Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Analysis of the Effect of Cerebrospinal Fluid Drainage on the Postoperative Efficacy of Minimally Invasive Hematoma Puncture and Drainage for Hypertensive Intracerebral Hemorrhage
*Corresponding author:Hairen Zou, Department of Neurosurgery, People’s Hospital of Longhua, China.
Received: March 4, 2024; Published: April 1, 2024
DOI: 10.34297/AJBSR.2024.21.002909
Abstract
Objective: To explore the effect of Cerebrospinal Fluid (CSF) drainage on hypertensive cerebral hemorrhage after minimally invasive puncture drainage.
Methods: 87 patients with hypertensive cerebral hemorrhage from January 2019 to December 2022 were retrospectively analyzed. The patients were divided into observation group and control group according to whether the cerebrospinal fluid was drained through the drainage tube of hematoma cavity. The hematoma clearance rate of 24 hours, 72 hours, KPS score of 1 month, KPS score of 6 months, KPS score of 12 months, intracranial infection rate, rebleeding rate during hospitalization and mortality rate of 12 months after operation were compared between the two groups.
Results: The clearance rate of hematoma 72 hours after operation and the KPS score of 1 month in the observation group were significantly higher than those in the control group (P<0.01).
Conclusion: Drainage of cerebrospinal fluid through hematoma cavity after minimally invasive puncture and drainage for hypertensive cerebral hemorrhage is beneficial to the removal of hematoma and the early functional recovery, but it cannot improve the long-term prognosis of patients.
Keywords: Hypertensive Cerebral Hemorrhage, Hematoma Puncture, Cerebrospinal Fluid (CSF) Drainage, Prognosis
Introduction
Hypertensive Intracerebral Hemorrhage (HICH) refers to sudden hemmorrhage in the brain parenchyma of the basal ganglia, thalamus, lobe, cerebellum, and brainstem in patients with a history of hypertension, mostly caused by the rupture of lesions in cerebral arterioles. The disability rate and mortality rate are extremely high, seriously endangering the life and life of patients. There are many surgical treatment options for intracerebral hemmorrhage, mainly including craniotomy microscope-assisted hematoma re moval, minimally invasive neuroendoscopic hematoma removal, and hematoma puncture external drainage [1]; compared with traditional craniotomy, which is highly invasive and risky, minimally invasive puncture drainage is simple and less invasive; preoperative CT body surface positioning simple puncture is widely used in primary hospitals, and has a positive effect on postoperative functional recovery [2]. There are many factors affecting the prognosis of hematoma puncture. We found that in the hypertensive intracerebral hemorrhage hematoma puncture without breaking into the ventricle, cerebrospinal fluid drainage through the hematoma cavity drainage tube often occurs without penetrating the ventricle; but there are few studies on the postoperative effects of cerebrospinal fluid drainage on intracerebral hemorrhage. This project provides evidence support for postoperative recovery estimates by studying the effects of cerebrospinal fluid drainage on the prognosis of minimally invasive hematoma
Data and Methods
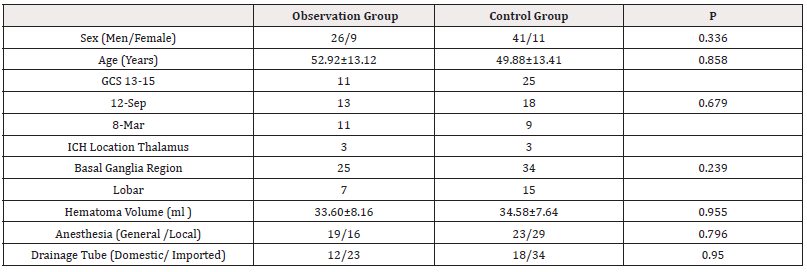
87 patients with hypertensive intracerebral hemorrhage, including 67 males and 20 females; age 26-79 years, average age (51.13±13.31) years; GCS score 13-15 points 36 cases, 9-12 points 31 cases, 3-8 points 20 cases; left 48 cases, right 39 cases; hematoma located in the thalamus 6 cases, basal ganglia region 59 cases, 22 cases of the lobe; hematoma volume 20-60ml, average (34.18±7.82) ml;42 cases of surgery under general anesthesia, 45 cases of local anesthesia; using domestic drainage tube 30 cases, imported drainage tube 57 cases. According to whether cerebrospinal fluid through the hematoma cavity drainage tube drainage patients were divided into cerebrospinal fluid drainage group and cerebrospinal fluid without drainage group, including 35 cases of cerebrospinal fluid drainage group, 52 cases of non-drainage group.The two groups of patients with gender, age, cerebral hemorrhage site, bleeding volume, anesthesia methods, drainage tube model comparison, there was no statistically significant difference (P>0.05, Table 1).
Inclusion Criteria
1. According to the history, clinical manifestations and CT imaging results diagnosed as hypertensive intracerebral hemorrhage
2. Cerebral hernia did not form, brainstem function was not involved.
3. Minimally invasive hematoma puncture drainage treatment.
4. The first onset, the onset time from the operation ≤24h.
5. Complete clinical data.
Exclusion Criteria
1. Conservative treatment of hypertensive intracerebral hemorrhage.
2. Treatment of recurrent intracerebral hemorrhage.
3. Cerebral hematoma burst into the ventricle.
4. Brainstem hemorrhage, cerebellar hemorrhage.
5. Serious bleeding tendency, history of malignant tumors.
6. Have lung, liver, kidney and other important organs serious disease.
Midway Exit Criteria
Surgery Irrelevant Serious Complications: post-traumatic hemorrhage; follow-up missing.
The Evaluation Criteria
preoperative cranial CT confirmed that the brain hematoma did not break into the ventricle, no subarachnoid hemorrhage; intraoperative or postoperative cerebrospinal fluid through the hematoma drainage tube outflow, drainage tube liquid level fluctuations, drainage volume is significantly more than the hematoma volume; postoperative cranial CT confirmed that the hematoma did not break into the ventricle, the drainage tube did not break into the ventricle.
Treatment Methods
All surgical patients were within 24 hours after the onset of the disease. After the patient was admitted to the hospital, preoperative CT positioning, with the largest layer of the hematoma center as the puncture direction, to the point of the nearest point from the center of the hematoma puncture; operation room hematoma puncture drainage: general anesthesia or local anesthesia, puncture point skull cone drilling, avoid important vascular nerve, functional area, cone open dura mater after using disposable brain puncture casing along the CT puncture direction puncture to the hematoma, exit the needle core, uniform, carefully suction hematoma 1/2-2/3, connect the drainage bag; drainage tube using domestic (Shandong Zhengda medical disposable external craniocerebral drainage device) F10 tube or French Sofiosa (cerebrospinal fluid shunt and its components) DE-304 tube. The residual hematoma cavity was injected with urokinase (Peking University Huake Huatai Pharmaceutical, China National Drug Approval Number H37020115) 100,000 U+ normal saline, and the drainage tube was clamped for 2h before being opened again for drainage. The drainage tube was opened again after repeated washing for many days until the hematoma disappeared obviously (about 1-2 times/d), postoperative symptomatic support, early guidance for rehabilitation exercise, etc.
Observation Indicators
Primary Observation Index
KPS score 1 month after operation. Secondary observation index: hematoma clearance rate 24 hours after operation (preoperative hematoma volume - postoperative hematoma volume)/ preoperative hematoma volume x 100%, which was calculated by the Tada formula by comparing preoperative and postoperative CT images; hematoma clearance rate 72 hours after operation, KPS score 1 month after operation, KPS score 6 months after operation, KPS score 12 months after operation, intracranial infection rate, rebleeding rate during hospitalization and mortality within 12 months after operation.
Statistical Analysis
SPSS 25.0 statistical software was used to process the data. The enumeration data were expressed in terms of cases (%) and the comparison between groups was conducted by X2 test; the measurement data were expressed in terms of mean ± standard deviation (x±s) and the comparison between groups was conducted by t test. P<0.05 indicated that the difference was statistically significant.
Results
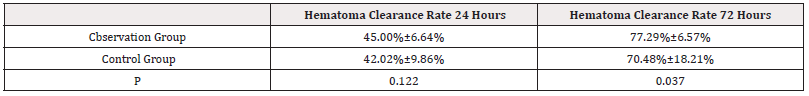
I. There was no significant difference in hematoma clearance rate 24 hours after operation between the cerebrospinal fluid drainage group and the control group (P>0.05). The hematoma clearance rate of the cerebrospinal fluid drainage group was significantly higher than that of the control group 72h after operation, with statistically significant difference (P<0.05) (Table 2).
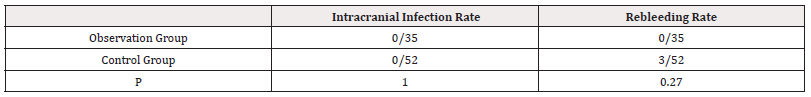
II. There was no statistically significant difference in postoperative intracranial infection rate and rebleeding rate during hospitalization between the cerebrospinal fluid drainage group and the control group (P>0.05) (Table 3).
III. The KPS score 1 month after operation in the cerebrospinal fluid drainage group was significantly higher than that in the control group, with statistically significant difference (P<0.05); there was no statistically significant difference in KPS score 6 months after operation, KPS score 12 months after operation, and mortality within 12 months after operation between the two groups (P>0.05) (Table 4).
Discussion
There are many factors affecting the early recovery after minimally invasive puncture treatment of hypertensive intracerebral hemorrhage. At present, the relevant studies [3] mainly include age, preoperative blood glucose value, preoperative GCS score, intraventricular hemorrhage, secondary surgery and surgical infection. There are few studies on the factors of cerebrospinal fluid drainage through the drainage tube of the hematoma cavity. It is found in clinical practice that cerebrospinal fluid drainage along the drainage tube of the hematoma cavity can relieve intracranial pressure, prolong hematoma organization, keep the drainage tube unobstructed, and promote hematoma drainage as soon as possible; however, at the same time of cerebrospinal fluid drainage, hematoma can return to the subarachnoid space and ventricle through cerebrospinal fluid, affecting the circulation of cerebrospinal fluid, which is not conducive to postoperative recovery.
The neurological dysfunction caused by hypertensive intracerebral hemorrhage is related to hematoma compression and hematoma decomposition products. Removing hematoma as soon as possible can effectively reduce postoperative reperfusion injury and complications, which is considered an important factor affecting the prognosis [4]. Jordan, et al. [5]. also proposed that early surgical treatment can significantly improve the prognosis of patients with intracerebral hemorrhage. Therefore, in this study, minimally invasive hematoma puncture surgery was performed within 24hours after the onset of hypertensive intracerebral hemorrhage. This study showed that there was no significant difference in the hematoma clearance rate between the two groups 24 hours after the operation, which was considered to be related to the intraoperative hematoma aspiration volume. Although the migration of intraoperative hematoma puncture center was uncontrollable, the intraoperative hematoma aspiration volume was about 1/2-2/3 of the total amount under the condition of no significant difference in the material of the drainage tube, which basically achieved the goal. Moreover, the drainage of cerebrospinal fluid through the drainage tube of the hematoma cavity mostly occurred 24hours after puncture and after urokinase washing in the drainage tube, resulting in little difference in the hematoma clearance rate 24hours after surgery. The hematoma clearance rate 72hours after surgery in the cerebrospinal fluid drainage group was significantly higher than that in the non-cerebrospinal fluid drainage group, which may be related to the patency of the drainage tube and the adequate response of urokinase to the hematoma through the cerebrospinal fluid.
Postoperative rebleeding after hypertensive intracerebral hemorrhage is the most serious complication after surgery, and the main influencing factors [6] include the time from onset to surgery ≤6h, abnormal coagulation function, uncontrolled hypertension, diabetes, and other factors. In this study, there was no significant difference in the rebleeding rate during hospitalization between the cerebrospinal fluid drainage group and the non-drainage group; there was a certain relationship between the hypertensive intracerebral hemorrhage patients without cerebral hernia included in this study, the intracranial pressure was in the compensatory range, and the hypertension was stable. The intracranial infection rate after minimally invasive puncture of hypertensive intracerebral hemorrhage was lower than that after craniotomy, about 6.73% [7]; the relevant factors include preoperative GCS score, drainage tube indwelling time, whether there was subcutaneous hydrops, postoperative hypoproteinemia, and hyperglycemia. In this study, there was no significant difference in the postoperative intracranial infection rate between the two groups; it may be related to the short drainage tube indwelling time and early extubation.
Hypertension intracerebral hemorrhage has high mortality and disability rate after surgery, and slow recovery of neurological dysfunction; Zhao Jizong, et al. [8]. showed that the mortality and disability rate after hematoma puncture surgery were significantly lower than those after craniotomy hematoma removal surgery; the main risk factors are preoperative GCS≤8, postoperative complications, and thalamic hemorrhage. Some studies [9] have shown that during the process of hematoma removal in intracerebral hemorrhage surgery, although rapid removal of hematoma can relieve intracranial pressure as soon as possible, it is easy to cause local inflammatory reactions caused by cerebral vascular reperfusion, which affects the efficacy. The sustained and slow drainage of hematoma in minimally invasive hematoma puncture surgery is conducive to reducing the risk of reperfusion injury [10]. In this study, the KPS score of the cerebrospinal fluid drainage group was significantly higher than that of the non-drainage group at 1 month after surgery; there was no significant difference in the KPS score at 6 and 12 months after surgery. Considering that early postoperative recovery is related to the relatively rapid removal of hematoma after cerebrospinal fluid drainage, and long-term recovery is related to preoperative GCS score, bleeding volume, and bleeding site. The shortcomings are short follow-up time, and long-term efficacy needs to be further evaluated. In summary, the drainage of cerebrospinal fluid through the drainage tube of the hematoma cavity after minimally invasive hematoma puncture drainage for hypertensive intracerebral hemorrhage is conducive to the removal of cerebral hematoma, and promotes early postoperative functional recovery, but cannot improve the long-term prognosis of patients.
Funding
Scientific Research Projects of Medical and Health Institutions of Longhua District, Shenzhen (Project No.2021111).
Acknowledgement
None.
Conflict of Interest
None.
References
- Mendelow AD, Gregson BA, Fernandes HM, Gordon D Murray, Graham M Teasdale, et al. (2005) Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the Internationa Surgical Trial in Intracerebral Haemorrhage (STICH): a randomised trial. Lancet 365(9457): 387-397.
- Wang GQ, Li SQ, Huang YH, Wei Wei Zhang, Wen Wei Ruanet, al. (2014) Can minimally invasive puncture and drainage for hypertensive spontaneous Basal Ganglia intracerebral hemorrhage improve patient outcome: a prospective non-randomized comparative study. Mil Med Res 1:10.
- Daniel F Hanley, Richard E Thompson, John Muschelli, Michael Rosenblum, Nichol McBee, et al. (2016) Safety and efficacy of minimally invasive surgery plus alteplase in intracerebral haemorrhage evacuation (MISTIE): a randomised, controlled, open label, phase 2 trial. Lancet Neurol 15(12): 1228-1237.
- Lin Jie Wei, Chi Lin, Xing Sen Xue, Guo Dong Dun, Jian Bo Zhang, et al. (2021) The effect of hematoma puncture drainage before decompressive craniectomy on the prognosis of hypertensive intracerebral hemorrhage with cerebral hernia at a high altitude. Chin J Traumatol 24(6): 328-332.
- Dedrick Jordan J, Kathryn Morbitzer A, Denise Rhoney H (2015) Acute treatment of blood pressure after ischemic stroke and intracerebral hemorrhage. Neurol clin 33(2):361-380.
- Shuwen Sun, Yuping Li, Hengzhu Zhang, Heng Gao, Xinmin Zhou, et al. (2020) Neuroendoscopic Surgery versus Craniotomy for Supratentorial Hypertensive Intracerebral Hemorrhage: A Systematic Review and Meta-Analysis. World Neurosurg 134: 477-488.
- Roa a W Jaradat, Amro B Lahlouh, Osama Y Alshogran, Belal A Aldabbour, Abedallah AK Balusha (2019) Nosocomial Infections among Patients with Intracranial Hemorrhage: A Retrospective Data Analysis of Predictors and Outcomes. Clin Neurol Neurosurg 182: 158-166.
- Morgenstern L, Hemphill JC, Anderson C, Kyra Becker, Bernard R Bendok, et al. (2010) Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 41(7): 2108-2129.
- Mailikarjuna R Pabbidi, Julio Juncos, Luis Juncos, Marija Renic, Hurtis J Tullos, et al. (2013) Identification of a region of rat chromosome 1 that impairs the myogenic response and autoregulation of cerebral blood flow in fawn-hooded hypertensive rats. Am J Physiol Heart Circ Physio 304(2): H311-H317.
- Yan YF, Ru DW, Du JR, Shen X, Wang ES, et al. (2015) The clinical efficacy of neuronavigation-assisted minimally invasive operation on hypertensive basal ganglia hemorrhage. Eur Rev Med Pharmacol Sci 19(14): 2614-2620.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.