Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Occult Breast Carcinoma Presenting as Axillary Metastases, about Two Cases and Review of the Literature
*Corresponding author:Oumaima Talbi, Department of medical oncology, Hassan II University Hospital, University Sidi Mohamed Ben Abdellah, Fez, Morocco.
Received: February 28, 2024; Published: March 05, 2024
DOI: 10.34297/AJBSR.2024.21.002886
Abstract
Background: Occult breast cancer is a very rare type of cancer which presents with axillary lymphadenopathy with no visible mass in the breast, significant progress in breast imaging has taken place since its description, as well as its incidence. To date, optimal management of this type of cancer is lacking.
Case Presentation: We report two cases of occult breast carcinoma diagnosed at the department of Medical Oncology after presenting an axillary nodule. No relevant anomalies in the breast or other organs were found. The treatment consisted of neoadjuvant chemotherapy, axillary surgery, breast radiotherapy, and hormone therapy.
Conclusion: This case report demonstrates that histological and immunohistochemical results were crucial in identifying its mammary origin, The conservative approach (axillary lymph node dissection combined with breast radiotherapy) is currently the preferred approach when the breast MRI does not identify the primary lesion.
Keywords: Occult breast cancer, Axillary metastasis, Breast RMI
Introduction
Halsted initially reported occult breast cancer (OBC) in 1907, defining it as a clinically identifiable metastatic cancer originating from an undetectable primary breast tumor [1]. It represents 0.3 to 1% of all breast cancers [2]. The diagnostic and therapeutic approach to occult breast cancer (OBC) relies on evaluating its clinical presentation as well as conducting histological and immunohistochemical analyses. This article was conducted to assess the presentation and the management of two patients with occult breast cancer in the medical oncology department of the Hassan II University Hospital in Fez.
Cases Presentation
1st Case
A 57-year-old woman menopaused with no medical history, specifically regarding gynecological or oncological issues, who consults for a left axillary lymphadenopathy in January 2022. The clinical examination finds a mobile left axillary ADP measuring 2 cm in its largest dimension. No masses were identified in the right axilla, breasts, or bilateral supraclavicular areas. A bilateral mammogram and breast ultrasound were performed, both of which were normal apart from left axillary lymphadenopathy of 2 cm on average classified ACR4. RMI did not identify the primary tumour.
The adenectomy performed showed Lymph node metastasis of a poorly differentiated adenocarcinoma, first evoking a breast origin. Pathological examination revealed a left axillary metastasis (Figure 1). Immunohistochemical (IHC) results were: RE 30%, RP négatif, GATA3 (+), mammoglobine negatif. Primitive breast cancer was the suspected etiology.

Figure 1: Paraffin sections of the lymph node with metastasis, stained with H&E in A (×2) and B (×5).
Following a multidisciplinary evaluation of the breast involving surgeons, oncologists, radiotherapists, and pathologists, it was decided to start neoadjuvant systemic chemotherapy - four cycles of neoadjuvant chemotherapy according to AC-P protocol (anthracyclin, cyclophosphamide and paclitaxel). The surgery was followed by whole breast radiotherapy (WBRT) and hormone therapy (HT) with letrozole.
2nd Case
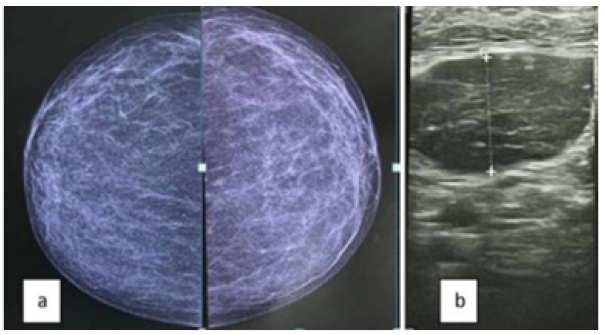
56-year-old women was admitted to our institution in January 2020 to clarify an asymptomatic right axillary lump. She was being treated for chronic hypertension and had no relevant family history. A bilateral mammogram (Figure 2) and a breast ultrasound were normal. Images were reviewed and a needle biopsy was performed. Pathological examination revealed a right axillary metastasis. Immunohistochemical profile with 90 % positivity for estrogen and progesterone receptors, and Ki-67 60 % (Luminal B like). MRI was performed showing no pathological changes. PET-CT, in addition to abnormal uptake in the axillary lesion, showed no pathological FDG uptake. The IHC profile suggests a breast origin. The patient underwent a supero-external quadrantectomy following the decision of the CPR.
The surgery was followed by chemotherapy with anthracyclines and taxanes, whole breast radiation therapy (WBRT) and HT with letrozole.
Discussion
Cancer of unknown primary site accounts for 4-5% of all invasive cancers [3], Axillary adenopathies of malignant origin include various types of cancers, notably those of the breast, thyroid, lung, pancreas, stomach, colon, uterus, and ovaries. The biopsy of the suspicious lymph node, and the subsequent immunohistochemical study, will allow the diagnosis IHC staining proves highly valuable in diagnosing the primary site, often requiring a comprehensive panel. In breast cancer, the typical expression of CK7, absence of CK20, and occasional negativity for TFF1 [4] along with ER and PrR positivity, support the identification of an occult breast primary. However, it's essential to note that a negative staining result does not rule out the possibility of breast cancer.
However, these metastases rarely present as the initial signs of the disease. This underscores the need for numerous para-clinical investigations to facilitate a comprehensive differential diagnosis. The first-line diagnostic tools typically include ultrasound mammography and thoraco-abdominopelvic computed tomography. MRI is now considered the standard approach for evaluation of breasts in OBC patients [5,6].
There is a lack of consensus for the treatment of CUP syndrome from OBC, and various therapeutic strategies have been proposed. The choice of a treatment regimen remains controversial, the literature does not clearly support the mass use of one or the other [7] Mastectomy showed lower rate of local recurrence and superior disease free and overall survival than no local therapy. However, surgery became more conservative [8,9] as studies demonstrated that mastectomy did not improve survival outcomes, locoregional recurrence or distant metastasis [10] compared to breast conservative surgery (BCS). Axillary radiotherapy after surgery is essential to reduce the risk of local axillary recurrence [11] Research findings have substantiated its viability as a suitable substitute for mastectomy. Exclusive breast radiotherapy, while less extensively examined in the literature, emerges as an intriguing alternative to radical mastectomy, as indicated by the retrospective study conducted by Vlastos, et al.
Regarding adjuvant systemic therapy, NCCN recommends systemic chemotherapy, endocrine therapy and biologic therapy (anti-HER2 monoclonal antibody) according to the same indications as for stage II and III disease.
For the first case, depending on the lymph node stage, neoadjuvant treatment was carried out. After evaluation by a multidisciplinary team, the second patient benefited from a multimodal treatment including surgery, adjuvant chemotherapy, radiotherapy and hormonal and biological treatment.
References
- W S Halsted (1907) The results of radical operations for the cure of breast carcinoma Anne. Surg 46(1): 1-19.
- Walker GV, Blacksmith GL, Perkins GH, Oh JL, Woodward W, Yu TK, et al. (2010) Population-based analysis of occult primary breast cancer with axillary lymph node metastasis. Cancer 116(17): 4000-4006.
- Hainsworth JD, Greco FA (2019) Overview of the classification and management of cancers of unknown primary site.
- Kaklamani V, Gradishar WJ (2019) Axillary node metastases with occult primary breast cancer.
- M Terada, Y Adachi, M Sawaki, M Hattori, A Yoshimura, G Naomi, et al. (2018) Occult breast cancer may originate from ectopic breast tissue present in axillary lymph nodes. Breast Cancer Res Treat 172(1): 1-7.
- (2019) NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®)-Breast Cancer. Version 1.
- Massard C, Rochaix P, Ilié M (2016) Cancer of unknown primary (CAPI): a new hope? pp. 6.
- FIB Macedo, JJ Eid, J Flynn, MJ Jacobs, VK Mittal (2016) Optimal surgical management for occult breast carcinoma: a meta-analysis. Ann Surg Oncol 23(6): 1838-1844.
- F Couder, C Schmitt, I Treilleux, O Tredan, C Faure, et al. (2015) Axillary lymph node invasion without primary breast tumor found: about 16 cases from a cohort of 7770 patients. Gynecol Obst Fertil 43: 588-592
- Ge, X.Y. Liu, Y. Xiao, Z.C. Gou, S. Zhao, Y.Z. Jiang, et al. (2018) Clinicopathological characteristics and treatment outcomes of occult breast cancer: a SEER population-based study. Cancer Manag Res 10: 4381-4391.
- G Vlastos, M E Jean, A N Mirza, N Q Mirza, H M Kuerer, et al. (2001) Feasibility of breast preservation in the treatment of occult primary carcinoma presenting with axillary metastases. Ann Surg Oncol 8(5): 425-431.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.