Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Ochronosis? Osteomyelitis? Cervical Disc Calcification in the Pediatric Population: 4 Cases Series
*Corresponding author:Carla Olim Castro, Praceta Professor Mota Pinto, 3004-561, Coimbra, Portugal.
Received: January 8, 2024; Published: January 22, 2024
DOI: 10.34297/AJBSR.2024.21.002819
Abstract
Intervertebral disc calcification is a rare condition affecting healthy children aged 5-10 years. It manifests as acute disabling neck pain with limited range of motion and torticollis. Plain radiography is the diagnostic examination of choice, CT and MRI are useful in the study of calcifications and involvement of adjacent structures.
The authors present 4 cases of pediatric patients with intense neck pain and torticollis of sudden onset without trauma, irradiation or local inflammatory signs. The 4 patients where female and aged 3-10. The spine radiograph presented cervical disc calcifications at one level in 3 patients and 1 patient presented with cervical and thoracic disc calcifications. Blood examination was performed, with normal findings in 3,1 presented higher levels of acute inflammatory indicators. Conservative treatment was adopted and 1 had antibiotic treatment.
After exclusion of high-energy trauma, metabolic disorders such as ochronosis or phosphorous-calcium metabolism abnormalities, infectious pathology such as osteomyelitis/spondylodiscitis and tumour, a review of the literature on the subject was performed. The clinical picture of neck pain in a child of this age, in the absence of comorbidities and with radiological evidence of disc calcifications suggests the diagnosis of Intervertebral Disc Calcification (IVDC). Despite its frightening clinical presentation and challenging diagnosis, intervertebral disc calcification is a self-limiting condition with an excellent outcome.
Keywords: Intervertebral disc, Pediatrics, Torticollis, Neck Pain, Paediatrics, Wryneck, Cervicalgia
Level of Evidence: IV
Type of Study: Case Series
Introduction
Intervertebral Disc Calcification (IVDC) was first described by Baron [1] in 1924 and since then there is only about 300 reported cases [2]. This rare disease affects children aged between 5 to 10 years old and has a higher incidence in boys [3-5]. The etiology of IVDC remains unclear.
Most of the children affected are completely asymptomatic diagnosed by incidental imaging findings. Symptomatic children present with acute-onset cervical or dorsal pain, stiffness and with limited range of motion, that can mimic spondylodiscitis, meningitis, traumatic injuries or even tumor [2-4]. In rare occasions, neurologic symptoms have been reported [2,4,6].
The cervical spine is the most affected, often in the C4 to C7 segment, and usually occurs in a single disc, however IVDC can involve thoracic spine, rarely lumbar spine, and affected multiple discs [3,4]. Diagnosis is based on imaging tests, particularly plain radiography of the affected segment [4,5]. Intervertebral disc calcification is characterized by radiopaque round or ovoid calcified structure in the intervertebral disc space, often with a fragmented appearance [4]. CT and MRI are useful in the study of disc herniation with compression of neighboring structures in the presence of neurological symptoms.
IVDC is a self-limiting condition with an excellent outcome [3,5]. The gold standard treatment is conservative and comprises non-steroidal anti-inflammatory drugs, analgesics, rest, cervical collar or a combination of these treatments [3,4]. Surgical treatment is reserved for specific cases where neurologic symptoms persist despite conservative treatment [5]. The authors describe 4 cases of symptomatic intervertebral disc calcification in girls aged 3-10, all presented cervical disc calcification and 1 with multilevel discs disease involving thoracic spine.
Case Series
Patient 1
This patient was a 10years old girl admitted to emergency department with exacerbation of cervical pain and torticollis with onset 5 months earlier. It was an acute disabling pain, day and night, aggravated by movement and with limited range of motion. The pain had no irradiation, no local inflammatory signs and only relieved with tramadol. She was a healthy girl without history of trauma, recent infection or fever. The blood tests revealed normal values of leucocytes, CRP and ESR and negative homogentisic acid research. Imaging showed radio-opaque disc lesions at C5-C6, C6-C7 and T2-T3 levels and involvement of C5 and C6 vertebral bodies (Figure 1). The patient started therapy with non-steroidal anti-inflammatory drugs with symptoms improvement. This is the most recent case with only 9months of follow-up.
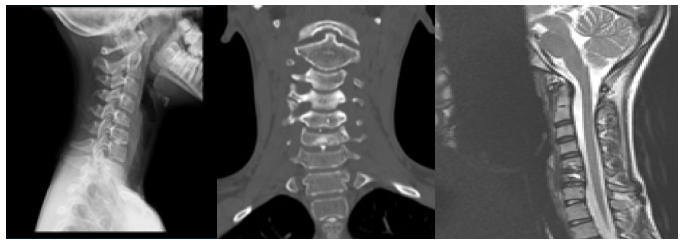
Figure 1: Patient 1 at presentation: radio-opaque disc lesions at C5-C6, C6-C7 and T2-T3 levels. A - X-ray in lateral view of cervical spine. B - Cervical CT-scan coronal view with disc lesions and involvement of C5 and C6 vertebral bodies. C - MRI sagittal T2 weighted image, with low disc signal at C5-C6 and C6-C7 and intervertebral disc herniation with bone edema at C5-C6; no medullar compression neither perivertebral soft tissue swelling.
Patient 2
This patient was a 9years old girl admitted to emergency department with complaints of intense lower cervical and upper dorsal pain and limited range of motion for 3 days. The pain irradiated to the left scapular region. There were no local inflammatory signs and no neurological deficits. There was no history of trauma, recent infection, headaches or fever. The blood teste was normal parameters including the phosphorous-calcium metabolism. The x-ray and CT-scan showed a radio-opaque disc lesion at C4-C5 (Figure 2). The MRI revealed a D2-D3 disc herniation with inferior retrosomatic migration and C4-C5 nucleus pulposus calcification (Figure 3). She was hospitalized for pain control that consisted of rest and anti-inflammatory therapy and discharged 14 days after. The girl was regularly evaluated at medical appointments, with no pain complaints. The MRI was repeated after one year with regression of the calcification.
Patient 3
This patient was a 3years old girl admitted to emergency department with cervical pain and torticollis lasting 1 week, which was associated with a fall 2 weeks before. She presented with limited left neck rotation, no limitation to the right side and no neurological deficits. The blood test was normal parameters. The imaging tests showed a C3-C4 nucleus pulposus calcification. She was regularly assessed in medical appointments and maintained sporadic complaints of cervicalgia for 6 months. The MRI was repeated after 4 months and 1 year with improved of C3-C4 intervertebral disc signal.

Figure 2: Patient 2 at presentation: Cervical CT-scan sagittal view with radio-opaque disc lesion at C4-C5.
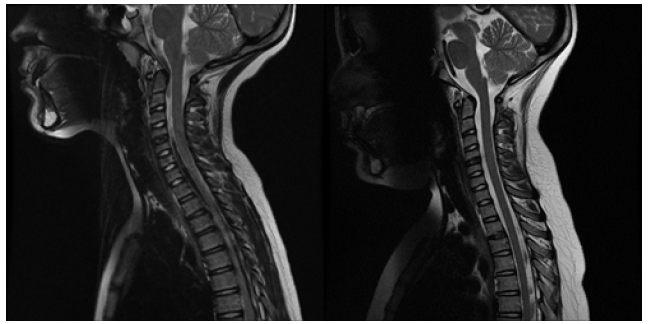
Figure 3: MRI of Patient 2 at presentation with lesion at C4-C5 disc and D2-D3 disc herniation with inferior retrosomatic migration, and at one year follow-up. A –Sagittal T2 weighted image at presentation. B - Sagittal T2 weighted image at one year follow-up, with regression of D2-D3 disc herniation.
Patient 4
This patient was a 4years old girl admitted to emergency department with cervical pain and torticollis for 15 days. She had tonsillitis 7 days prior to the onset of cervical complaints. At emergency department she presented with right lateralization of the neck and no neurologic deficits. The blood tests revealed higher levels of acute inflammatory indicators, CRP and ESR and leucocytosis, but negative blood culture. The CT scan revealed C4 body deformity and C3-C4 disc calcification with narrowing of the right nerve root canal (Figure 4). The MRI study confirmed C4 deformity, vertebra plana, and bone marrow signal alteration (Figure 5). The girl was hospitalized with suspicious diagnosis of C4 osteomyelitis, discharged after 31 days and completed a total of 14 days of gentamicin and 45 of flucloxacillin. The girl was regularly evaluated at medical appointments, with no pain complaints and improved of C3-C4 intervertebral disc signal at one year follow-up. This is the oldest case with 10 years follow-up.
Discussion
Intervertebral disc calcification is a rare disease with an unclear etiology and the real incidence of disc calcifications in children is unknown [7]. Some authors suggest that IVDC can be related to trauma, metabolic changes, inflammatory or infectious pathology or vascular causes [4,7]. In children, the intervertebral disc blood supply is large and has a more active metabolism, which is increased in case of inflammation. This could be an explanation for the sudden appearance and disappearance of the intervertebral disc calcification after a hematoma followed by calcification secondary to trauma or infection [7]. Another hypothesis is that at the age of 5 to 12 years the maturation of intervertebral disc occurs, in which the nutritional supply changes from a microvascular system to an osmotic avascular system [6]. The occurrence of trauma or infection at that time will make that vulnerable disc susceptible to ischemia, necrosis, herniation, and calcification [5,8]. Afterwards, an inflammatory response occurs which increases the supply of nutrients and consequently leads to the spontaneous resolution of the calcified disc [5,8]. IVDC is a self-limiting disease that occurs in nucleus pulposus, while in adults disc calcification is permanent and affects annulus fibrosis [2,3,7,9].
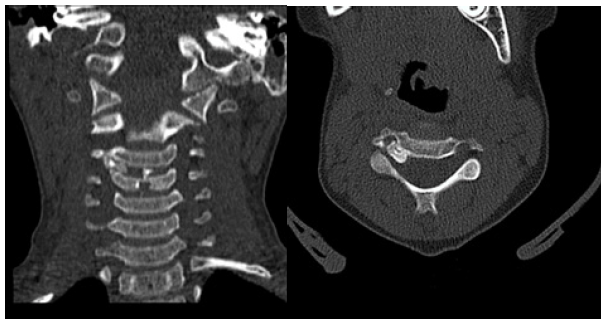
Figure 4: Cervical CT-scan of Patient 4 at presentation with C4 body deformity and C3-C4 disc calcification with narrowing of the right nerve root canal. A – CT-Scan coronal view. B - CT-Scan axial view.
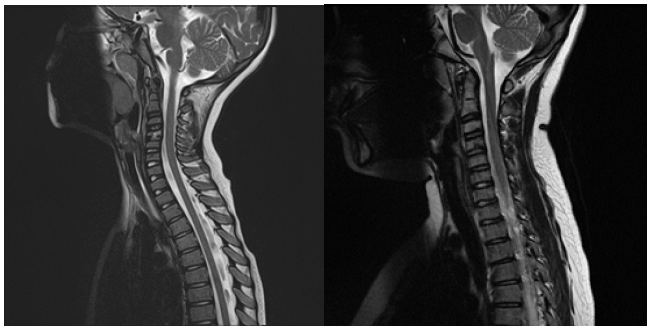
Figure 5: MRI of Patient 4 at presentation with C4 deformity and bone marrow signal alteration and at seven-year follow-up with regression of the lesion. A – Sagittal T2 weighted image at presentation. B – Sagittal T2 weighted image at seven-year follow-up.
A very few children with disc calcification will experience symptoms. Beluffi, et al. assessed children radiographs over 26 years and found 6 cases of intervertebral disc calcification, of those only 1 presented with acute neck pain [7]. It is thought that the increased pressure of the calcified disc may be the cause of symptoms in patients without herniation [3]. When symptomatic, IVDC patients are present with neck or back pain in 85%, limited range of motion in 32%, 20% complain of torticollis and 5% can have antalgic scoliosis [4]. In rare occasions, neurologic symptoms have been reported due to compression of nerve roots or spinal cord by the calcified nucleus pulposus herniation into the spinal canal [2,4,6]. Coppa et al. revised 51 studies involving 91 children, the neurological status was normal in 63%, whereas radiculopathy was described in 29% cases and myelopathy signs in 9% [4]. Lam, et al., reported a case of a 12years old athletic girl that was presented with acute incomplete spinal cord injury with Brown-Séquard-plus syndrome [6]. In our series, despite the fact that Patient 4 presented C3-C4 disc calcification with narrowing of the right nerve root canal, no neurologic deficits were observed.
The cervical spine is the segment most frequently affected, 64-74%, and the calcification tends to occur in a single disc space, as reported in this series [5,7,9,10]. In the Coppa study, a single level was affected in 70%, two levels in 19% and more than two levels in 10% of the cases [4].
The diagnosis is based on imaging tests, mainly plain radiography of the affected segment. However, due to the rarity of IVDC, the 4 patients underwent a more detailed imaging study using CT and MRI. On plain radiographs the lesions are characterized by round or ovoid calcified structure in the intervertebral disc space, often with a fragmented appearance [4,7,9,11]. CT scan allows a more accurate evaluation of calcifications and involvement of neighboring structures, such as the narrowing of the C3-C4 right nerve root canal, showed in patient 4 [4,7]. Some studies reported neurologic deficit associated to disc herniation and/or posterior ligament calcification [5,6,8,12]. The MRI is useful to assess spinal cord and nerve roots conditions and bone edema [4,7]. Of special note is the absence of perivertebral soft tissue swelling in this pathology [7]. IVCD can cause chances in adjacent vertebral bodies such as anterior or posterior wedging, flattening, irregularities or marginal sclerosis and bone edema [4,7,13]. These changes were evident in Patient 4, C4 vertebra plana - like, and contributed to the misdiagnosis of osteomyelitis. Another typical feature IVDC is that the calcified structure tends to gradually disappear, with minor radiographic abnormalities remaining. In our series only Patient 1 had no regression of the calcification due to the short time of follow-up, whereas in the others the MRI showed calcification regression after one year.
Laboratory tests can be useful in the IVDC differential diagnosis. The acute inflammatory indicators, CRP and ESR and leucocytes, tend to be normal or slightly elevated [2,4,5,10,11]. The investigation of metabolic disorders such as homogentisic acid research, phosphorous-calcium metabolism abnormalities and microbiological studies may also be useful in the differential diagnosis, as shown in this series. Alkaptonuria is an autosomal recessively inherited disorder caused by a deficiency of an enzyme in tyrosine metabolic pathway resulting in increased homogentisic acid reserves. Homogentisic acid accumulates in circulation and in cells, leading to increased excretion in the urine, alkaptonuria, and after a chemical modification it is gradually deposited in the connective tissue, ochronosis, resulting in intervertebral discs calcification [13,14]. However, this calcification usually occurs in adults. Metabolic disorders like hypervitaminosis D are associated with calcification of annulus fibrosis but is not typically associated with childhood nucleus pulposus calcification [13].
The differential diagnosis of IVDC with infectious pathology can be challenging and the case of patient 4 is an example of that. Despite negative microbiology, this patient had a clinical picture and analyses highly suggestive of infectious pathology and a C4 deformity that could corroborate the diagnosis of osteomyelitis. In the presence of these data, combined with lack of knowledge of IVCD, she was diagnosed with osteomyelitis and underwent 45 days of antibiotic therapy. It was later revealed to be a self-limiting disease, masked by the analytical tests compatible with recent streptococcal infection, related to the tonsillitis she had contracted previously. It should be noted that osteomyelitis/spondylodiscitis are more common in the lumbar spine and have different radiological findings such as narrowing of the intervertebral space, perivertebral soft tissue swelling, possible vertebral-body fusion as a sequel and never disc calcification [7].
In the presence of acute and disabling neck pain with radiological changes in a previously healthy child, we must be suspicious of traumatic injuries, infectious pathology such as chronic recurrent multifocal osteomyelitis, spondylodiscitis and meningitis, metabolic pathology, and tumor [4,15]. However, the evidence of an intervertebral disc calcification suggests the diagnosis of IVDC [4].
The gold standard treatment is conservative and comprises non-steroidal anti-inflammatory drugs, analgesics, limited activity, cervical soft collars, or a combination of these treatments [2-4,10]. The presence of a nerve root or spinal compression by a calcified disc is not an absolute indication for surgery as this tends to resolve spontaneously. Dai et al. documented the self-limiting course of IVDC, of the 17 children reported, 6 had neurological deficits and none required surgery [9]. Surgical treatment is reserved for specific cases where neurologic symptoms persist despite conservative treatment [5,6,10,12].
Conclusion
In the absence of high-energy trauma, tumors and infection, neck pain in a child aged 5-10 years with disc calcifications suggests the diagnosis of intervertebral disc calcification.
Despite a frightening clinical presentation and challenging diagnosis, intervertebral disc calcification is a self-limiting disease with an excellent prognosis.
Acknowledgement
The work was conducted at Spine Unit, Hospital CUF Descobertas.
Conflict of Interest
The authors have no conflicts of interest to declare.
References
- Baron A (1924) About a new disease of the spine. Jahrd Kinderheilk 104: 357-360.
- Dushnicky MJ, Okura H, Shroff M, Laxer RM, Kulkarni A V, et al. (2019) Pediatric Idiopathic Intervertebral Disc Calcification: Single-Center Series and Review of the Literature. J Pediatr 206: 212-216.
- Magnus K (1998) Intervertebral disc calcification in children. SA J Radiol: 8-11.
- Coppa V, Marinelli M, Martiniani M, Giacchetta AM, Gigante AP, et al. (2020) Pediatric intervertebral disc calcification: Case series and systematic review of the literature. Journal of Pediatric Orthopaedics Part B 29(6): 590-598.
- King HJ, Ramchandani R, Maxwell C, Sarkar A, Loven T, et al. (2021) To cut or not to cut? A case report on pediatric intervertebral disc calcification. Surg Neurol Int 12: 307.
- Lam SK, Niedzwecki CM, Daniels B, Mayer RR, Vakharia MM, et al. (2016) Acute spinal cord injury associated with multilevel pediatric idiopathic intervertebral disc calcification: Case report. J Neurosurg Pediatr 17(2): 182-186.
- Beluffi G, Fiori P, Sileo C (2009) Calcifications of intervertebral discs in children. Medical Radiology 114: 331-341.
- Wang G, Kang Y, Chen F, Wang B (2016) Cervical intervertebral disc calcification combined with ossification of posterior longitudinal ligament in an-11-year old girl: case report and review of literature. Child’s Nervous System 32(2): 381-386.
- Dai LY, Ye H, Qian QR (2004) The natural history of cervical disc calcification in children. J Bone Joint Surg Am 86(7): 1467-1472.
- Tsutsumi S, Yasumoto Y, Ito M (2011) Idiopathic intervertebral disk calcification in childhood: A case report and review of literature. Child’s Nervous System 27(7): 1045-1051.
- Garg M, Kumar S, Satija B, Gupta R (2012) Pediatric intervertebral disc calcification: A no touch lesion. J Craniovertebr Junction Spine 3(1): 23-25.
- Sato K, Nagata K, Park JS (2005) Calcified intervertebral disc herniation in a child with myelopathy treated with laminoplasty. Spinal Cord 43(11): 680-683.
- Barrett MO, Anderson JT, Rao B, Vaslow D, Hoernschemeyer DG, et al. (2008) Multilevel pediatric cervicothoracic intervertebral disc calcifications. Am J Orthop 37(7): 126-128.
- Aliberti G, Pulignano I, Schiappoli A, Minisola S, Romagnoli E, et al. (2003) Bone metabolism in ochronotic patients. J Intern Med 254(3): 296-300.
- Sergi CM, Miller E, Demellawy D El, Shen F, Zhang M, et al. (2022) Chronic recurrent multifocal osteomyelitis. A narrative and pictorial review. Front Immunol 13: 959575.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.