Mini Review 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Impact of Diabetes, Depression in Dementia
*Corresponding author: Arubala P Reddy, Department of Nutritional Sciences, College of Human Sciences, Texas Tech University, 1301 Akron Avenue Lubbock, TX 79409,USA.
Received: January 08, 2024; Published: January 12, 2024
DOI: 10.34297/AJBSR.2024.21.002809
Abstract
With increasing aging population, dementia is a major healthy concern in US and worldwide. Increasing evidence also suggests that coexistence of diabetes and depression exacerbate the high prevalence of dementia in elderly. Recent advanced medical care, diagnostic features, timely provided medicines and caregiving facilities, lifespan is increased in elderly individuals with diabetes and depression. Our mini-review discusses the latest developments in depression, diabetes, and dementia research. We also covered interlinks between depression, diabetes, and dementia in relation to gender, age, and lifestyle risk factors. We also briefly discussed, pharmacological and lifestyle intervention to reduce diabetes, depression, and dementia.
Keywords: Diabetes, Depression, Dementia, Lifestyle Factors, Aging Population, Lifespan
Abbreviations: 5-HT: Serotonin; AD:Alzheimer’s disease; ADRD: Alzheimer’s Disease-Related Dementias; Aβ: Amyloid-β ; DM: Diabetes Mellitus; MDD: Major Depressive Disorder; P-Tau: Phosphorylated tau; T2D : Type 2 Diabetes
Opinion
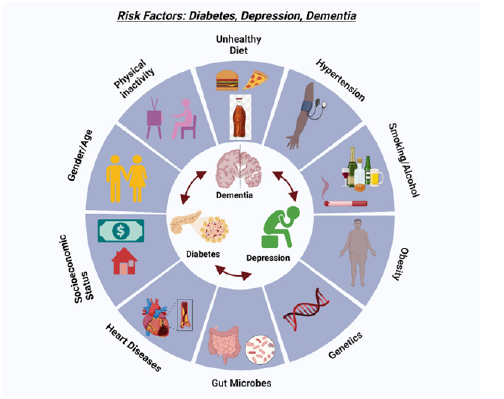
Dementia is a growing concern in modern society. Dementia does not represent a distinct pathological entity; it serves as a comprehensive designation for cognitive decline. Alzheimer’s Disease (AD) stands out as the predominant manifestation within the spectrum of dementia [1]. Dementia is also linked to Alzheimer’s Disease-Related Dementias (ADRD) in elderly population. While dementia predominantly affects the elderly population [2], it is crucial to emphasize that it does not form an integral aspect of the usual aging trajectory. Dementia is the result of various alterations at the cellular level, including synaptic depletion, dysfunctional mitochondria, the emergence of amyloid-β (Aβ) plaques, and the presence of actively phosphorylated tau in the brain [3]. Amyloid beta and Phosphorylated Tau (P-Tau) accumulation are hallmarks of AD. In conjunction with the interaction of these proteins, numerous other factors, including age, gender, genetics, comorbidities such as depression, diabetes, hypertension, race/ethnicity, lifestyle, and environmental factors, contribute to the onset of dementia [4].
According to the Alzheimer’s Association (2023), AD affects over 6 million individuals across various age groups in the United States. In 2023, approximately 6.7 million Americans aged 65 and above were struggling with AD. Comorbidities such as chronic diabetes, depression, hypertension, and obesity are closely associated with dementia. Diabetes is a prolonged health condition characterized by a protracted impairment in the utilization of blood glucose within the body; the regulation of blood glucose is governed by insulin, a hypoglycemic hormone [5]. Historically, the emphasis in diabetes management has centered on addressing conventional complications such as diabetic retinopathy, peripheral neuropathy, nephropathy, and cardiovascular diseases [6]. Nevertheless, recent reports have increasingly indicated that prolonged diabetes may impact cognitive functions [6]. Considerable epidemiological evidence suggests a robust correlation between T2DM and cognitive impairment, attributed to the inadequacy of glucose absorption in neurons for energy production [7-9].
Depression, specifically Major Depressive Disorder (MDD), is a prevalent and significant medical condition that adversely impacts one’s emotional state, cognitive processes, and behavioral patterns. Depression is one of the causative factors of dementia. The manifestations of depression vary among individuals, and there exist different degrees of severity in depressive states. Studies, both retrospective and prospective, have demonstrated that depression, whether accompanied by cognitive features or presenting as depressive symptoms without explicit depression, is associated with an increased susceptibility to dementia [10-12]. Increasing evidence indicates the complexity of the association, as epidemiological studies suggest that depression may function as an independent risk factor for dementia. Crucially, the timing of depression is noteworthy, with earlier-life depression or depressive symptoms being linked to a more than twofold increase in the risk of dementia (Figure 1).
Gender Differences in Diabetes, Depression, and Dementia Risk
Gender differences are increasingly recognized as a critical factor in clinical variation, potentially influencing the transition from diabetes and depression to dementia and/or AD/ADRD. Females are statistically twice as prone to developing overweight or obesity conditions compared to males [13]. Which might increase the risk of diabetes in women. Females have approximately a twofold higher incidence of being diagnosed with depression and dementia compared to males. A suggested theory for the increased risk of ADRD in women is changes in internal estrogen production related to menopause [14]. Additionally, the average life expectancy is higher in females than in males. Hormonal influences are significant in the development of these chronic conditions.
Diabetes and Dementia
Because of the heightened risk of late-onset AD associated with diabetes mellitus, impaired mitochondrial energy metabolism and oxidative stress, researchers referred AD as Type 3 diabetes mellitus [15-17]. The link between prolonged T2DM can contribute to various factors. Diabetes Mellitus (DM) is linked to notable cognitive deficits and an elevated risk of dementia, specifically vascular dementia, and AD, with respective elevations in risk estimated at 100%-150% and 50%-100% [18]. Amyloid beta and phosphorylated tau are identified as the primary pathogenic factor in the development of AD [1]. Advanced glycation end products contribute to its elimination, while an insulin-degrading enzyme, with which it competes with insulin, facilitates its deterioration.
The secretion of Aβ and the promotion of brain inflammation are triggered by insulin [19]. Another factor involves the impact of diabetes on heart health, which is interconnected with brain health. Heart disease and high blood pressure, (in other words hypertension), often associated with diabetes, can contribute to strokes, a known precursor to dementia. Research has demonstrated impaired insulin signaling in the brain, leading to the tau protein’s heightened phosphorylation (hyperphosphorylation). This hyperphosphorylation is ultimately causing the accumulation of neurofibrillary tangles [20]. Insulin depletion in both T1DM and T2DM influences brain health, particularly impacting memory functions [20]. Beyond its metabolic role, insulin appears to play a crucial role in cognitive processes, and its deficiency may contribute to cognitive impairments, affecting memory functions in individuals with diabetes.
Depression and Dementia
When considering depression as either a cause or a risk factor for dementia, it is essential to recognize the substantial overlap in symptoms. Individuals experiencing depression often report memory issues and exhibit measurable cognitive deficits on tests [21]. Common indicators of major depression include a predominantly low mood. However, it may manifest as irritability, anger, or anxiety, and disruptions in biological rhythms, affecting sleep, appetite, and energy levels, are frequently observed. Additionally, individuals experiencing major depression may exhibit negativity, feelings of hopelessness, or even nihilistic perspectives [22]. These alterations in lifestyle can lead to dementia. Research findings indicate that when depression occurs in individuals already experiencing preexisting dementia, it contributes to an expedited cognitive decline [23]. Neurotransmitter alterations might potentially be underlying mechanisms that could be linked to both dementia and depression. Depression is commonly characterized by decreased levels of brain Serotonin (5-HT) and norepinephrine, forming the foundation for the neuropharmacological treatment of depression [24]. Increasing evidence also suggest that serotonin levels are reduced in women compared to men further supporting high prevalence of depression and dementia/AD in women [23,24].
Conclusion
Current evidence suggests a complex and significant association between diabetes and depression are strongly linked to in the pathogenesis of AD and ADRD. The coexistence of both diabetes and depression may exacerbate the vulnerability to developing dementia. Additional research is essential to elucidate the intricate mechanisms driving the interconnection between diabetes, depression, and dementia. This understanding will be crucial in creating specific interventions aimed at reducing the dementia risk in individuals affected by both diabetes and depression. The adoption of lifestyle modifications is vital for disease prevention. Diabetes and depression are a precursor to chronic health conditions, significantly reducing both life expectancy and quality of life. Therefore, this triad of conditions necessitates an integrated clinical approach for early detection and intervention, aiming to attenuate the compounded risk and progression of dementia in individuals with diabetes and depression.
Conflict of Interest statement
Authors declare that they do not have any conflict of interest.
Funding
The presented research was supported by Alzheimer’s Association through a SAGA grant, Garrison Family Foundation Grant, and NIH grants AG063162 and AG071560 (to APR).
Acknowledgements
Authors sincerely thank all the Reddy Lab or 3D Lab members for their support and constructive criticism to improve the manuscript.
References
- Sehar U, Rawat P, Reddy AP, Kopel J, Reddy PH (2022) Amyloid beta in aging and Alzheimer’s disease. International journal of molecular sciences 23(21): 12924.
- Rawat, P, Sehar U, Bisht J, Selman A, Culberson J, et al. (2022) Phosphorylated tau in Alzheimer’s disease and other tauopathies. International Journal of Molecular Sciences 23(21): 12841.
- Oliver D, PH Reddy (2019) Molecular basis of Alzheimer’s disease: focus on mitochondria. Journal of Alzheimer's Disease 72: 95-116.
- Rawat P, et al. (2023) Alzheimer's Disease and Alzheimer’s Disease-Related Dementias in Hispanics: Identifying Influential Factors and Supporting Caregivers. Ageing Research Reviews 102178.
- Rawat P, Sehar U, Bisht J, Reddy PH (2023) Support Provided by Caregivers for Community-Dwelling Diabetic Hispanic Adults with Intellectual Disabilities and Comorbid Conditions. International Journal of Molecular Sciences 24(4): 3848.
- Pugazhenthi S, Qin L, Reddy PH (2017) Common neurodegenerative pathways in obesity, diabetes, and Alzheimer's disease. Biochimica Et Biophysica Acta (BBA)-molecular basis of disease 1863(5): 1037-1045.
- Yang Y, Song W (2013) Molecular links between Alzheimer’s disease and diabetes mellitus. Neuroscience 250: 140-150.
- Cukierman T, Gerstein H, Williamson J (2005) Cognitive decline, and dementia in diabetes-systematic overview of prospective observational studies. Diabetologia 48: 2460-2469.
- Brands AM (2005) The effects of type 1 diabetes on cognitive performance: a meta-analysis. Diabetes care 28(3): 726-735.
- Chen R (2008) Severity of depression and risk for subsequent dementia: cohort studies in China and the UK. The British Journal of Psychiatry 193(5): 373-377.
- Butters MA (2008) Pathways linking late-life depression to persistent cognitive impairment and dementia. Dialogues in clinical neuroscience 10(3): 345-357.
- Fernández Martínez M (2008) Risk factors for dementia in the epidemiological study of Munguialde County (Basque Country-Spain). BMC neurology 8(1): 1-8.
- Selman A (2022) The role of obesity and diabetes in dementia. International journal of molecular sciences 23(16): 9267.
- Royse SK (2021) Differences in Alzheimer’s disease and related dementias pathology among African American and Hispanic women: A qualitative literature review of biomarker studies. Frontiers in systems neuroscience 15: 685957.
- Cai Z, Yan Y, Wang Y (2013) Minocycline alleviates beta-amyloid protein and tau pathology via restraining neuroinflammation induced by diabetic metabolic disorder. Clinical interventions in aging 1089-1095.
- De la Monte SM, Wands JR(2008) Alzheimer's disease is type 3 diabetes-evidence reviewed. Journal of diabetes science and technology 2(6): 1101-1113.
- Kandimalla R, Thirumala V, Reddy PH (2017) Is Alzheimer's disease a type 3 diabetes? A critical appraisal. Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease 1863(5): 1078-1089.
- Agrawal M, Agrawal AK (2022) Pathophysiological association between diabetes mellitus and Alzheimer's disease. Cureus 14(9).
- Pavlović DM, Pavlović AM (2008) Dementia and diabetes mellitus. Srpski arhiv za celokupno lekarstvo 136(3-4): 170-175.
- Hobday AL, Parmar MS, Hobday A (2021) The link between diabetes mellitus and tau hyperphosphorylation: implications for risk of Alzheimer's disease. Cureus 13(9).
- Thomas AJ, O'Brien JT (2008) Depression, and cognition in older adults. Current opinion in psychiatry 21(1): 8-13.
- Kitching D (2015) Depression in dementia. Australian prescriber 38(6): 209.
- Rapp MA (2011) Cognitive decline in patients with dementia as a function of depression. The American Journal of Geriatric Psychiatry 19(4): 357-363.
- Chen Z, Skolnick P (2007) Triple uptake inhibitors: therapeutic potential in depression and beyond. Expert opinion on investigational drugs 16(9): 1365-1377.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.