Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
A Rare Recurrence of Cervical Cancer to the Sigmoid Colon: A Case Report
*Corresponding author:Zafar S, Ontario Institute for Studies in Education, University of Toronto, Canada.
Received: February 21, 2024; Published: March 04, 2024
DOI: 10.34297/AJBSR.2024.21.002884
Introduction
There are estimated 604,127 new cases and 341,831 deaths in 2020 [1], accounting for a large proportion of cancer deaths worldwide [2,3]. Primary colorectal SCC is rare. Squamous carcinoma of cervical carcinoma is the second most common cancer in women worldwide. Early-stage cervical cancer can be potentially cured with radical hysterectomy or chemoradiation therapy. Approximately 30% of patients treated for cervical cancer will have tumor recurrence, most commonly in the first 2 years after treatment. Direct local extension and lymphatic dissemination are the main ways of metastasis. The lung and paraaortic nodes are the most prevalent sites of distant metastases [4]. The brain, skin, spleen, muscle and gastrointestinal tract are rare sites that have only been described in a few cases. Lymphonodal status, parametrial and surgical margin involvement, tumor size or deep stromal invasion significantly affect recurrence rate while histological type and grade of the cervical lesion reportedly do not [5-6]. We report a case of isolated recurrent cervical cancer in the sigmoid colon arising 9 months after primary surgical therapy and treated by en mass resection of left sided rectus muscle resection, urinary bladder wall, sigmoid colon, skin subcutaneous tissue to achieve R0.
Case Presentation
We report a 43-year-old woman admitted to our hospital with a complaint of vaginal spotting in between mensus 1 year back. On gynecological physical examination she was found to have a cervical mass which was bleeding on touch. Liquid based cytology was done and showed atypical glandular (endocervical) cells. A high vaginal swab biopsy was taken and showed squamous epithelium with features of CIN-3 and an invasive tumor showing squamous cells. Immunohistochemistry with p16 confirms the subtype as HPV associated. She underwent MRI pelvis which was consistent with cervical cancer invading the upper third of vagina (Stage II FIGO classification) and a PETCT scan revealed FDG avid soft tissue mass lesion in the cervix, consistent of malignant pathology. Cervical biopsy was taken and histological features were consistent with squamous cell carcinoma of cervix, HPV associated. Histological grade of lesion is Grade 3–Poorly differentiated. The patient was planned for upfront surgery and undergone radical hysterectomy, salpingo-ovariectomy, bilateral pelvic lymphadenectomy and para- aortic lymph node sampling through the laparoscope. During the operation we carefully examined the abdomen and pelvis, including the small intestine, omentum, peritoneum, colon, sigmoid colon, and other organs. The peritoneal surfaces were noted to be smooth, and no visible lesions were found in other tissues. The operation went smoothly, and the uterus with the lesion was completely taken out through the vagina. The lesion residual was R0. Tumor size was 5×4×2.5 cm. Tumor site was in left and right inferior (posterior) quadrant (3-6 and 6-9 o clock). Depth of stromal invasion 2.5cm and the level of cervical stroma invasion is middle one third. Pathological stage classification pT1b3 and FIGO stage IB3. She was planned for adjuvant radiotherapy-16 cycles. The patient was then discharged shortly in relatively good health.
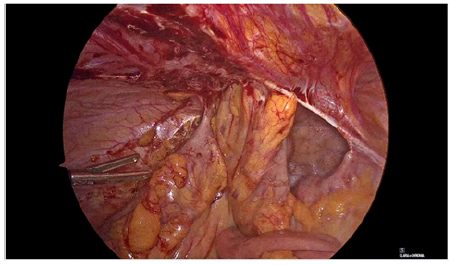
After 2 months, the patient was admitted again with complaints of difficulty passing stool and abdominal pain. An MRI was done and showed solid nodule with peripheral enhancement and central cystic– necrotic changes in left lower paramidline abdomen measuring approximately 3.6cm×3.5cm×5.7cm. The central cystic non enhancing part measures approximately 1.8cm×1cm. The periphery of this nodule appears low signal on T1, heterogeneous high signal on T2 images with restricted diffusion and low signal intensity on ADC map images. Few high fluid signal intensity areas at the superior aspect of the nodule on T2 images. Anteriorly the soft tissue nodule abuts and possibly partially infiltrates the left lower rectus abdominis muscle which appears to show high signal intensity, however no obvious extension into ventral subcutaneous fat. Postero-superiorly it abuts junction of sigmoid and descending colon with suspected serosal/muscular infiltration with mild enhancement of contiguous segment of sigmoid–distal descending colon. A referral was given for a colonoscopy guided biopsy showed large ulceroproliferative, submucosal infiltrating growth seen in the descending colon causing significant luminal narrowing. She then underwent en mass resection of left side resection of rectus muscle, urinary bladder wall, sigmoid colon, skin, subcutaneous tissue to achieve R0. Post operative mass excision biopsy was taken and revealed sections from the tumor composed of large nests of malignant cells. Tumor is infiltrating into colonic wall and infiltrating into full thickness colonic mucosa with ulceration. Adjacent colonic mucosa and both colonic margins are free of tumour (Figures 1-4).

Figure 2: Colonoscopy shows infiltrating tumor through the sigmoid colon occupying 80% of the lumen. Scope could not be passed through fully.
Discussion
Cervical cancer is one of the most common gynecological cancers with higher incident rates and mortality in developing countries. Implementing HPV vaccines and early detection including Pap smear, liquid-based cytology and HPV test have markedly reduced the incidence and mortality of cervical cancer in part of the world [7]. Pelvic is the most common site of recurrence [8]. Distant metastates of recurrences involve the lungs (69%), bone (21%), gastrointestinal tract (14%), liver (13%), brain and other sites [9]. Unusual metastases have been reported in the skin [10], thumb [11], spleen [12], kidney [13], oral cavity [14] and skeletal muscle [15]. Colonic metastases, especially sigmoid colon metastases of cervical cancers are exceedingly rare [16], probably due to relatively short intestinal segment. To date only a few cases of sigmoid colon metastases are reported and three are isolated [17-19]. While the small intestine accounted for a large space in the enterocelia. So, the low incidence rates of small intestine metastases are notable, and several associated mechanisms have been raised as follows [20-23]: (1) the intestine has abundant immune protection with numerous lymphoid cells and large secretions of IgA in the mucosa and submucosa of the intestine; (2) a rapid refresh rate of small intestinal mucosa may inhibit the tumorigenesis; (3) liquefied chyme may cause less mucosal irritation, then reduces mechanical injury and inflammation [24].
The intestine metastases usually occur through the lympatics to the bowel serosa and less commonly via intraperitoneal dissemination, direct spread and hematogenous spread [25-27] However recurrence or distant metastases poses a considerable challenge due to limited therapeutic options and poor prognosis. After precise calculation, the 10 year incidence of distant metastases was 3% for stage IA, 16% for stage IB, 31% for stage IIA, 26% for stage IIB, 39% for stage III and 75% for stage IVA in cervical cancer patients. In the setting of gastrointestinal tract recurrences, however, intraperitoneal seeding or tethering of bowel loops to mesenteric tumor implants often preclude focal resection due to diffuse spread and poor prognosis. We present an unusual case of pelvic recurrence isolated to a segment of the sigmoid colon treated by sigmoid resection with achievement of negative surgical margins. There was a sufficient degree of redundancy noted in the descending colon and rectosigmoid to allow for a tension free primary anastomosis to avoid ostomy creation. As such and per surgeons’ discretion, we felt that a minimally invasive procedure without additional lymph node sampling at the time of her recurrence was a favorable option to minimize her intraoperative and postoperative morbidity. Additionally, the patient underwent sentinel node mapping at the time of her initial surgery. Although sentinal node mapping in the setting of cervical cancer is still considered investigational, it has gained increasing support in the literature, demonstrating a potential role for sparing complete nodal dissection while still accurately identifying nodal metastases [28-30].
Retrospective data suggests that minimally invasive surgery techniques (standard laparoscopy or robotic assisted laparoscopy) cause less blood loss, shorter hospital stay and lower post operative complications. Hence, thus patient chose to be treated with laparoscopic radical hysterectomy, salpingo-ovariectomy, bilateral pelvic lymphadenopathy and para-aortic lymph node sampling. Hence, in addition to detecting the vaginal stump regularly by HPV testing and cervical cytology, CT or MRI are also recommended to evaluate the distant region relapse in some special circumstances such as involved high pelvic lymph nodes [31]. In general, a small intestine and sigmoid colon metastatic tumor indicates a poor prognosis. Bleeding and obstruction as well as non-specific symptoms such as abdominal discomfort, gas distension and vomiting are common clinical features. Once intestinal metastases are suspected, contrast enhanced CT, endoscope and even exploratory laparotomy should be operated. Typical features of intestinal metastases include increased intestinal wall thickening and stiffness, submucosal spread, and ulcers. Laparotomy seems to be the common choice if the patients are physically capable. Chemotherapy could also be employed as a palliative treatment.
Acknowledgments
None.
Conflicts of Interest
None.
References
- Bray F, Ferlay J, Soerjomataram I, Rebecca L Siegel, Lindsey A Torre, et al. (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68: 394-424.
- Cohen PA, Jhingran A, Oaknin A (2019) Cervical cancer. Lancet 393: 169-182.
- Enokida T, Moreira A, Bhardwaj N (2021) Vaccines for immunoprevention of cancer. J Clin Invest 131(9).
- H Fagundes, CA Perez, PW Grigsby, MA Lockett (1992) Distant metastases after irradiation alone in carcinoma of the uterine cervix. Int J Radiat Oncol Biol Phys 24(2): 197-204.
- Hopkins MP, Morley GW (1991) Radical hysterectomy versus radiation therapy for stage IB squamous cell cancer of the cervix. Cancer 68(2): 272-277.
- Estape RE, Angioli R, Madrigal M, Janicek M, Gomez C, et al. (1998) Close vaginal margins as a prognostic factor after radical hysterectomy. Gynecol Oncol 68(3): 229-232.
- Andreas C Chrysostomou, Dora C Stylianou, Anastasia Constantinidou, Leondios G Kostrikis (2018) Cervical Cancer Screening Programs in Europe: The Transition Towards HPV Vaccination and Population-Based HPV Testing. Viruses 10(12): 729.
- Neerja Bhatla, Daisuke Aoki, Daya Nand Sharma, Rengaswamy Sankaranarayanan (2021) Cancer of the cervix uteri: 2021 update. Int J Gynaecol Obstet 1: 28-44.
- H Fagundes, CA Perez, PW Grigsby, MA Lockett (1992) Distant metastases after irradiation alone in carcinoma of the uterine cervix. Int J Radiat Oncol Biol Phys 24(2): 197-204.
- Vatsala Katiyar, Tiago Araujo, Nasma Majeed, Nicholas Ree, Shweta Guptac, et al. (2019) Multiple recurrences from cervical cancer presenting as skin metastasis of different morphologies. Gynecol Oncol Rep 28: 61-64.
- Lenny Gallardo Alvarado, Alma Astorga Ramos, Delia Perez Montiel, Rebeca Ramirez Morales, Erick Diaz, et al. (2020) Hand metastasis in a patient with cervical cancer: A case report. Medicine (Baltimore) 99(27).
- Dixit J, Mohammed N, Shetty P (2016) Splenic Metastasis from Cancer of Uterine Cervix-a Rare Case. Indian J Surg Oncol 7(4): 479-483.
- Juliana Rodriguez, Juan C Castro, María Beltran, Oscar Forero, Rene Pareja, et al. (2019) Simultaneous Metastasis from Cervical Cancer to the Kidney and Paraspinal Muscle: A Case Report. Cureus 11(2).
- Ram H, Kumar M, Bhatt ML, Shadab M (2013) Oral metastases from carcinoma of cervix. BMJ Case Rep.
- Nagisa Omokawa, Seiji Mabuchi, Kana Iwai, Naoki Kawahara, Ryuji Kawaguchi, et al. (2020) Skeletal muscle metastasis as a first site of recurrence of cervical cancer. A case report and review of the literature 99(19): e20056.
- Xiuyan Yu, Zhen Wang, Zhigang Zhang, Yang Liu, Jian Huang, et al. (2016) Postoperation of cervical cancer with intestine metastasis: a case report and literature review. World J Surg Oncol 14(1): 2.
- Shen W, Huang Y, Zhou Y, B Chang, M Zhang (2019) Intestinal metastasis after total laparoscopic radical trachelectomy for stage IB1 cervical cancer: A case report. Gynecol Oncol Rep 28: 37-40.
- Lelchuk A, Morin N, Bain K (2018) Squamous cell carcinoma of cervix origin with rare metastasis to the colon. AME Case Rep 2: 23.
- Damin AP, Agnes G, Tarta C, PC Contu, TL Ghezzi, et al. (2014) Human papillomavirus detected in a colonic metastasis of cervical adenocarcinoma. Tech Coloproctol 18(5): 515-516.
- Schottenfeld D, Beebe Dimmer JL, Vigneau FD (2009) The epidemiology and pathogenesis of neoplasia in the small intestine. Ann Epidemiol 19: 58-69.
- Torres M, Matta E, Chinea B, Dueno MI, Martinez Souss J, et al. (2003) Malignant tumors of the small intestine. J Clin Gastroenterol 37(5): 372-380.
- Loualidi A, Spooren PF, Grubben MJ, Blomjous CE (2004) Goey SH Duodenal metastasis: an uncommon cause of occult small intestinal bleeding. Neth J Med 62: 201-205.
- Kariv R, Arber N (2003) Malignant tumors of the small intestine-new insights into a rare disease. IMAJ 5: 188-192.
- Misonou J, Natori T, Aizawa M, Jou B, Tamaki A, Ogasawara M (1988) Stage (Ia) cervical cancer recurring 13 years after hysterectomy and causing small intestinal perforation. A case report with a review of the literature. Acta Pathol Jpn 38(2): 225-234.
- Gurian L, Ireland K, Petty W, Katon R (1981) Carcinoma of the cervix involving the duodenum: case report and review of the literature. J Clin Gastroenterol 3: 291-294.
- Mathur SK, Pandya GP (1984) Solitary metastatic malignant stricture of the ileum: a rare cause of small bowel obstruction (a case report) J Postgrad Med 30(3): 186-188.
- Kanthan R, Senger JL, Diudea D, Kanthan S (2011) A review of duodenal metastases from squamous cell carcinoma of the cervix presenting as an upper gastrointestinal bleed. World J Surg Oncol 9: 113.
- Cibula D, Abu-Rustum NR, Dusek L, Slama J, Zikan M, et al. (2012) Bilateral ultrastaging of sentinel lymph node in cervical cancer: lowering the false-negative rate and improving the detection of micrometastasis. Gynecol Oncol 127(3): 462-466.
- Cormier B, Diaz JP, Shih K, Sampson RM, Sonoda Y, et al. (2011) Establishing a sentinel lymph node mapping algorithm for the treatment of early cervical cancer. Gynecol Oncol 122(2): 275-280.
- Selman TJ, Mann C, Zamora J, Appleyard TL, Khan K (2008) Diagnostic accuracy of tests for lymph node status in primary cervical cancer: a systematic review and meta-analysis. CMAJ 178(7): 855-862.
- Bhatla N, Aoki D, Sharma DN, R Sankaranarayanan (2021) Cancer of the cervix uteri: 2021 update. Int J Gynaecol Obstet 155: 28-44.





 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.