Short Communication 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Elimination of Wound Healing Lag Time by Novel Alternative Pathways
*Corresponding author:Sufan Chien, Department of Surgery University of Louisville School of Medicine, Louisville, KY 40292, and Noveratech LLC of Louisville, Kentucky, USA.
Received: February 19, 2024; Published: February 28, 2024
DOI: 10.34297/AJBSR.2024.21.002875
Introduction
The traditional wound healing process can be divided into four distinct but overlapping phases, hemostasis, inflammation, proliferation, and remodeling, requiring a 3–6-day lag time during which no new tissue is generated. Is it possible to change this dogma to shorten the healing time? No one has ever been able to do it.
For the first time, our group has discovered certain conditions where this lag time can be significantly shortened or eliminated, resulting in a substantially enhanced wound healing process. When we apply our nanoliposome-encapsulated Mg-ATP (ATP-vesicles) to rabbit ear wounds, which have almost no skin contraction, new tissue growth appears in the wound cavity within 24 hours. The growth continues and covers the defects within a few days. This process is totally different from the traditional wound healing process where fibrin, platelets, and red blood cells form an early provisional matrix that is gradually replaced by granulation tissue after 3–6 days of lag time. All control dressings, including the only FDA-approved prescription growth factor, Regranex, do not have similar effects. This result is very dramatic and sometimes criticized for being “too good to be true” with possible unexpected consequence. However, it has been proven in more than 400 rabbits (over 3000 wounds) with the longest survived more than 2 years without any complications.
The mechanisms behind such a dramatic effect are not entirely clear at this time. Our results have indicate multiple pathways involved. However, at this time, we have only performed some pathways but not all due to their complex nature, which will require many years to make them clear (Figure 1).
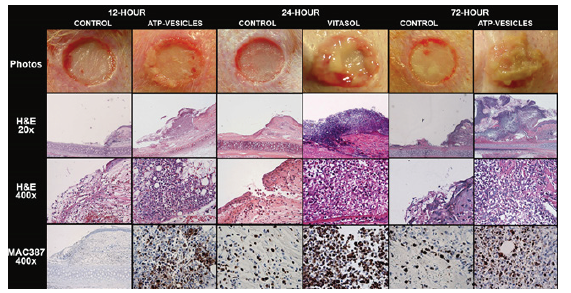
Figure 1: Histology and immunohistochemistry stains at 12, 24, and 72 hours after dressing application. Wounds treated by ATP-vesicles have new growth starts at 12 hours. It keeps growing thereafter. The newly grown tissue is filled with cells instead of scab which will be gradually replaced by granulation tissue.
i. Extremely early and rapid macrophage accumulationcurred in 12-month diabetic animals. Further IHC tests show strong expression of M2 macrophage markers, such as CD80, CD163, and IL13R.
ii. Direct collagen generation by macrophages. A simple massive macrophage accumulation is not adequate for extracellular matrix formation because the initial loose cell mass can easily be dislodged or removed. However, our newly generated tissues are solid, and analyses have indicated direct macrophage collagen production to form extracellular matrix, a key to sustainable healing. This is further confirmed by Van Gieson collagen staining. Macrophage studies have been ongoing for more than a century, but these cells remain a mystery in many aspects. Because direct macrophage collagen production has always been under debate in the wound care community, we have shown such result both in vivo and in vitro when ATP-vesicles are used [1].
iii. Accumulation of very early platelets and platelets microparticles. Platelets are involved at all the stages of wound healing cascade. Platelets accumulate, adhere, aggregate and form a procoagulant surface favoring thrombin generation and fibrin formation in very early wounds. Platelet-Derived Growth Factor (PDGF) is released by activated platelets to recruit inflammatory cells toward the wound bed. Platelets also have effects on promoting granulation tissue formation and angiogenesis. They contain large secretable pools of biologically active proteins, while newly synthesized active metabolites are also released. The binding of secreted proteins within a developing fibrin mesh or to the extracellular matrix can create chemotactic gradients favoring the recruitment of stem cells, stimulating cell migration and differentiation, and promoting repair. Although our knowledge is still not complete, the role of platelets is clearly seen in all wound healing processes. When ATP-vesicles are used, the platelet accumulation is even seen earlier than macrophage accumulation [2].
iv. No hypertrophic scar formation. In traditional wound healing process, the hemostasis phase starts immediately after injury and the coagulation cascade leads to platelet aggregation and clot formation in order to limit blood loss. A hypertrophic scar is a thick raised scar that’s an abnormal response to wound healing. They more commonly occur in taut skin areas following skin trauma, burns or surgical incisions. The blood components and platelets come in contact with exposed collagen and other extracellular matrix components, resulting in the release of clotting factors from the platelets and the formation of a blood clot, composed of fibronectin, fibrin, vitronectin and thrombospondin. Despite extremely rapid tissue growth when ATP-vesicles are used, histology study shows a solid cell mass but finally healed smooth without any hypertrophic scar formation.
There are other specific process when the ATP-vesicles are used. However, we have not done extensive studies regarding their mechanisma at this time. The following are other related processes still under investigation.
a. Early vascular progenitor cells accumulation along with rapid neovascularization.
b. Highly expressions of circulating bone marrow progenitor cells.
c. Rapid cytokines, chemokines, and growth factors accumulation.
d. Expressions of chromatin remodeling enzymes.
e. Specific microRNA upregulation.
Due to extremely complex mechanisms in wound healing, more than 100 factors could be involved. Tissue ischemia is the main cause that hinders healing. At the same time, the patterns of DFUs (Diabetic Foot Ulcers) seen in Western countries have changed in the last two decades, with the neuro ischemic ulcer now replacing the previously predominant neuropathic type in many clinics. Simply increasing the wound oxygen with hyperbaric oxygen therapy has not shown consistent results, because oxygen alone is inadequate to reverse ischemic damage. The most critical consequence of ischemia is a decrease in cellular energy supply. Energy is required in every aspect of the wound-healing process: Synthesis of a protein by linking its individual amino acids through peptide bonds requires a significant input of chemical energy. Most collagen is synthesized by fibroblasts, but fibroblasts cannot proliferate or synthesize collagen under ischemic conditions. Cell migration and proliferation, membrane transport, and growth factor production all consume energy. Small-scale clinical trials of growth factors such as βFGF have shown effectiveness in non-ischemic wounds, but their effects disappear in hypoxic dermal ulcer models. Providing energy such as Mg-ATP directly to the wound tissue doest not work because ATP and its analogs are intrinsically cell impermeable. We encapsulate Mg-ATP in nanoliposomes to achieve this goal. However, the multiple related mechanisms make the study complex. We view our results are still preliminary, and many more studies are required down the road.
Funding
This study was supported by the following grants: National Institutes of Health grants: DK74566, AR52984, HL64186, HL114235, GM106639, DK104625, DK105692, DK133065, and OD021317 from NIH, and KSTC-184-512-12-138, KSTC-184-512-14-174 from Kentucky Science and Technology Cooperation.
Acknowledgement
None.
None.
None.
References
- Sarojini H, Bajorek A, Wan R, Wang J, Zhang Q, et al. (2021) Enhanced skin incisional wound healing with intracellular ATP delivery via macrophage proliferation and direct collagen production. Front Pharmacol 12: 594586.
- Mo Y, Sarojini H, Wan R, Zhang Q, Wang J, et al. (2020) Intracellular ATP Delivery Causes Rapid Tissue Regeneration via Upregulation of Cytokines, Chemokines, and Stem Cells. Front Pharmacol 10: 1502.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.