Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Intramural Recto-Sigmoid Wall Abscess Following Simultaneous Kidney and Pancreas Transplant: A Case Report
*Corresponding author: Atta M Nawabi, The University of Kansas Medical Center, Department of Surgery, 3901 Rainbow Boulevard, Kansas City, KS 66160, USA.
Received: December 26, 2023; Published: January 10, 2023
DOI: 10.34297/AJBSR.2024.21.002805
Abstract
Management and treatment of peri-pancreatic abscess after simultaneous kidney pancreas transplantation generally includes initiation of empiric antibiotics with consideration for percutaneous drain placement. However, this is the first documented case of symptomatic intramural abscess of the recto-sigmoid junction after simultaneous kidney and pancreas transplantation that required a gastroenterologist unique minimal invasive approach.
Keywords: Simultaneous kidney pancreas transplantation, Peri-transplant fluid collection, Intramural abscess
Introduction
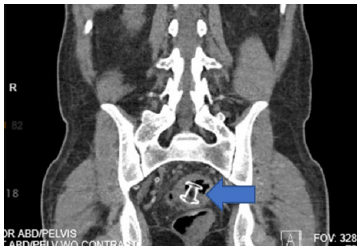
Simultaneous Kidney Pancreas Transplantation (SPK) is the gold standard treatment for patients who have developed end stage renal disease secondary to type 1 diabetes [1]. However, transplantation is not without risk. Undergoing simultaneous kidney pancreas transplant increases the risk of morbidity, including infection, anastomotic leak, and abscess formation, compared to kidney transplantation alone [2]. The development of a peri-pancreatic fluid collection is a known complication after undergoing SPK and will be detected by Ultrasound (US) or Computed Tomography (CT) imaging. Here, we present the first reported case involving a patient with ill-defined symptoms found to have a peri-pancreatic and intramural large abscess formation at the level of recto-sigmoid junction (Figure 1).
Presentation of Case
41-year-old male with a history of end stage renal disease secondary to type 1 diabetes on hemodialysis had undergone SPK with enteric drainage. 8 months later, he presented with neutropenic fever, malaise, and diarrhea. He started on IV antibiotics. CT of the abdomen and pelvis revealed a multiloculated, thick-walled, rim-enhancing peri-pancreatic transplant fluid collection in the pelvis with a large intramural recto-sigmoid junction abscess formation that near complete obstruct the lumen of the sigmoid colon (Figures 1,2). The intramural component measured approximately 5.9 x 4.4 x 10.8cm.
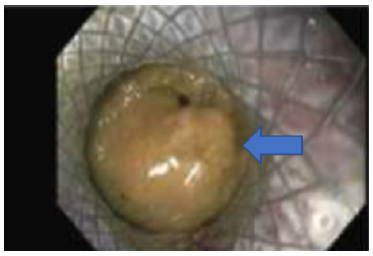
Gastroenterology was consulted for flexible sigmoidoscopy. A large submucosal bulge at the junction of recto sigmoid was seen. Endoscopic ultrasound demonstrated that the peri-pancreatic abscess had a well-defined capsule directly adjacent to the bowel wall. Ultrasound-guided lumen-apposing Metal Stent (LAMS) or AXION Stent was placed. Copious amount of purulent discharge drained and send for culture (Figure 3). Interval CT imaging was obtained 72-hours later, demonstrating. improvement in abscess size (Figures 4, 5). He then underwent interval flexible sigmoidoscopy in a week that showed the resolution of the recto-sigmoid junction abscess. Post procedure follows up in 3 month he was doing well, off the antibiotics and Ct scan did not show recurrence of the abscess.

Figure 1: CT of peri-pancreas transplant abscess with intraluminal component of the recto-sigmoid junction (Coronal).
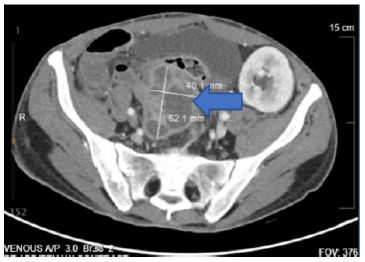
Figure 2: CT of peri-pancreas transplant abscess with intraluminal component of the recto-sigmoid junction (Axial).
Discussion
Immunosuppression increases risk of infection after solid organ transplantation [3]. Development of an abscess after solid-organ transplantation is a known complication for immunocompromised patients and can be a significant cause of morbidity, allograft dysfunction, rejection, and mortality. Early detection and intervention with a multidisciplinary approach has been the key to gaining source control and treat the infection.
Incidental peri-transplant fluid collections without evidence of systemic infection or allograft dysfunction can generally be observed. However, fluid collections with complex features on the imaging, mass effect, systemic signs of graft dysfunction or infection require intervention. These collections can be medically managed with antibiotics and consideration for percutaneous drain placement. If there are systemic signs of infection, the goal is to gain adequate control of the infectious source. In this case, early intervention with a multidisciplinary approach was key to gaining source control of the intramural component of the abscess in the sigmoid colon with Ultrasound guided drainage and lumen apposing Stent placement.
Endoscopic interventions are associated with improved outcomes and reduced risk of complication, as well as fast recovery time [4]. Endoscopic ultrasound-guided drainage with use of AXIOS lumen Apposing Metal Stent (LAMS) has become a preferred approach for the management of complex and symptomatic peripancreatic fluid collections, specifically. In this case, LAMS was able to be deployed due to the proximity of the intramural abscess to the colon wall. This stent created a successful tract for intramural abscess drainage. Source control was then further reinforced with pigtail catheter placement within the stent and IV antibiotics.
Acknowledgement
None.
Conflict of Interest
None.
References
- Ojo Akinlolu O, Meier Kriesche, Herwig Ulf, Hanson Julie A, Leichtman Alan, et al. (2001) The Impact of Simultaneous Pancreas-Kidney Transplantation on Long-Term Patient Survival. Transplantation 71(1): 82-89.
- Pirsch JD, Andrews C, Hricik DE, Josephson MA, Leichtman AB, et al. (1996) Pancreas transplantation for diabetes mellitus. Am J Kidney Dis 27(3): 444-450.
- Meier Kriesche HU, Li S, Gruessner RW, Fung JJ, Bustami RT, et al. (2006) Immunosuppression: evolution in practice and trends, 1994-2004. Am J Transplant 6(5 Pt 2): 1111-1131.
- Chandraprakash Umapathy, Mahesh Gajendran, Rupinder Mann, Umesha Boregowda, Thimmaiah Theethira, et al. (2020) Pancreatic fluid collections: Clinical manifestations, diagnostic evaluation and management, Disease-a-Month 66(11): 100986.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.