Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Paratesticular Liposarcoma: A Case Report and Review of the Literature
*Corresponding author:Khadija Hinaje, Department of medical oncology, Hassan II University Hospital, University Sidi Mohamed Ben Abdellah, Fez, Morocco.
Received: February 20, 2024; Published: February 23, 2024
DOI: 10.34297/AJBSR.2024.21.002868
Abstract
We report the case of a well-differentiated paratesticular liposarcoma in a 45-year-old man. This rare tumor develops from the fatty tissue surrounding the testicle and the spermatic cord. Clinical and radiological signs are nonspecific, and the diagnosis is usually only made on the operative specimen. Treatment consists of radical inguinal orchidectomy. Adjuvant radiotherapy may have a role in high-grade tumors with lymphatic invasion or in cases of incomplete resection and recurrence. The role of systemic treatment remains controversial. The prognosis of well-differentiated paratesticular liposarcoma is better than that of others. Despite its slow progression, prolonged surveillance is necessary due to the high risk of late recurrence.
Keywords: Paratesticular liposarcoma, Well-differentiated liposarcoma, Orchidectomy
Introduction
Paratesticular Liposarcoma (PLS) develops from the adipose tissue surrounding the spermatic cord and covers the testicle and epididymis [1]. It is an extremely rare pathological entity. Approximately 200 cases have been reported in the literature, but their incidence has been slowly increasing [2]. Due to the rarity of cases, there is no standardized management for PLS, posing a real challenge for clinicians. In this paper, we report a case of a well-differentiated paratesticular liposarcoma with the aim of further understanding the diagnosis and treatment of this rare disease.
Case Presentation
In January 2021, a 45-year-old unmarried patient with no significant medical history, was admitted to our hospital with an increasing right inguinal mass lasting for 6 months. Examination revealed a right hard and painless inguinal mass, measuring approximately 10cm in maximum diameter with poorly defined border and extended to the right testis and epididymis. It’ was the only positive finding of physical examinations. The left testis and epididymis were well developed. There are no specific abnormalities in the laboratory examinations notably Alpha-Fetoprotein (AFP) and Human Chorionic Gonadotropin (HCG) were negative, Lactate Dehydrogenase (LDH) at 171U/L. However, pelvic CT scan demonstrated a right inguinal mass with fatty density measuring 100 mm in its largest dimension, well circumscribed, extending to the right testis and epididymis: this appearance suggested a tumor of the spermatic cord of lipomatous nature: lipoma or liposarcoma (Figure 1). Ten days later, the patient underwent a right orchidectomy. The microscopic examination showed a well-circumscribed adipose tumor proliferation, to be definitively characterized after IHC study. The resection was complete. Immunohistochemical study showed positive results for CD34 and CDK 4. Molecular biology revealed amplification of the MDM2 gene, indicating a cytogenetic profile consistent with well-differentiated liposarcoma (Figure 1). A staging post-operative CT of the thorax, abdomen and pelvis was performed which was negative for metastatic disease. Then the case was referred to our Department of Medical Oncology. No indication for radiotherapy or systemic treatment was deemed necessary. At 3 years follow-up, there is no evidence of local recurrence or distant metastasis (Figure 2), (Figure 2a, 2b,2c,2d).

Figure 1: CT scan showing the solid soft-tissue paratesticular mass, well circumscribed, extending to the right spermatic cord (red arrow).
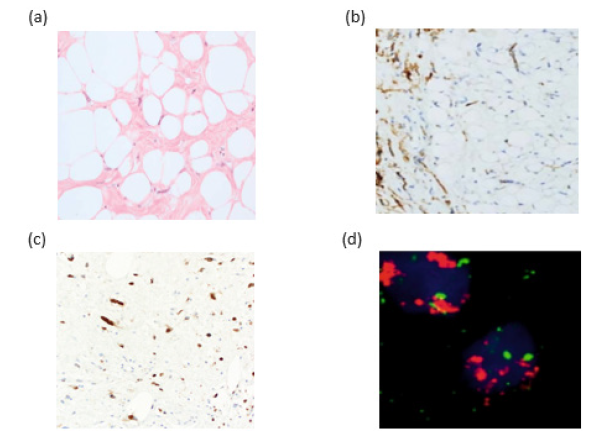
Figure 2: (a): Well-differentiated liposarcoma, adipocytes with cytologic atypia cells. (b): Immunohistological examination showed nuclear positivity for CDK34, (c): Immunohistological examination showed nuclear positivity for CDK4, (d): FISH assay with MDM2 target showed increased signals (red), corresponding to MDM2 gene amplification.
Discussion
Liposarcoma accounts for 20% of adult paratesticular tumors and ranks third after leiomyosarcoma (32%) and rhabdomyosarcoma (24%) [3] (Figure 2). Most sarcomas have not been associated with risk factors, but some environmental and genetic predispositions have been suggested in a minority of patients [4]. LPS mainly occurs in individuals aged between 50 and 60 years old. It is more common on the right, as in the case of our patient [3].
Clinically, LPS progresses slowly over several months to years. It manifests as pain, heaviness, or a pulling sensation in 10-15% of cases. It presents as a firm, irregular, painless mass, located near or distant from the testicle, which can be either intrascrotal or in the groin, or encompassing both areas. Its size varies, ranging from a few centimeters to over 30 centimeters, and it can reach enormous proportions, up to 13.5 kg. It may present a differential diagnosis challenge with inguinal hernia or hydrocele. Thera are no specific tumor markers or characteristic radiological signs. On Ultrasonography (US) examination, PLS are identified as solid, heterogeneous solid and hypoechoic lesions. However, US cannot always distinguish PLS from lipomas if the tumor is small or it is a well-differentiated PLS with homogenous fatty pattern, which makes PLS similar to lipoma [5]. CT usually demonstrates the tumor area with lower density. It may be helpful to establish tumor location, tissue characteristics, staging and follow-up [6]. MRI, the golden standard in staging soft tissue tumors, not only provides clear information on the tumor foci but also characterizes and delineates the degree of local tumor extension [7].
Histologically, different types of PLS are described: well-differentiated, dedifferentiated, myxoid, pleomorphic and myxoid pleomorphic liposarcoma according to the 2020 World Health Organisation (WHO) classification of tumors of soft tissue and bone [3]. The well-differentiated type accounts for approximately 50% of cases. Liposarcomas are immunoreactive for MDM2 and CDK4 markers, which can help differentiate the lesion from benign lipomas. However, the most specific immunohistochemical marker is the S100 protein, which is positive in up to 90% of cases; and highgrade tumors are often positive for desmin [8].
Due to the rarity of PLS, treatment recommendations are based on case reports, small series and literature reviews, making difficult any generalization regarding treatment. Radical inguinal orchiectomy and complete resection of the tumor with negative microscopic margins (R0) are the current standard treatment strategies [9,10]. Hemicortectomy may be justified in cases of extracapsular tumor with invasion of adjacent structures. There is no clear consensus regarding the utility of retroperitoneal lymph node dissection; it should be reserved for patients with identified lymphadenopathy. Liposarcomas are tumors sensitive to radiation. However, the role of radiotherapy remains uncertain. Coleman and al. reported that adjuvant radiotherapy does not significantly reduce the rate of local recurrence and does not improve overall survival [11]. Other authors have observed more sustainable control following combined surgery and radiotherapy. A combined approach should be considered, especially in cases of high-grade tumors, lymphatic invasion, involved resection margins, or in case of recurrence. The irradiated area should encompass the proximal part of the scrotum, the pathway of the inguinal canal, as well as adjacent tissues and ipsilateral pelvic lymph nodes. The role of chemotherapy in the treatment of liposarcomas is controversial, and it may be considered on a caseby- case basis. Adjuvant chemotherapy has been reported in two cases, but the follow-up was short. Chemotherapy with doxorubicin has been used occasionally. The prognosis of well-differentiated paratesticular liposarcoma is better than that of other sarcomas. Its progression is slow, and its metastatic potential is minimal, whereas dedifferentiated forms result in metastases in 15 to 20% of cases. Local recurrence is the main issue with paratesticular sarcomas, occurring in 30 to 50% of cases, sometimes after delays exceeding five years. Thus, long-term surveillance is required in all cases.
Conclusion
Well-differentiated paratesticular liposarcoma is a rare tumor. The lack of specific clinical and radiological signs makes preoperative diagnosis difficult. Surgical treatment involves radical orchidectomy +/- ipsilateral hemiscrotectomy. The prognosis is relatively good compared to other types of pretesticular sarcomas. Continuous surveillance is always necessary due to the risk of recurrence. The role of chemotherapy and retroperitoneal lymph node dissection remains controversial.
Acknowledgement
None.
Conflict of Interest
None.
References
- John T, Portenier D, Auster B, Mehregan D, Drelichman A, et al. (2006) Leiomyosarcoma of scrotum-case report and review of literature. Urology 67(2): 424.e13- 424.e15.
- Chiodini S, Luciani LG, Cai T, Molinari A, Morelli L, et al., (2015) Unusual case of locally advanced and metastatic paratesticular liposarcoma: a case report and review of the literature. Arch Ital Urol Androl 87(1): 87- 89.
- Khoubehi B, Mishra V, Ali M, Motiwala H, Karim O (2002) Adult paratesticular tumors. BJU int 90 (7): 707-715.
- Zahm SH, Fraumeni JF (1997) The epidemiology of soft tissue sarcoma. Semin Oncol 24(5): 504-514.
- Raza M, Vinay HG, Ali M, Siddesh G (2014) Bilateral paratesticular liposarcoma-a rare case report. J Surg Tech Case Rep 6(1): 15-17.
- Pănuş A, Meşină C, Pleşea IE, Drăgoescu PO, Turcitu N, et al. (2015) Paratesticular liposarcoma of the spermatic cord: A case report and review of the literature. Rom J Morphol Embryol 56(3): 1153-1157.
- Schoonjans C, Servaes D, Bronckaers M (2016) Liposarcoma scroti: A rare paratesticular tumor. Acta Chir Belg 116(2): 122-125.
- Dayron Rodríguez, Aria F Olumi (2012) Management of spermatic cord tumors: a rare urologic malignancy, Ther Adv Urol 4(6): 325-334.
- Vukmirović F, Zejnilović N, Ivović J (2013) Liposarcoma of the paratesticular tissue and spermatic cord: A case report. Vojnosanit Pregl 70(7): 693-696.
- Khandekar MJ, Raut CP, Hornick JL, Wang Q, Alexander BM, et al. (2013) Paratesticular liposarcoma: Unusual patterns of recurrence and importance of margins. Ann Surg Oncol 20(7): 2148-2155.
- Coleman J, Brennan MF, Alektiar K, Russo P (2003) Adult spermatic cord sarcomas: management and results. Ann Surg Oncol 10(6): 669-675.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.