92-96.
- Tsaknis G, Naeem M, Singh A, Vijayakumar S (2021) Malignant melanoma without primary, presenting as solitary pulmonary nodule: A case report. J Med Case Rep 15(1): 347.
- C S Sivasubramaniamurthy, D M kumar, A S Murthy, S Parijatham, G Jayalakshmi, et al. (1983) SOLITARY PULMONARY NODULE (A CASE REPORT). Lung India 1(4): 155-157.
- Kosaka T, Iizuka S, Yoneda T, Otsuki Y, Nakamura T (2022) Solitary pulmonary nodule as the initial manifestation of isolated metastasis from prostate cancer without bone involvement: A case report. Int J Surg Case Rep 90: 106681.
- Duqing X, Zhaohong W, Gefei W (2019) Multiple spindle cell hemangiomas in both lungs: A rare case report and review of the literature. J Cardiothorac Surg 14(1): 86.
- He C, Fang H, Liu Y, Huang X, Zhen W, et al. (2012) Pulmonary sclerosing hemangioma: Report of two cases. World J Surg Oncol 10(1): 182.
- Huang T, Pope SJ, Volpe JP, Shah RP, Fiel Gan MD (2017) Pulmonary capillary hemangioma diagnosed by needle core biopsy: Case report and review of the literature. Human Pathology: Case Reports 9: 50-54.
- Hagui E, Sakane T, Hioki K, Nakano T, Haneda H (2023) A case of resected pulmonary capillary hemangioma with a literature review. Respirol Case Rep 11(5): e01138.
- Chen Q, Li H, Hu B, Jin M, Guo J (2014) Multiple Cavernous Hemangiomas of the Lung. Ann Thorac Surg 98(5): 1835-1837.
- Zhuang B, Li W, Chen Z, Cao C, Xie X, et al. (2018) Multiple cavernous hemangiomas of the lung and liver mimicking metastasis: A case report and literature review. Medicine 97(51): e13509.
- Hiroya Tamai, Naoshi Nishina, Tsutomu Takeuchi (2019) Pulmonary Vein Vasculitis Presenting as Multiple Pulmonary Nodules in a Patient with Systemic Lupus Erythematosus. J Rheumatol 46(3): 323-324.
- Gulbanu Horzum Ekinci, Osman Haciomeroglu, Ayse Ersev, Levent Alpay, Ayçim Sen, et al. (2015) Sclerosing hemangioma of the lung: An analysis of 8 cases. European Respiratory Journal 46(suppl 59): PA4303.
- Dai W, Gu H, Hao S (2020) Potential benefits, mechanisms, and uncertainties of convalescent plasma therapy for COVID-19. Blood Sci 2(3): 71-75.
- Luo H, Ma L, Chen Y, Zhang T, Peng D, et al. (2020) Multiple sclerosing hemangioma of the right lung in a 23‑year‑old female patient: A case report and review of the literature. Mol Clin Oncol 12(3): 263-
- Kim MJ, Hong W, Kim TJ, Han J, Choi YL, et al. (2022) Solitary Pulmonary Capillary Hemangioma: CT and PET-CT Features with Clinicopathologic Correlation. Diagnostics (Basel, Switzerland) 12(11): 2618.
- Mansour J, Raptis D, Bhalla S, Heeger AP, Abbott GF, et al. (2022) Diagnostic and Imaging Approaches to Chest Wall Lesions. Radiographics 42(2): 359-378.
- Haseli S, Mansoori B, Shafiei M, Shomal Zadeh F, Chalian H, et al. (2022) A Review of Posteromedial Lesions of the Chest Wall: What Should a Chest Radiologist Know? Diagnostics (Basel) 12(2): 301.
- Diaz Churion F, Walsh KL, Yu Lee Mateus A, Sriram A, Abia Trujillo D, et al. (2023) Multiple Capillary Hemangiomas of the Lung with Multi-Organ Involvement. Respiration 102(6): 463-464.
- Soumil VJ, Navin B, Sangeeta D, Na J, Sharma S, et al. (2004) Multiple Sclerosing Hemangiomas of the Lung. Asian Cardiovasc Thorac Ann 12(4): 357-359.
- Kuo KT, Hsu WH, Wu YC, Huang MH, Li WY (2003) Sclerosing hemangioma of the lung: An analysis of 44 cases. J Chin Med Assoc 66(1): 33-38.






 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.