Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Current Practice of Warfarin Anticoagulation Therapy in China
*Corresponding author:Yi Wang, Department of Thoracic and Cardiovascular Surgery, Huaihe Hospital of Henan University, Kaifeng, Henan Province, China and Xiaokang An, Department of Thoracic Surgery, First Affiliated Hospital of Henan University, Kaifeng, Henan Province, China.
Received: February 13, 2024; Published: February 19, 2024
DOI: 10.34297/AJBSR.2024.21.002863
Abstract
The vitamin K antagonist warfarin has been used as a common oral anticoagulant to treat and prevent thromboembolic conditions in deep vein thrombosis, pulmonary embolism, atrial fibrillation, and heart valve replacement. Although Novel Oral Anticoagulants (NOACs), such as dabigatran, rivaroxaban, edoxaban, and apixaban, have been gaining acceptance and popularity in recent years, warfarin will likely remain as an important option due to its affordability and decades long experience of clinical use. In patients with moderate-to-severe mitral stenosis or those who underwent mechanical heart valve replacement, warfarin is the recommended anticoagulant as per clinical guidelines. The top indications for warfarin treatment in China are Atrial Fibrillation (AF) and Heart Valve Replacement (HVR), accounting for more than 60% of all patients. This is followed by deep vein thrombosis/ pulmonary embolism (DVT/PE) (up to 30%) among other indications. Among AF patients with high stroke risk (CHADS2≧2 and CHA2DS2-VASc≧2) in Chinese hospitals, a large proportion of patients were taking antiplatelets instead of anticoagulants. Many physicians may be reluctant to prescribe oral anticoagulants in elderly AF patients due to fear of bleeding events and may underestimate the benefits of oral anticoagulants to reduce stroke risk. Also, despite demonstrated advantage of pharmacogenetic dosing approach in helping patients achieve and maintain within therapeutic INR window, an empirical approach to warfarin dosing is used in vast majority of cases. Clearly more education and promotion on warfarin anticoagulation is needed among healthcare professionals and patients in China to maximize its benefits and reduce adverse complications.
Keywords: Anticoagulation, Clinical practice, Warfarin, China healthcare
Introduction
With the aging population in China, the incidences of cardiovascular diseases have risen over the years. According to an epidemiological study published in 2021, the prevalence of Atrial Fibrillation (AF) was 1.8%, which equates to about 7.9 million people aged 45 or more in China [1]. The AF prevalence was higher in the ≥75 age group, which are 5.4% and 4.9% among men and women respectively. According to an epidemiological update published in 2018, Venous Thromboembolism (VTE) was more common in elderly individuals, with the overall annual incidence of Deep Vein Thrombosis (DVT) alone, Pulmonary Embolism (PE) alone, and PE with DVT reported as 30.0, 8.7, and 3.0 per 100,000 population in China, respectively [2]. This is an increase in incidence compared with findings reported 10 years ago. AF and VTE could lead to detrimental cardiovascular complications, thereby significantly reducing the quality of life in patients. There is an up to 5-fold increase in the risk of ischemic stroke in patients with AF, which accounts for 20-30% of all ischemic stroke cases, while VTE is one of the leading causes of cardiovascular death, along with Myocardial Infarction (MI) and ischemic stroke [3-6]. Furthermore, a Taiwanese study reported a 3-fold increase in the risk of VTE in patients with AF [7]. For this reason, the safety and effectiveness of oral anticoagulants to treat and prevent thromboembolism in cardiovascular diseases has received increased attention in recent years.
As a type of vitamin K antagonist, warfarin has been used as a common oral anticoagulant to treat and prevent thromboembolic conditions in DVT, PE, AF, and Heart Valve Replacement (HVR) [8-10]. Due to large interindividual variability and narrow therapeutic window, warfarin therapy requires routine monitoring of International Normalized Ratio (INR) to prevent thromboembolism (under-coagulation) or bleeding (over-coagulation) especially during initial phase of dosing. In recent years, Novel Oral Anticoagulants (NOACs), such as dabigatran, rivaroxaban, edoxaban, and apixaban have been developed with superior efficacy than warfarin in the prevention of stroke, while having lower incidence rates of thromboembolism and bleeding [11-13]. Also, NOACs do not require monitoring and are able to achieve anticoagulant effects quickly due to short half-lives [14]. While NOACs have been gaining acceptance and popularity in anticoagulant treatment, warfarin will likely remain as an important oral anticoagulant option since the costs of NOACs might be prohibitive to socio-economically disadvantaged patients and assays to measure the plasma levels or activity of NOACs are not widely available to inform timing for emergency surgeries [15-17]. This review discusses current practice of oral anticoagulant therapy in China and showcases how patients receiving warfarin are educated and followed-up for adequate anticoagulant control in typical tertiary (top-tier) hospitals in China.
Warfarin vs. NOACs
Since 2009, NOACs, such as rivaroxaban, dabigatran, apixaban, and edoxaban, have been approved for market authorization in China. Results from large, randomized Phase 3 trials showed that NOACs achieved non-inferior efficacy to warfarin in preventing stroke or systemic embolism, with lower or similar rates of bleeding. In the ROCKET AF (Rivaroxaban Once Daily Oral Direct Factor Xa Inhibition Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism) trial in patients with nonvalvular atrial fibrillation (NVAF), rivaroxaban was noninferior to warfarin for the primary endpoint of preventing stroke or systemic embolism, with less frequent occurrences of intracranial and fatal bleeding [12]. In the RE-LY (Randomized Evaluation of Long-Term Anticoagulation Therapy) trial, compared to AF patients receiving warfarin, those receiving 150 mg dabigatran had lower rates of stroke and systemic embolism with similar rates of major hemorrhage, while those receiving the lower dose of 110 mg had similar rates of stroke and systemic embolism but with lower rates of major hemorrhage [13]. In the ARISTOTLE (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation) trial, apixaban demonstrated superior efficacy to warfarin in preventing stroke or systemic embolism, with lower rates of bleeding and mortality [11]. In the ENGAGE AF-TIMI 48 (Effective Anticoagulation with Factor Xa Next Generation in Atrial Fibrillation-Thrombolysis in Myocardial Infarction 48) trial, edoxaban treatment was also noninferior to warfarin in preventing stroke or systemic embolism with lower rates of bleeding and cardiovascular-related mortality [18]. Despite having at least non-inferior efficacy at preventing thromboembolic events, it is considered that the risk of gastrointestinal bleeding might be higher in those receiving NOACs, especially for older patients. Since 2018, the cost of NOACs have decreased significantly since China implemented a national centralized drug purchase policy, which includes dabigatran, rivaroxaban, edoxaban, and apixaban [19]. Studies have shown that, over the long-term, NOACs could be cost-effective options in the healthcare system of China [19-21]. A study on the health insurance claims data indicates that oral anticoagulant use among AF patients in Shanghai had risen from 19.46% to 56.75% between 2015 and 2020, mainly due to prescription increases for NOACs [22]. In 2015, warfarin was the most predominant oral anticoagulant prescribed. In 2019, however, the number NOAC prescriptions became the same as warfarin, whereas in 2020 it even exceeded the number of warfarin prescriptions. Clearly, the use of anticoagulants, and especially NOACs, in AF patients has received more emphasis in recent years. Warfarin is still cheaper than NOACs even after insurance reimbursement and is therefore more easily accepted by the general public in China. On the other hand, patients taking warfarin need to undergo routine INR monitoring and dose adjustments if necessary. Nevertheless, guidelines from AHA/ACC/HRS (American College of Cardiology/American Heart Association/Heart Rhythm Society) and ESC (European Society of Cardiology) recommend warfarin over NOACs in patients with moderate-to-severe mitral stenosis or a mechanical heart valve [9,23].
Clinical Use of Warfarin in China
Despite the large interindividual variability in warfarin dose/response and the delay in reaching pharmacologic steady-state, warfarin remains the anticoagulant of choice for many patients, especially in economically disadvantaged populations. Through literature review, it can be observed that AF and valve replacement were the top indications for receiving warfarin treatment in China, accounting for more than 60% of all patients (Figure 1). This is followed by DVT/PE (up to 30%) among other indications.
Atrial Fibrillation
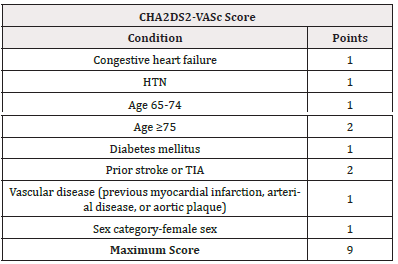
AF is one of the most common types of arrhythmias seen in the clinic. Patients with AF have significantly increased risk for thromboembolic events, congestive heart failure, and mortality, with the most serious complication being ischemic stroke, especially in the elderly and other patients with high-risk factors [24, 25]. It is estimated that there are at least 10 million AF patients in China, with at least 65% of those having nonvalvular AF [26, 27]. The risk of having ischemic stroke is at least 5 to 6 times greater in patients with nonvalvular AF compared to the healthy population [28]. The CHADS2 classification scheme has been widely used for evaluating stroke risk in AF patients (Table 1A). Due to the limitation of CHADS2 in categorizing a large proportion of patients as “intermediate risk” recommended for using either aspirin or warfarin, the 2010 ESC guidelines introduced a new score, the CHA2DS2-VASc, in which two other criteria, the presence of vascular disease and female sex were included for evaluation (Table 1B). Traditionally, anticoagulation therapy is recommended for patients with a CHADS2 score of 2 or more, while the 2016 ESC guidelines for management of AF recommend anticoagulation therapy for patients with CHA2DS2-VASc score of 1 or more for men, and 2 or more for women [29]. Figure 2 shows the percentage of antithrombotic medication use, including oral anticoagulants and antiplatelets, among AF patients with CHADS2 ≧2 and CHA2DS2-VASc ≧2 in Chinese hospitals, for whom current guidelines recommend anticoagulation for stroke prevention. It can be seen that for most hospitals, other than the one reported by Guo, et al. and Li, et al. [30,31], the percentages of AF patients taking either warfarin or NOACs are between 5 to 40%, whereas those taking antiplatelet therapy, such as aspirin or clopidogrel, are between 50 to 90%. Guo et al. [30] reported the highest percentage of patients taking NOACs; that plus the those taking warfarin makes the percentage of patients on oral anticoagulants above 75%. Li, et al. [31] also reported 57.2% of AF patients were taking warfarin. This may reflect thorough implementation of anticoagulation guidance recommendation in AF patients in those two healthcare facilities. Previous studies have suggested that older age, multi-morbidities, and polypharmacy were major reasons for prescribing antiplatelets instead of oral anticoagulants [32-34].
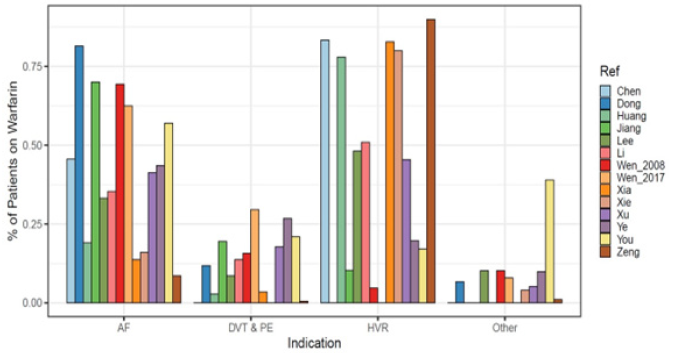
Figure 1: Percent of patients with AF (atrial fibrillation), DVT & PE (deep vein thrombosis and pulmonary embolism), HVR (heart valve replacement), and other indications receiving warfarin in China [51,58,60,79-89]. The results were based on literature search in PubMed, CNKI (China National Knowledge Infrastructure), and Wanfang Data with the following keywords: warfarin, dose, dosage, dosing, Chinese. The search period was from inception of the database to Dec 2022. This yielded a total of 76 records in PubMed, 47 records in CNKI, and 165 records in Wanfang Data, from which 14 references were selected with applicable data.
Heart Valve Replacement
Valvular heart disease is a condition where any valve in the heart was damaged or diseased. By adversely affecting blood circulation, valvular heart disease has a negative impact on patients’ quality of life and can even lead to death. Heart valve replacement surgery is the main treatment option for severe valvular heart disease. There are two choices for valve replacement, mechanical or bioprosthetic valves. In China, the incidence of valvular heat disease is estimated to be 2.34‰~2.72‰ [35]. About 80,000 heart valve replacement surgeries are performed in China each year, with 70% of those being mechanical heart valve replacement [36,37]. Mechanical heart valves are usually more durable than bioprosthetic valves. However, after implantation, mechanical heart valves may cause the formation of thrombus, and patients who underwent mechanical heart valve replacement are required to receive lifetime anticoagulation therapy for the prevention of thromboembolism, whereas only 3 months of anticoagulation therapy is required for those receiving bioprosthetic valve replacement [38,39]. In many settings, including bioprosthetic valve replacement, NOACs have become the anticoagulant of choice due to their favorable safety and efficacy profiles. However, clinical guidelines recommend patients who underwent mechanical heart valve replacement to receive warfarin instead of NOACs based on results of the phase II study comparing dabigatran and warfarin (RE-ALIGN, Randomized, Phase II Study to Evaluate the Safety and Pharmacokinetics of Oral Dabigatran Etexilate in Patients after Heart Valve Replacement), which was stopped prematurely due to excess stroke and bleeding with the dabigatran doses tested [40]. In patients receiving mechanical heart valve replacement, it is best to start anticoagulation therapy within the next day of surgery in order to prevent thromboembolic complications. Due to warfarin’s mechanism of action, its full antithrombotic effects will only be reached after about 5 days into therapy. Therefore, clinical guidelines recommend heparin or low-molecular weight heparin be used for anticoagulation bridging until INR reaches therapeutic level for two consecutive days [41]. In China, patients undergoing heart valve replacement are usually hospitalized for 1 to 2 weeks after surgery. Before patients are discharged, nursing staff will educate patients on the proper use of warfarin using pamphlet handout similar to Table 2. Patients’ understanding about warfarin use will be evaluated using a questionnaire similar to Table 3, and areas with insufficient understanding will be trained specifically by the nursing staff. After discharge, patients return for outpatient follow-up once a week for INR check and dose adjustment if necessary. Frequency for follow-up visits gradually decrease to once every 2 weeks and then once a month eventually.
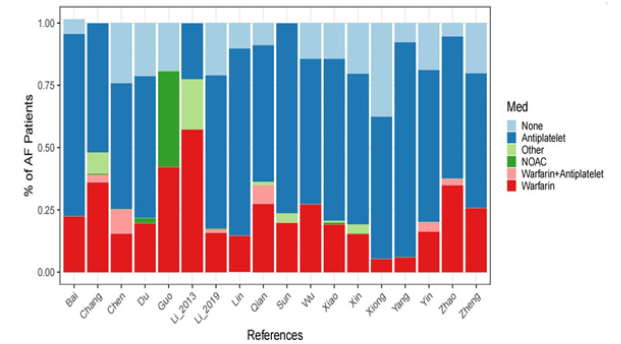
Figure 2: Antithrombotic medication use among AF patients with CHADS2≧2 and CHA2DS2-VASc ≧2 in Chinese hospitals [30,31,90-105]. The results were based on literature search in PubMed, CNKI (China National Knowledge Infrastructure), and Wanfang Data with the following keywords: atrial fibrillation, anticoagulation, anti-thrombosis, medication, Chinese. The search period was from inception of the database to Dec 2022. This yielded a total of 5 records in PubMed, 121 records in CNKI, and 96 records in Wanfang Data, from which 18 references were selected with applicable data.

Table 2: Education pamphlet handout for new patients taking warfarin in typical tertiary (top-tier) hospitals in China.
Venous Thromboembolism and Pulmonary Embolism
Venous Thromboembolism (VTE) is a disease that includes DVT and PE. DVT occurs when a blood clot (thrombus) forms in one or more of the deep veins in the body due to the abnormal coagulation of blood in the venous cavity, occurring more frequently in the lower rather than upper extremity [42]. This may be caused by the slow blood flow in the veins or injuries to blood vessel walls, leading to high coagulation state in the blood. Pulmonary embolism is a related condition and usually happens when a blood clot in the lower extremity travels to the lungs and blocks a blood vessel. A frequent, sometimes disabling complication of DVT is Post-Thrombotic Syndrome (PTS), which occurs in 20-50% of patients within 2 years [43,44]. This condition can cause chronic pain, swelling, and other symptoms in the legs of patients who have had DVT. There have been no reports on the incidence of DVT in the Chinese population based on large sample analysis. However, based on a preliminary cross-sectional study, the incidence of DVT of lower extremity was 10.2% in 372 high-risk hospitalized patients in Zhongshan hospital in Shanghai, including bedridden stroke patients, post-surgery bedridden patients, and patients in surgical intensive care unit [45]. In the clinic, treatment of DVT includes the following aspects:
1) prevent the growth and spread of a clot, alleviate the swelling and pain of lower extremity, and prevent the development of PE;
2) clear the blood clot as soon as possible to resume blood flow in veins, preserve heart valve function as much as possible, and prevent DVT relapse and minimize development of PTS with long-term anticoagulation.
For acute anticoagulation of DVT, heparin and Low Molecular Weight Heparin (LMWH) can be used, usually for 7-10 days. Chronic anticoagulation with warfarin or NOACs should be maintained for at least 3 months, and some experts recommend continued treatment for 6-12 months after the first episode of idiopathic DVT and long-term treatment after DVT relapse [46]. To prevent the development of PE by limiting the movement of blood clots from lower extremity into lungs or heart, Inferior Vena Cava Filter (IVCF) can be used in patients with contraindication to anticoagulants. Furthermore, surgical procedures, such as thrombectomy or catheter-directed thrombolysis, can be used to remove or dissolve the clot in order to prevent DVT relapse and the development of PTS.
Warfarin Dosing in Chinese Population
Warfarin has a narrow therapeutic window and large interindividual variability in dosing due to both nongenetic and genetic factors. Nongenetic factors include patient’s clinical characteristics such as age, height, weight, Body Surface Area (BSA), race, and use of interacting concomitant medications, and so forth. The most predominant genetic factors in warfarin dose/response include polymorphisms in cytochrome P450 (CYP) 2C9 and vitamin K epoxide reductase complex 1 (VKORC1). Together, genetic and nongenetic factors may account for about 50% of warfarin dose variability [47]. To improve warfarin dosing, the Clinical Pharmacogenetics Implementation Consortium (CPIC) recommended the use of pharmacogenetic dosing algorithms developed by the International Warfarin Pharmacogenetics Consortium (IWPC) and by Gage, et al. to inform dosing of warfarin using patients’ genetic information [47-49]. Despite the benefits of pharmacogenetic dosing, in majority of cases in China, doctors would monitor patients’ INR and adjust doses accordingly without having genotype information on hand. Figure 3 shows examples of dose adjustments according to INR monitoring in patients receiving warfarin after mechanical heart valve replacement at Huaihe Hospital of Henan University, with the goal of reaching and maintaining within the target INR window of 1.5-3. In all three cases, loading doses of 3.75 mg/day were prescribed for 2 to 4 days after surgery. After anticoagulation effect is realized within a week, doses would be increased, decreased or paused in response to the INR result on that day to maintain within therapeutic window before discharge from hospital.
To promote pharmacogenetic dosing, the Chinese Society of Cardiothoracic and Vascular Anesthesiology published expert advice on the use of genetic polymorphism and antithrombotic drugs in the clinic in 2017, recommending that patients undergo genetic testing when starting warfarin and that doses should be calculated based on CYP2C9*2, *3, and VKORC1-1639 G>A [50]. Furthermore, a number of pharmacogenetic algorithms based on local patients have been developed to achieve better predictive accuracy of stable warfarin doses in the Chinese population [51, 52]. Although pharmacogenetic dosing of warfarin has demonstrated superior efficacy and safety in both Western and Chinese populations, there are ethnic differences in genotype distributions of VKORC1 and CYP2C9, resulting in different dosing requirements [53-56]. In contrast to the expected frequencies for VKORC1-1639 AA, AG, and GG in Whites (16.5%, 46.6%, and 36.9% respectively), at least 80% of the Chinese population have the AA genotype for VKORC1-1639 [57-60]. Also, the allele distribution for CYP2C9*1 in the Chinese population is at least 90%, as compared to a distribution of 70-80% in Whites for the wild type allele [49,58,61]. Furthermore, demographics characteristics, such as lower weight, height, and BSA, result in lower clearance rate and, thus lower dosing requirements, for warfarin in the Chinese population [52].

Figure 3: Antithrombotic medication use among AF patients with CHADS2≧2 and CHA2DS2-VASc ≧2 in Chinese hospitals [30,31,90-105]. The results were based on literature search in PubMed, CNKI (China National Knowledge Infrastructure), and Wanfang Data with the following keywords: atrial fibrillation, anticoagulation, anti-thrombosis, medication, Chinese. The search period was from inception of the database to Dec 2022. This yielded a total of 5 records in PubMed, 121 records in CNKI, and 96 records in Wanfang Data, from which 18 references were selected with applicable data.
Discussions
Warfarin was initially discovered and marketed as a rat poison in 1948. After learning that its overdose could be treated with vitamin K, warfarin was later transitioned into clinical use as a therapeutic anticoagulant [62]. Today, warfarin remains one of the most commonly prescribed drugs to treat and prevent thromboembolic conditions in AF, DVT, PE, and HVR. Due to differences in clinical and genetic factors, warfarin has a large interindividual variability among patients, which requires routine INR monitoring and dose adjustments to achieve and maintain within therapeutic window. In recent years, NOACs, such as dabigatran, rivaroxaban, edoxaban, and apixaban, have been approved and accepted as alternatives to warfarin in many indications. NOACs have several advantages compared to warfarin. Firstly, NOACs have a rapid onset and offset action due to fast absorption and short elimination half-lives, thus erasing the need for heparin bridging in patients undergoing surgery [63]. Secondly, patients taking NOACs do not need to undergo routine INR monitoring to make dose adjustment, since NOACs have fixed daily doses except in special cases, such as impaired renal function [64]. Thirdly, the therapeutic effects of NOACs are not affected by food intake, and therefore patients do not have any dietary restrictions [65]. In China, medical insurance could reimburse NOACs for inpatients, and up to 70% of the cost for outpatient. Many outpatients, such as those with non-valvular AF, need to pay the remaining 30% at their own expense, which remain too high ($1740/year) for those in socioeconomically disadvantaged rural areas [66]. Additionally, clinical guidelines recommend patients with mechanical heart valves or moderate-to-severe mitral stenosis to receive long-term anticoagulation with warfarin [9,23]. According to a study on oral anticoagulant prescription trends covering 189,006 prescriptions of 67 hospitals in 5 major regions of China (Beijing, Shanghai, Hangzhou, Guangzhou, and Chengdu), warfarin prescription accounts for as much as 72% of patients in 2017 [67]. Clearly, warfarin remains an important anticoagulant option in the era of NOACs.
According to our literature review, AF and HVR account for more than 60% of all patients, with DVT/PE accounting for up to 30% among other indications in China (Figure 1). With one of the fastest growing aging populations in the world, China has seen significant increase in the incidence and prevalence of AF over the past 20 years [68]. It is estimated there are at least 10 million AF patients in China, and 62% of the AF cases affected people aged 65 and above [27]. AF is associated with significantly higher risk of major systemic thromboembolism and ischemic stroke compared to healthy population. Therefore, treatment with oral anticoagulant is essential to prevent and treat thromboembolic complications. The 2010 ESC guidelines recommend that patients with CHADS2≧2 should receive oral anticoagulant, while for the new score CHA2DS2-VASc, the 2016 ESC guidelines recommend that men with a score of 1 and women with a score of 2 be preferably treated with oral anticoagulant [29,69]. Our literature review suggests that among AF patients with high stroke risk in Chinese hospitals (CHADS2≧2 and CHA2DS2-VASc ≧2), a large proportion of patients were taking antiplatelets instead of anticoagulants. Our findings are consistent with results from previous studies suggesting of significant underuse of warfarin in Chinese patients with AF [70-72]. This underuse of oral anticoagulants is in contrary to clinical guideline recommendations and may have many reasons. Many physicians in China may be reluctant to prescribe oral anticoagulants in elderly AF patients due to the fear of bleeding events and underestimation of the benefit of oral anticoagulant to reduce the stroke risk. Furthermore, the cost and inconvenience of frequent INR monitoring may be a concern for patients, which may lead to noncompliance and discontinuation of therapy. Antiplatelet treatment is indicated for secondary prevention of coronary events but only modestly reduced stroke in AF patients not receiving anticoagulation [73]. Results from a population-based cohort study using electronic health records from 52,178 high-risk patients with AF (CHA2DS2-VASc ≧2) in Hong Kong suggest that warfarin and NOACs were associated with lower risk of ischemic stroke and all-cause mortality than antiplatelets [34]. Clearly, more education emphasizing on the importance of anticoagulation to prevent stroke is needed among health professionals in China to reverse the current trend.
Apart from AF, the other big indication for warfarin use in China is HVR. Nowadays NOACs have gained more acceptance and are becoming the anticoagulants of choice to treat and prevent thromboembolism in many indications, but guidelines published by the AHA/ACC/HRS and ESC specifically recommend treatment with warfarin instead of NOACs in those with moderate-to-severe mitral stenosis or those who underwent mechanical heart valve replacement [9,23]. This recommendation was based on results of the RE-ALIGN trial comparing dabigatran and warfarin in patients after heart valve replacement, which was stopped prematurely due to an excess of both stroke and bleeding with the dabigatran doses tested [40]. Furthermore, results from the INVICTUS (The Investigation of Rheumatic AF Treatment Using Vitamin K Antagonists, Rivaroxaban or Aspirin Studies) trial indicated that among patients with rheumatic heart disease-associated atrial fibrillation, vitamin K antagonist therapy, such as warfarin, led to a lower composite rate of cardiovascular events or death than rivaroxaban therapy, without a higher rate of bleeding [74]. The current practice in China is for patients undergoing mechanical heart valve replacement is to take warfarin for the long-term, whereas for patients undergoing bioprosthetic valve replacement, warfarin should be taken within 6 months after surgery. Also, warfarin should be taken long-term in patients with atrial fibrillation undergoing bioprosthetic valve replacement. Patients undergoing heart valve replacement are usually hospitalized for 1 to 2 weeks after surgery. Before patients are discharged, nursing staff will educate patients on the proper use of warfarin using a pamphlet handout similar to Table 2, and then patients’ knowledge will be evaluated using a questionnaire similar to Table 3. Any areas lacking in sufficient understanding will be reinforced by the nursing staff.
Warfarin has large inter individual variability in dosing among patients due to genetic (VKORC1, CYP2C9, CYP4F2*3, APOE ε2, ε3, ε4 etc.) and clinical factors (age, concomitant medication, weight, height, BSA, etc.) [75]. To promote pharmacogenetic dosing, the Chinese society of Cardiothoracic and Vascular Anesthesiology has published expert advice on the use of genetic polymorphism and antithrombotic drugs in 2017 and recommended patients to undergo genetic testing of CYP2C9*2, *3, and VKORC1-1639 G>A to inform the dosing of warfarin [50]. With regard to warfarin dosing in the Chinese population, one has to keep in mind that there are ethnic differences in VKORC1 and CYP2C9 genotype distributions between Chinese and Western populations. At least 80% of the Chinese population has the VKORC1-1639 AA genotype, and at least 90% has the CYP2C9*1 allele. Furthermore, differences in body weight and BSA may explain clearance and dosing differences between Chinese and Western populations [52]. Also, it has been reported that Chinese patients, and Asian patients in general, are more sensitive to warfarin anticoagulation, with a higher incidence of major bleeding and intracranial hemorrhages than in Western countries [76,77]. According to the expert consensus published by the Chinese Society of Cardiology and Committee of Cardio-cerebral-Vascular of Gerontological Society of China, most patients who stopped receiving warfarin have INR below 1.5 for the long-term, and those who receive warfarin and have INR above 3.0 should undergo dose reduction or interruption to reduce bleeding risk [78]. Therefore, many physicians consider INR between 1.5 and 3.0 to be a “relative safe window”. Since dosing algorithms based on Western patients may be unsuitable for the Chinese population, algorithms based on local patient populations have been developed to better inform dosing in Chinese patients. Huang, et al. [79] developed a pharmacogenetics-based dosing model using retrospective data from 266 Chinese patients. They then prospectively validated this model in 156 patients needing HVR and found that the pharmacogenetic-based dosing model was able to improve the time to reach stable dosing of warfarin [79]. Despite obvious advantages, in many hospitals in China, an empirical approach to warfarin dosing is used in patients after heart valve replacement surgery, where loading doses would be prescribed for the first few days after initiation, followed by adjustments in response to lab monitoring to help maintain INR within therapeutic window before patient discharge similar to Figure 3. Clearly, more education and promotion of pharmacogenetic dosing is needed among healthcare professionals and patients in China to fully realize its benefits.
Conclusions
Even in the age of NOACs, warfarin remains a commonly prescribed anticoagulant in China due to its affordability and decades long experience of clinical use. In patients with moderate-to-severe mitral stenosis or those who underwent mechanical heart valve replacement, warfarin is the recommended option as per clinical guidelines. In our literature review, we found that contrary to clinical guideline recommendations a large proportion of AF patients with high stroke risk were taking antiplatelets instead of anticoagulants in China. Furthermore, given the large interindividual variability in dose/response, pharmacogenetic dosing approach is helpful to guide dosing in patients initiating warfarin. Nevertheless, an empirical approach consisting of loading doses at the beginning followed by dose adjustments based on INR result of the day is still being used in the majority of Chinese hospitals. To further improve warfarin clinical practice, more education and training is needed among healthcare professionals and patients in China.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding
This work was supported by the research start-up fund for Yellow River Scholar of Henan University.
Data Availability Statement
The data used to support findings of this study are included within the article.
References
- Du X, Guo L, Xia S, Du J, Anderson C, et al. (2021) Atrial fibrillation prevalence, awareness and management in a nationwide survey of adults in China. Heart 28;107(7): 535-54.
- Law Y, Chan YC, Cheng SWK (2018) Epidemiological updates of venous thromboembolism in a Chinese population. Asian J Surg 41(2): 176-182.
- Kannel WB, Benjamin EJ (2008) Status of the epidemiology of atrial fibrillation. Med Clin North Am 92(1): 17-40, ix.
- Hald EM, Rinde LB, Lochen ML, Mathiesen EB, Wilsgaard T, et al. (2018) Atrial Fibrillation and Cause-Specific Risks of Pulmonary Embolism and Ischemic Stroke. J Am Heart Assoc 29;7(3): e006502.
- Silverstein MD, Heit JA, Mohr DN, Petterson TM, O'Fallon WM, et al. (1998) Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med 23;158(6): 585-93.
- Heit JA (2005) Venous thromboembolism: disease burden, outcomes and risk factors. J Thromb Haemost 3(8): 1611-7.
- Wang CC, Lin CL, Wang GJ, Chang CT, Sung FC, et al. (2015) Atrial fibrillation associated with increased risk of venous thromboembolism. A population-based cohort study. Thromb Haemost 113(1): 185-92.
- Wadhera RK, Russell CE, Piazza G (2014) Cardiology patient page. Warfarin versus novel oral anticoagulants: how to choose? Circulation 25;130(22): e191-3.
- January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, et al. (2019) 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients with Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation 9;140(2): e125-e151.
- Tran HA, Gibbs H, Merriman E, Curnow JL, Young L, et al. (2019) New guidelines from the Thrombosis and Haemostasis Society of Australia and New Zealand for the diagnosis and management of venous thromboembolism. Med J Aust 210(5): 227-235.
- Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, et al. (2011) Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 15;365(11): 981-92.
- Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, et al. (2011) Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 8;365(10): 883-91.
- Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, et al. (2009) Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 17;361(12): 1139-51.
- Lopez Lopez JA, Sterne JAC, Thom HHZ, Higgins JPT, Hingorani AD, et al. (2017) Oral anticoagulants for prevention of stroke in atrial fibrillation: systematic review, network meta-analysis, and cost effectiveness analysis. BMJ 28:359: j5058.
- Arwood MJ, Deng J, Drozda K, Pugach O, Nutescu EA, et al. (2017) Anticoagulation endpoints with clinical implementation of warfarin pharmacogenetic dosing in a real-world setting: A proposal for a new pharmacogenetic dosing approach. Clin Pharmacol Ther 101(5): 675-683.
- Weitz JI, Eikelboom JW (2016) Urgent Need to Measure Effects of Direct Oral Anticoagulants. Circulation 19;134(3): 186-8.
- Tripodi A, Marongiu F, Moia M, Palareti G, Pengo V, et al. (2018) The vexed question of whether or not to measure levels of direct oral anticoagulants before surgery or invasive procedures. Intern Emerg Med 13(7): 1029-1036.
- Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, et al. (2013) Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med 28;369(22): 2093-104.
- Zhou H, Nie X, Jiang M, Dong W (2022) Cost-effectiveness of anticoagulants for preventing stroke in patients with non-valvular atrial fibrillation in mainland China. J Clin Pharm Ther 47(4): 523-530.
- Wei H, Cui C, Cui X, Liu Y, Li D (2021) Cost-effectiveness analysis of dabigatran, rivaroxaban and warfarin in the prevention of stroke in patients with atrial fibrillation in China. BMC Health Serv Res 28;21(1): 96.
- Sun KX, Cui B, Cao SS, Huang QX, Xia RY, et al. (2021) Cost-Effectiveness Analysis of Direct Oral Anticoagulants Versus Vitamin K Antagonists for Venous Thromboembolism in China. Front Pharmacol 20:12: 716224.
- Chen M, Li C, Liao P, Cui X, Tian W, et al. (2022) Epidemiology, management, and outcomes of atrial fibrillation among 30 million citizens in Shanghai, China from 2015 to 2020: A medical insurance database study. Lancet Reg Health West Pac 3:23: 100470.
- Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, et al. (2021) 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J 1;42(5): 373-498.
- Chao TF, Liu CJ, Tuan TC, Chen TJ, Hsieh MH, et al. (2018) Lifetime Risks, Projected Numbers, and Adverse Outcomes in Asian Patients with Atrial Fibrillation: A Report from the Taiwan Nationwide AF Cohort Study. Chest 153(2): 453-466.
- Balsam P, Lodzinski P, Gawalko M, Kraj L, Sliwczynski A, et al. (2021) Antithrombotic Management and Long-Term Outcomes of Patients with Atrial Fibrillation. Insights from CRAFT Trial. J Clin Med 10(8): 1780.
- Hu D, Sun Y (2008) Epidemiology, risk factors for stroke, and management of atrial fibrillation in China. J Am Coll Cardiol 2;52(10): 865-8.
- Li C, Wang H, Li M, Qiu X, Wang Q, et al. (2022) Epidemiology of Atrial Fibrillation and Related Myocardial Ischemia or Arrhythmia Events in Chinese Community Population in 2019. Front Cardiovasc Med 4:9: 821960.
- Gao P, Fang Q, Wang JL, Fan JB, Zhu KB, et al. (2013) Causes of insufficient anticoagulation in Chinese patients with non-valvlar atrial fibrillation. Zhonghua Xin Xue Guan Bing Za Zhi 41(11): 931-4.
- Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, et al. (2016) 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur J Cardiothorac Surg 50(5): e1-e88.
- Guo H (2017) Investigational Analysis of Anticoagulation Treatment in Patients with Nonvalvular Atrial Fibrillation. Journal of Practical Medical Techniques 24: 1331-33.
- Li X, Wang Q, Lv Q (2013) Clinical application analysis of anticoagulants in patients with non-valvular atrial fibrillation. Chinese Journal of Clinical Pharmacy 22: 163-65.
- Vallakati A, Lewis WR (2016) Underuse of anticoagulation in patients with atrial fibrillation. Postgrad Med 128(2): 191-200.
- Wong CW (2016) Anticoagulation for stroke prevention in elderly patients with non-valvular atrial fibrillation: what are the obstacles?. Hong Kong Med J 22(6): 608-15.
- Li X, Pathadka S, Man KKC, Ng VWS, Siu CW, et al. (2020) Comparative Outcomes Between Direct Oral Anticoagulants, Warfarin, and Antiplatelet Monotherapy Among Chinese Patients with Atrial Fibrillation: A Population-Based Cohort Study. Drug Saf 43(10): 1023-1033.
- Han C, Li D (2018) Strategy of anticoagulation therapy during pregnancy in patients with mechanical heart valve. Chin J Clin Thorac Cardiov Surg 25: 83-89.
- Wang Z, Hu S (2020) Interpretation of report on cardiovascular health and diseases in China. Chin J Cardiovasc Med 25: 401-410.
- Zhu Z, Zhang H, Jiao Y, Meng X (2018) Research progress of anticoagulant therapy in patients with mechanical aortic valve replacement under the context of "Internet +". China Medicine 13: 1902-1905.
- Mair H, Sachweh J, Sodian R, Brenner P, Schmoeckel M, et al. (2012) Long-term self-management of anticoagulation therapy after mechanical heart valve replacement in outside trial conditions. Interact Cardiovasc Thorac Surg 14(3): 253-257.
- Becker RC, Eisenberg P, Turpie AG (2001) Pathobiologic features and prevention of thrombotic complications associated with prosthetic heart valves: fundamental principles and the contribution of platelets and thrombin. Am Heart J 141(6): 1025-1037.
- Eikelboom JW, Connolly SJ, Brueckmann M, Granger CB, Kappetein AP, et al. (2013) Dabigatran versus warfarin in patients with mechanical heart valves. N Engl J Med 369(13): 1206-1214.
- Guyatt GH, Akl EA, Crowther M, Schunemann HJ, Gutterman DD, et al. (2012) Introduction to the ninth edition: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl): 48S-52S.
- CMA (2017) Chinese Medical Association Vascular Surgery Group: Diagnostic and Treatment Guidelines for Deep Vein Thrombosis. Chinese J Vascu Surg (Electronic Version) 9: 250-257.
- Tick LW, Kramer MH, Rosendaal FR, Faber WR, Doggen CJ, et al. (2008) Risk factors for post-thrombotic syndrome in patients with a first deep venous thrombosis. J Thromb Haemost 6(12): 2075-2081.
- Kahn SR, Shrier I, Julian JA, Ducruet T, Arsenault L, et al. (2008) Determinants and time course of the postthrombotic syndrome after acute deep venous thrombosis. Ann Intern Med 149(10): 698-707.
- Lu J, Wu J, Yang J (2019) Anticoagulation Treatment for Lower Extremity Deep Vein Thrombosis. Cardiovascular Disease Electronic Journal of Integrated Traditional Chinese and Western Medicine 7: 13-20.
- Hu D, Sun Y (2005) Standard Prevention and Treatment for Thromboembolic Diseases--Learnings from the Latest ACCP Thrombolysis and Antithrombotic Guidelines. Clinical Focus 20: 841-843.
- Johnson JA, Gong L, Whirl Carrillo M, Gage BF, Scott SA, et al. (2011) Clinical Pharmacogenetics Implementation C. Clinical Pharmacogenetics Implementation Consortium Guidelines for CYP2C9 and VKORC1 genotypes and warfarin dosing. Clin Pharmacol Ther 90(4): 625-629.
- IWPC, Klein TE, Altman RB, Eriksson N, Gage BF, Kimmel SE, et al. (2009) Estimation of the warfarin dose with clinical and pharmacogenetic data. N Engl J Med 360(8): 753-764.
- Gage BF, Eby C, Johnson JA, Deych E, Rieder MJ, et al. (20058) Use of pharmacogenetic and clinical factors to predict the therapeutic dose of warfarin. Clin Pharmacol Ther 84(3): 326-331.
- CSCTVA (2017) Chinese Society of Cardiothoracic and Vascular Anesthesiology: Expert Advice on the Use of Genetic Polymorphism and Antithrombotic Drugs in the Clinic. Fujian Medical Journal 39: 9-19.
- Xie C, Xue L, Zhang Y, Zhu J, Zhou L, et al. (2020) Comparison of the prediction performance of different warfarin dosing algorithms based on Chinese patients. Pharmacogenomics 21(1): 23-32.
- Deng J, Wang Y, An X (2023) Comparison of Maintenance Dose Predictions by Warfarin Dosing Algorithms Based on Chinese and Western Patients. J Clin Pharmacol 63(5): 569-582.
- Pirmohamed M, Burnside G, Eriksson N, Jorgensen AL, Toh CH, et al. (2013) A randomized trial of genotype-guided dosing of warfarin. N Engl J Med 369(24): 2294-2303.
- Gage BF, Bass AR, Lin H, Woller SC, Stevens SM, et al. (2017) Effect of Genotype-Guided Warfarin Dosing on Clinical Events and Anticoagulation Control Among Patients Undergoing Hip or Knee Arthroplasty: The GIFT Randomized Clinical Trial. JAMA 318(12): 1115-1124.
- Guo C, Kuang Y, Zhou H, Yuan H, Pei Q, et al. (2020) Genotype-Guided Dosing of Warfarin in Chinese Adults: A Multicenter Randomized Clinical Trial. Circ Genom Precis Med 13(4): e002602.
- Zhu Y, Xu C, Liu J (2020) Randomized controlled trial of genotype-guided warfarin anticoagulation in Chinese elderly patients with nonvalvular atrial fibrillation. J Clin Pharm Ther 45(6): 1466-1473.
- Zhao L, Chen C, Li B, Dong L, Guo Y, et al. (2014) Verification of pharmacogenetics-based warfarin dosing algorithms in Han-Chinese patients undertaking mechanic heart valve replacement. PLoS One 9(4): e94573.
- Xia X, Huang N, Li B, Li Y, Zou L, et al. (2022) To establish a model for the prediction of initial standard and maintenance doses of warfarin for the Han Chinese population based on gene polymorphism: a multicenter study. Eur J Clin Pharmacol 78(1): 43-51.
- Watzka M, Nebel A, El Mokhtari NE, Ivandic B, Muller J, et al. (2007) Functional promoter polymorphism in the VKORC1 gene is no major genetic determinant for coronary heart disease in Northern Germans. Thromb Haemost 97(6): 998-1002.
- Xu Q, Xu B, Zhang Y, Yang J, Gao L, et al. (2012) Estimation of the warfarin dose with a pharmacogenetic refinement algorithm in Chinese patients mainly under low-intensity warfarin anticoagulation. Thromb Haemost 108(6): 1132-1140.
- Wu AH, Wang P, Smith A, Haller C, Drake K, et al. (2008) Dosing algorithm for warfarin using CYP2C9 and VKORC1 genotyping from a multi-ethnic population: comparison with other equations. Pharmacogenomics 9(2): 169-178.
- Lim GB (2017) Milestone 2: Warfarin: from rat poison to clinical use. Nat Rev Cardiol.
- Bauer KA (2013) Pros and cons of new oral anticoagulants. Hematology Am Soc Hematol Educ Program 2013: 464-470.
- Kubitza D, Becka M, Voith B, Zuehlsdorf M, Wensing G, et al. (2005) Safety, pharmacodynamics, and pharmacokinetics of single doses of BAY 59-7939, an oral, direct factor Xa inhibitor. Clin Pharmacol Ther 78(4): 412-421.
- Hoffman R, Brenner B (2012) The promise of novel direct oral anticoagulants. Best Pract Res Clin Haematol 25(3): 351-360.
- Liu T, Yang HL, Gu L, Hui J, Omorogieva O, et al. (2020) Current status and factors influencing oral anticoagulant therapy among patients with non-valvular atrial fibrillation in Jiangsu province, China: a multi-center, cross-sectional study. BMC Cardiovasc Disord 20(1): 22.
- Yu Z, Yu L, Shan C (2020) Trends of ambulatory oral anticoagulant prescription in five major cities of China, 2012-2017. BMC Health Serv Res 20(1): 209.
- Song J (2022) The Chinese burden of atrial fibrillation review of atrial fibrillation studies in China. Ann Noninvasive Electrocardiol 27(6): e12957.
- European Heart Rhythm A, European Association for Cardio-Thoracic Surgery, Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, et al. (2010) Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J 31(19): 2369-2429.
- Wang C, Yang Z, Wang C, Wang Y, Zhao X, et al. (2014) Significant underuse of warfarin in patients with nonvalvular atrial fibrillation: results from the China national stroke registry. J Stroke Cerebrovasc Dis 23(5): 1157-1163.
- Guo J, Guan T, Fan S, Chao B, Wang L, et al. (2018) Underuse of Oral Anticoagulants in Patients with Ischemic Stroke and Atrial Fibrillation in China. Am J Cardiol 122(12): 2055-2061.
- Zheng HJ, Ouyang SK, Zhao Y, Lu K, Luo SX, et al. (2017) The use status of anticoagulation drugs for inpatients with nonvalvular atrial fibrillation in Southwest China. Int J Gen Med 10: 69-77.
- Benz AP, Johansson I, Dewilde WJM, Lopes RD, Mehran R, et al. (2022) Antiplatelet therapy in patients with atrial fibrillation: a systematic review and meta-analysis of randomized trials. Eur Heart J Cardiovasc Pharmacother 8: 648-659.
- Connolly SJ, Karthikeyan G, Ntsekhe M, Haileamlak A, El Sayed A, et al. (2022) Investigators I. Rivaroxaban in Rheumatic Heart Disease-Associated Atrial Fibrillation. N Engl J Med 387: 978-988.
- Asiimwe IG, Zhang EJ, Osanlou R, Jorgensen AL, Pirmohamed M. (2021) Warfarin dosing algorithms: A systematic review. Br J Clin Pharmacol 87(4): 1717-1729.
- Suzuki S, Yamashita T, Kato T, Fujino T, Sagara K, et al. (2007) Incidence of major bleeding complication of warfarin therapy in Japanese patients with atrial fibrillation. Circ J 71(5): 761-765.
- Dong L, Shi YK, Tian ZP, Ma JY, Wang X, et al. (2003) [Low intensity anticoagulation therapy after mechanical heart valve replacement]. Zhonghua Wai Ke Za Zhi 41: 250-252.
- (2013) CSC. Chinese Society of Cardiology, Committee of Cardio-cerebral-Vascular of Gerontological Society of China: Expert Consensus for Anticoagulation using Warfarin. Chin J Intern Med 52: 76-82.
- Huang SW, Chen HS, Wang XQ, Huang L, Xu DL, et al. (2009) Validation of VKORC1 and CYP2C9 genotypes on interindividual warfarin maintenance dose: a prospective study in Chinese patients. Pharmacogenet Genomics 19: 226-234.
- Chen W, Wu L, Liu X, Shen Y, Liang Y, et al. (2017) Warfarin dose requirements with different genotypes of CYP2C9 and VKORC1 for patients with atrial fibrillation and valve replacement. Int J Clin Pharmacol Ther 55(2): 126-132.
- Dong J, Shi GH, Lu M, Huang S, Liu YH, et al. (2019) Evaluation of the predictive performance of Bayesian dosing for warfarin in Chinese patients. Pharmacogenomics 20(3): 167-177.
- Jiang J, Ji N, Lan J, Ge X, Du X (2018) Clinical verification of Lou type warfarin pharmacokinetic dosing algorithms equation. Mol Med Rep 17: 6144-6149.
- Lee MT, Chen CH, Chou CH, Lu LS, Chuang HP, et al. (2009) Genetic determinants of warfarin dosing in the Han-Chinese population. Pharmacogenomics 10(12): 1905-1913.
- Li C, Dai D, Hu G, Pu C, Cao Y, (2016) [Establishment and evaluation of a warfarin-dosing algorithm in Chinese Han population]. Zhonghua Yi Xue Za Zhi 96(10): 776-780.
- Wen MS, Chang KC, Lee TH, Chen YF, Hung KC, et al. (2017) Pharmacogenetic dosing of warfarin in the Han-Chinese population: a randomized trial. Pharmacogenomics 18: 245-253.
- Wen MS, Lee M, Chen JJ, Chuang HP, Lu LS, et al. (2008) Prospective study of warfarin dosage requirements based on CYP2C9 and VKORC1 genotypes. Clin Pharmacol Ther 84: 83-9.
- Ye C, Jin H, Zhang R, Sun Y, Wang Z, et al. (2014) Variability of warfarin dose response associated with CYP2C9 and VKORC1 gene polymorphisms in Chinese patients. J Int Med Res 42(1): 67-76.
- You JH, Wong RS, Waye MM, Mu Y, Lim CK, et al. (2011) Warfarin dosing algorithm using clinical, demographic and pharmacogenetic data from Chinese patients. J Thromb Thrombolysis 31: 113-118.
- Zeng WT, Xu Q, Li CH, Chen WY, Sun XT, et al. (2016) Influence of genetic polymorphisms in cytochrome P450 oxidoreductase on the variability in stable warfarin maintenance dose in Han Chinese. Eur J Clin Pharmacol 72(11): 1327-1334.
- Bai Y, Wei Z, Yang J (2017) The Treatment and Influencing Factors among Hospitalized Patients with Non-valvular Atrial Fibrillation. Journal of Clinic Nursing's Practicality 2: 21-24.
- Chang SS, Dong JZ, Ma CS, Du X, Wu JH, et al. (2016) Current Status and Time Trends of Oral Anticoagulation Use Among Chinese Patients With Nonvalvular Atrial Fibrillation: The Chinese Atrial Fibrillation Registry Study. Stroke 47: 1803-1810.
- Chen A, Li D, Pan M, Huang X, Yi Y, et al. (2018) Anti-thrombotic Treatment Analysis of Hospitalized Patients with Atrial Fibrillation at Our Hospital. Strait Pharmaceutical Journal 30: 247-249.
- Du X, Chen C, Qin Y, Sun H, Liu L, et al. (2015) Warfarin Application Research and Analysis in Patients with Non-valvular Atrial Fibrillation. Chinese Pharmaceutical Journal 50: 2000-2003.
- Li H, Lan G (2019) Analysis on Anticoagulation Therapy in Elderly Patients with non-valvular Atrial Fibrillation in the West Area of Chengdu. Journal of Kunming Medical University 40: 121-125.
- Lin H (2011) Anticoagulant Medication Use in 169 Patients with Nonvalvular Atril Fibrillation. Chinese Journal of Rural Medicine and Pharmacy 18: 26-27.
- Qian J, Chen J, Wang L, Li J, Zou Y, et al. (2018) Investigation on antithrombotic therapy of hospitalized patients with coronary heart disease complicated with persistent atrial fibrillation. Chin J Cardiac Arrhyth 22: 215-221.
- Sun R, Fan Z, Feng Y, Hao Y (2015) Study of Standardized Anticoagulant Therapy in Elderly Patient with Atrial Fibrillation. Medical Innovation of China 12: 107-110.
- Wu Y, Peng Y, Rong P, Li M, Zhou B (2015) Current Application of Warfarin in 179 Hospitalized Patients with Atrial Fibrillation. Herald of Medicine 34: 1165-1169.
- Xiao D, Hu J (2017) Clinical application of anticoagulant in patients with non-valvular atrial fibrillation. World Clinicall Drugs 38: 544-549.
- Xin J (2019) Warfarin Anticoagulation Treatment in Patients with Nonvalvular Atrial Fibrillation. Shanxi Medical Journal 48: 1200-1202.
- Xiong L, Luo C, Liu Y, Wu Y, Wen Y (2001) Survey of the Anti-Thrombosis Therapy for Patients with Non-Valvular Atrial Fibrillation in the Northwest of Sichuan. World Latest Medicine Information 15: 37-78.
- Yang K, Xu Y, Zhou Z, He W (2017) Anticoagulation Treatment and Influencing Factors in Patients with Nonvalvular Atrial Fibrillation. Chinese Rural Medicine 24: 56-57.
- Yin Y, Gao Y (2016) Related research on the treatment of inpatients with atrial fibrillation in primary hospital. Modern Medicine Journal of China 18: 20-24.
- Zhao H, Shen B, Jiang Y, Zhao F, Lu C, et al. (2013) Analysis on antithrombotic therapy for 116 cases of patients with persistent atrial fibrillation. Clinical Journal of Medical Officers 41: 1227-1236.
- Zheng L, Chen H (2012) investigation of anticoagulation therapy for elderly patients with high risk of nonvalvular atrial fibrillation. Chin J Clinicians (Electronic Edition) 6: 874-878.





 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.