Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Pneumothorax as First Evidence of Unknown Lymphangioleiomyomatosis
*Corresponding author:Dario Familiari, Medical Doctor of Thoracic Surgery of Gaetano Martino Hospital University of Messina, Italy.
Received: January 22, 2024; Published: January 24, 2024
DOI: 10.34297/AJBSR.2024.21.002826
Keywords: Pneumothorax, Lymphangioleiomyomatosis, Pleurodesis
Introduction
Lymphangioleiomyomatosis (LAM) is a rare disorder that causes cystic diseases in the lungs. It is frequently associated with renal angiomyolipomas (Sporadic form) (S-LAM) [1]. Exists also a rare condition characterized by presence of Tuberous sclerosis (TSC-LAM) [1]. Individuals affected by LAM are typically female of reproductive ages [2]. S-LAM may be unknown, and the first symptom may be due to development of pneumothorax [2]. We report a case of a 33-year-old woman with large right pneumothorax (first episode) and unknown LAM.
Case Presentation
TA 33 year-old woman without past medical history, presented to the emergency department with right chest pain, cough and dyspnea that occurred suddenly while she worked (psychologist). The patient did not report similar episodes, recent trauma or lung disease.
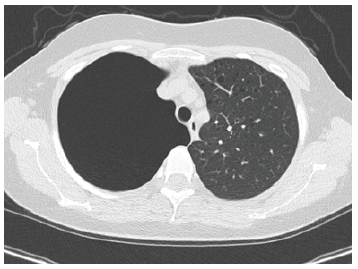
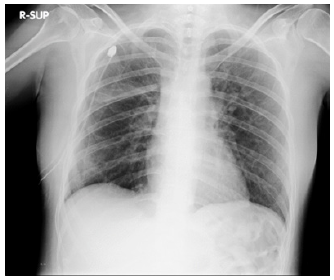
After ECG (normal sinus rhythm) and routine biochemical profiles (within normal limits) was subjected before to chest X-ray (large right-sided pneumothorax) and then to CT-scan to investigate secondary causes of pneumothorax which showed innumerable thin-walled cysts throughout both lungs (Figures 1,2) and angiomyolipoma in the left kidney.
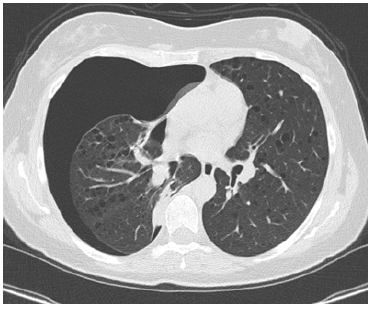
Figure 2: Ct of the chest showing multiple thick walled cysts located throughout both lung parenchyma.
Drainage (24 Fr) was placed in emergency and after three days the patient underwent to right video assisted thoracoscopy (Figure 3) with small wedge resection of the lower lobe where air-leak persisted (confirming the pathological diagnosis of LAM) and chemical pleurodesis with talc. After chest x-ray (two day after VATS) (Figure 4) showed complete lung re-expansion, we removed the drainage.
The patient was discharged the day after without noted post-operative complications. The patient was seen by her pulmonologist three months after the operation and her clinical status was stable without shortness of breath or chest pain. Therapy with sirolimus was started after pathological diagnosis of LAM (Figures 1-4).
Discussion
LAM is a rare disease characterized by diffuse cystic changes in the lungs resulting from destructive proliferation of smooth muscle- like or LAM cells. It is often undiagnosed.
Altough the true origin of LAM cells is undetermined, there are two plausible hypotheses. The first theory proposes that LAM cells are either of airway or vascular origin. Another model suggests that LAM cells originate from angiomyolipoma in the kidney and are transported to the lungs by means of neoplastic dissemination.
LAM exists in two main forms: the first is associated with the genetic disorder tuberous sclerosis complex (TSC-LAM), a condition characterized by hamartomatous lesions in the brain, heart, lungs and liver; and the second is the sporadic form (S-LAM). Overall, the majority of patients with LAM are sporadic (85%) and occur primarily in women of reproductive ages. Both TSC-LAM and S-LAM are associated with a mutation in either TSC1 or TSC2 gene, causing a loss of function in the corresponding gene products, namely hamartin (TSC1) and tuberin (TSC2) [1,2].
LAM is characterized by cystic lung disease resulting in progressive dyspnea, renal angiomyolipoma and lymphatic complications. Pneumothorax occurs frequently (70%) and definitive management pleurodesis is recommended as the risk of recurrence is high [3].
We presented a case of a woman without past medica history that after sudden chest pain went to the emergency department where was submitted to chest X-ray and CT-scan with diagnosis of pneumothorax and cystic disease of the lungs and renal angiomyolipoma.
While the radiological evidence was suggestive of LAM, we preferred to do a small wedge resection of the lung because there was a persistent air leak and for certainty of the diagnosis because the appearance of diffuse pulmonary cysts indicates possible LAM but many conditions can mimic the pathology including pulmonary Langerhans cell histiocytosis, emphysema, follicular bronchiolitis, lymphoid interstitial pneumonia and advanced interstitial lung disease [2,4]. Chemical pleurodesis with talc completed the procedure. After one year the patient had no further episodes of pneumothorax and is in therapy with sirolimus with follow-up from her pulmonologist every six months.
Conclusion
Pneumothorax can be often the first manifestation of unknown LAM. In the presence of a persistent air-leak, we prefer to do a small resection of the lung also for certainty of the diagnosis because many conditions can mimic LAM. Chemical pleurodesis with talc must complete the procedure in VATS to avoid recurrent pneumothorax.
Acknowledgement
None.
Conflict of Interest
None of the authors identify any conflict of interest.
References
- Sathirareuangchai S, Shimizu D, Vierkoetter KR Hawaii (2020) Pulmonary Lymphangioleiomyomatosis: A Case Report and Literature Review. J Health Soc Welf 79(7): 224-229.
- O Mahony AM, Lynn E, Murphy DJ, Fabre A, McCarthy C, et al. (2020) Lymphangioleiomyomatosis: a clinical review. Breathe (Sheff) 16(2): 200007.
- Odak M, Anandani K, Rogers PJ (2020) Lymphangioleiomyomatosis Presenting as Recurrent Pneumothorax. Cureus 12(10): e11102.
- Ukponmwan O, Gorantla A, Patel KH, Gabutan E, Zhonghua L, et al. (2023) Spontaneous Pneumothorax in a Young Female With Lymphangioleiomyomatosis. Cureus 15(9): e45413.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.