Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
A Case of Mammary Schwannoma Originated from the Pectoral Muscle Nerve
*Corresponding author:Natsuko Mizutani, Department of Medical technology Kyorin University School of Health Sciences. Department of Immunological diagnosis, Juntendo University Graduate School of Medicine.
Received: February 06, 2024; Published: February 13, 2024
DOI: 10.34297/AJBSR.2024.21.002859
Summary
Introduction
Schwannoma, also called neurilemmoma, neurinoma, a kind of slow-growing benign neoplasm [1-3]. Schwannoma has a predilection for the head, neck, and extensor surfaces of the upper and lower extremities [4]. They can arise from Schwann cells of any nerve in any organ. However, 2.6% of schwannomas occur in the breast. Schwannoma is a clearly bordered painful tumor and rarely arises within breast parenchyma. Fibroadenoma is a common benign breast tumor with also clearly bordered image. We experienced a case of schwannoma originating from the pectoral muscle nerve, and it was difficult to distinguish preoperatively from a fibroadenoma of breast.
Case Presentation
A 58-year-old woman complained right breast pain. We palpated a tumor in the right breast of the upper outer quadrant, 2cm in diameter, oval shape and elastic soft in texture. The US showed a mass, oval and smooth, clearly bordered, suggesting a fibroadenoma (Figure 1).
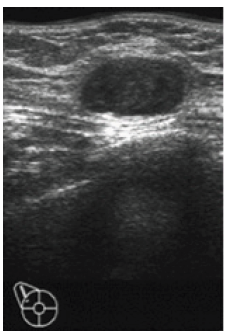
Figure 1: Assessment of the effect of emergency radiation therapy on patients, an effect on overall survival (OS).
Note*: Oval and smooth, clearly bordered, suggesting a fibroadenoma.
FNAC (Fine Needle Aspiration Cytology) expressive fatty cells and fibrous cells as well as stromal cells, with unconfirmed ductal cells (Figure 2). We reported ‘inadequate specimen’.
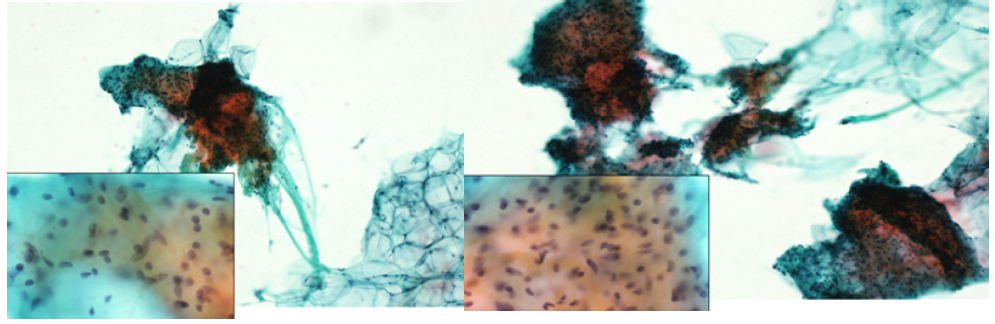
Figure 2: Assessment of the effect of emergency radiation therapy on patients, an effect on overall survival (OS).
Note*: There are fatty cells and fibrous cells as well as stromal cells. No ductal cells were found in the specimens.
MMG showed a mass, regular and oval shaped, on the edge of the breast (Figure 3).
The tumor extirpated to confirm the histology of breast tumor. The tumor was easily exfoliated from the greater pectoral muscle under the mammary glands. The tumor, measuring 2.9×2.4×1.6cm in size, appeared to be covered by a capsule, and yellowish in color. The pathological examination revealed tumor cells were spindled in shape and had oval or elliptical nuclei. The tumor showed nuclear palisading (Antoni A) and pluricellular areas (Antoni B) in part (Figure 4).
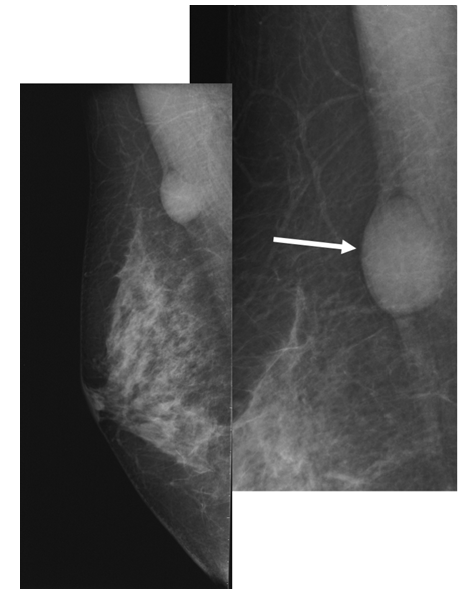
Figure 3: Assessment of the effect of emergency radiation therapy on patients, an effect on overall survival (OS).
Note*: A shaped and round mass was observed on the edge of the breast.
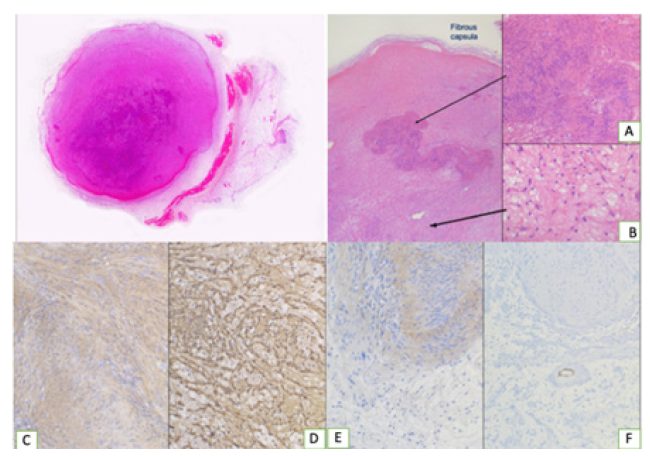
Figure 4: Assessment of the effect of emergency radiation therapy on patients, an effect on overall survival (OS).
Note*: Tumor size, 2.9x2.4x1.6 cm.
Re-examination of MMG indicated a schwannoma originated from the pectoral muscle nerve. Retrospectively, the findings of FNAC specimen were not in contradiction in a schwannoma of Antoni B, although we could not confirm the findings of Antoni A. The mammary schwannoma should be considered in the cytological diagnosis of a patient with a painful tumor with clear borders.
Discussion
Schwannomas are derived from Schwann cells that form the myelin sheath of nerves, which facilitates the transmission of an impulse.[5] A schwannoma is a slow growing tumor that develops in the peripheral nerves or spinal roots [5]. Any part of the body can be affected but intramammary localization is rare. Breast schwannomas account for only 2.6% of all schwannomas, with an incidence of 0.2% of all breast cancer cases [1,2]. Pathologically, schwannomas have 2 components, known as Antoni A tissue and B tissue, in variable proportions, and these spindle cells show nuclear palisading and parallel arrays are known as Vero cay bodies [5]. In addition, schwannomas express S-100 protein on immunochemistry findings. Similarly, on cytological diagnosis of the present schwannoma case, the spindle cell was a vague palisading pattern that resembled a Vero cay body and S-100 was positive.
Clinically, a breast schwannoma is considered that has a very low risk of malignant transformation [6]. Therefore, core-needle biopsy should be performed for pathological diagnosis and for the purpose of treatment because of the recurrent nature of the breast tumor. By the way what about preoperative FNAC. Table 1 shows the classification used in Japan (Table 1). The classification is based on the Bethesda system for cellular diagnoway,. If we had followed this system faithfully, the epithelial component was not collected in this case, and the specimen would have been deemed inadequate. However, instead of no epithelial component, a strangely large amount of mesenchymal cellular component was collected. In retrospect, this should have been the focus of attention. The high stromal component of the stroma also differentiates it from fibroadenoma but note that the cellular morphology differs from the stroma of fibroadenoma.
Breast schwannoma is a peripheral nerve sheath tumor in these nerves. Goose, et al. [7] reported that only 5/99 (5%) patients with benign schwannomas experienced pain at rest. In contrast, 94/99 (95%) patients with benign peripheral nerve sheath tumor had pain induced by pressure.
In conclusion, we report a case of breast schwannoma, which is a rare tumor and its characteristics. This neoplasm is very difficult to differentiate due to its morphological features and location. It is important to recognize this tumor based on physical examination and imaging findings. And after the image test, cytologic and pathologic findings should always confirm the type of tumor. Furthermore, even if no epithelial component is seen in FNAC it is necessary to focus on other cellular components that are frequently sampled.
Conflict of Interest
None.
Acknowledgement
None.
References
- TN Ravelomihary, NM Razafimanjato, L Nomenjanahary, AF Rakototiana, HJ Rakotovao, et al. (2019) Schwannoma of the breast: a report of rare location and a brief literature review. Ann Breast Surg 3(0): 17.
- Uchida N, Yokoo H, Kuwano H (2005) Schwannoma of the breast: report of a case. Surg Today 35: 238-242.
- QT Tan, EWL Chuwa, SHChew, GS Hong (2014) Schwannoma: an unexpected diagnosis from a breast lump. J Surg Case Rep (9): rju085.
- V Dialani, N Hines, Y Wang, P Slanetz (2011) Breast schwannoma. Case Rep.
- Dabbs DJ (2016) Breast Pathology E-Book. Elsevier Health Sciences 31: 663-717.
- Nayler S, Leiman G, Omar T, Cooper K (1996) Malignant transformation in a schwannoma. Histopathology 29: 189-192.
- Ogose A, Hotta T, Morita T, S Yamamura, N Hosaka, et al. (1999) Tumors of peripheral nerves: correlation of symptoms, clinical signs, imaging features, and histologic diagnosis. Skeletal Radiol 28(4): 183-188.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.