Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Spontaneous Bladder Rupture in ER Settings; 2 Case Reports And Management Algorithm
*Corresponding author: Dalati M Fadi, Deputy head of clinic of urology department of CHU Saint-Pierre, Belgium.
Received: December 22, 2024; Published: January 03, 2024
DOI: 10.34297/AJBSR.2024.21.002793
Abstract
Spontaneous bladder rupture, a seldom seen occurrence in the emergency room, poses diagnostic challenges and may lead to significant complications if not promptly identified and treated. We present two cases of spontaneous bladder rupture associated with alcohol intoxication. The purpose of this article is to shed light on these occurrences and suggest an algorithm for improved and expedited detection and management.
Introduction
Bladder rupture caused by blunt trauma represents a life-threatening and infrequent condition, carrying a mortality rate that can soar up to 50% [1]. Frequently, it remains undiagnosed initially, leading to severe complications. Various predisposing factors contribute to this rupture, including chronic bladder inflammation, excessive alcohol consumption leading to altered sensitivity, radiotherapy, urinary retention (such as due to obstructive pathologies), or neurogenic bladder resulting from increased intravesical pressure [2]. While cystography remains the gold standard, CT-scan imaging is more commonly employed in the emergency room (ER) due to its utility in differentiating diagnoses associated with acute abdominal conditions [3].
Case Presentation
Case1
This case involves a 52-year-old homeless Caucasian male who presented to the emergency room following a fall on an escalator in a subway station, during which he did not experience loss of consciousness. The patient mentioned consuming 10 beers on the night of the incident and did not report any warning signs before the fall.
Post-fall, the patient started experiencing progressively worsening abdominal pain, despite taking analgesics (paracetamol and tramadol), accompanied by episodes of nausea and vomiting (3 to 4 times). He complained of escalating abdominal discomfort and distention. Additionally, he reported a headache but without sensitivity to sound or light.
From a urological perspective, he reported experiencing voiding difficulties, polyuria, and overflow incontinence persisting for over 5 months. Upon arrival at the ER, the patient developed significant hematuria.
His medical history was largely unremarkable, except for alcohol addiction and a past heroin addiction for which he had been receiving methadone treatment for 30 years.
During assessment, he exhibited normal body temperature, heart rate, and blood pressure. Although he complained of acute abdominal pain, there were no indications of abdominal trauma, prompting consultation with a general surgeon. Laboratory tests revealed a normal white blood cell count of 9.07×10^3/ml, a C-reactive protein (CRP) level of 13.7mg/L, a creatinine level of 2.93mg/ dl, creatine kinase (CK) of 234UI/L, lactate dehydrogenase (LDH) of 287UI/L, and an ethanol level of 2.2g/L. His baseline creatinine 5 months earlier was recorded at 0.74mg/dl. A Foley catheter was inserted, yielding 2.5 L of visible hematuria.
After a non-contrast CT-scan, findings indicated the presence of substantial free fluid with evidence of hemoperitoneum within the pelvic cavity. Additionally, the bladder displayed an anomalous appearance characterized by thickened and indistinct contours (CTscan 1), indicative of a potential bladder rupture following blunt trauma. To confirm this diagnosis, exploratory laparoscopy was deemed necessary. Furthermore, the scan identified bilateral ureterohydronephrosis, observing the right renal pelvis measuring 27 mm and the left measuring 22mm.
An exploratory laparoscopy was conducted by both a general surgeon and a urologist, suspecting a bladder rupture. During the procedure, an extensive, decompensated bladder was discovered, exhibiting significant adherence to the anterior abdominal wall. This was accompanied by the presence of an intraperitoneal urinoma. Consequently, a decision was made to transition to a laparotomy. The procedure involved the release of bladder adhesions from the anterior abdominal wall, followed by a longitudinal incision made on the anterior bladder wall. A 2 cm perforation in the bladder was identified at the level of the right posterior wall (Figure 1).
The posterior bladder defect and the anterior wall were closed in two layers using watertight Vicryl 0 sutures. Following this, a thorough washout was carried out, and 2 JP drains along with a Foley catheter were inserted.
Following the surgery, the patient experienced acute renal failure, which swiftly resolved. The ureterohydronephrosis improved upon removal of the left drain and discontinuation of cefazolin antibiotic prophylaxis after 2 days. Despite this, hematuria persisted
while the Foley catheter remained in place. A control ultrasound on the third day post-operation revealed ongoing enlargement of the left pyelocaliceal system without significant hydronephrosis. The right JP drain was removed on the fourth day post-operation, followed by the Foley catheter on the sixth day. Although a follow-up retrograde cystography was planned for two weeks later, it couldn’t be carried out due to COVID-related restrictions.
Case 2
The second case involves a 46-year-old Caucasian male who presented to the emergency department due to alcohol intoxication. During his time in the ER, he experienced vomiting and altered consciousness. An immediate resuscitation process was swiftly initiated until the patient achieved hemodynamic stability. An abdominal scan was conducted, initially intended to focus on the bladder, revealing an unidentified mass of unknown origin within the bladder and suspected ascites surrounding the liver. (cf. CT-scan 2).
The urologist wasn’t sought for consultation, and a Foley catheter wasn’t inserted.
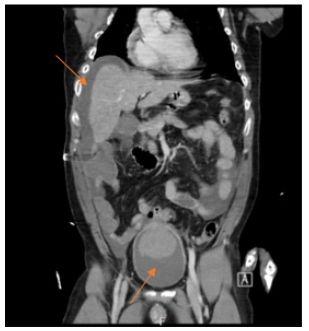
Figure 3: CT-scan 2: arrow 1 pointing at liquid around the liver and arrow 2 pointing at a hyper-density in the bladder.
Subsequently, the patient was transferred to the intensive care unit for continued management, and the decision against using a urinary catheter persisted due to concerns about the possibility of the mass being tumorous. Examination of the fluid collection surrounding the liver was carried out.
The patient remained unconscious and developed anemia (Hb8.5g/dL) along with severe renal insufficiency (creatinine 3.99mg/dL and GFR 17mL/min/1.73m²) accompanied by hyperkalemia (6.6mmol/L).
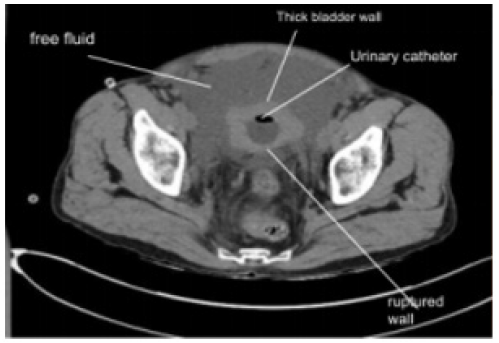
On the following day, a second abdominal scan with contrast was performed, prompting the consultation of a urologist at last. Upon further evaluation of the scan images by the urologist, the diagnosis of bladder rupture was confirmed (CT-Scan 3&4).
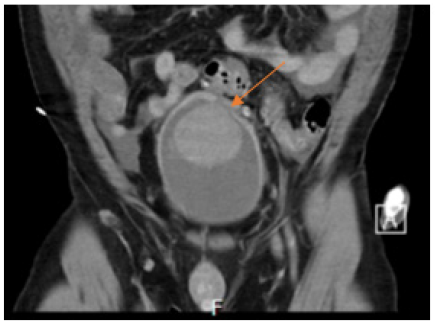
Figure 4: CT-scan 3: arrow pointing at the bladder rupture and hematoma in the bladder next to the burst.
Subsequently, the analysis of the peritoneal fluid confirmed the presence of a urinoma, exhibiting notably high levels of creatinine at 14.84mg/dL.
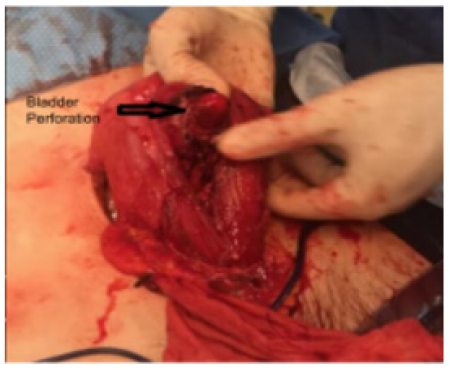
The patient underwent an exploratory laparotomy in the operating room, revealing a substantial intraperitoneal hematoma, which was evacuated. Additionally, a 10-cm defect of the bladder dome was identified and repaired using two-layer running overlock sutures. At the end of the surgery, a JP drain and a Foley catheter were inserted.
Remarkably, the renal insufficiency and hyperkalemia resolved swiftly within 48 hours. The Foley catheter was removed two weeks post-operation.
Discussion
Bladder ruptures commonly result from traumatic events. Spontaneous bladder rupture (SBR) is an extremely rare occurrence, affecting only 1 in 126,000 individuals, and even rarer in cases where patients lack predisposing factors such as bladder cancer, exposure to radiation therapy, or neurogenic bladder [4]. The symptoms often lack specificity, leading to misdiagnosis, delayed treatment, and heightened mortality rates [5].
In exceptional instances, bladder perforation may spontaneously arise due to increased intravesical pressure caused by a high intake volume, along with diuretic effects that reduce voiding, or weakened bladder wall strength, frequently observed in cases involving alcohol intoxication [7-12]. Factors that elevate intravesical pressure or compromise bladder wall strength should be considered as they heighten the risk of spontaneous bladder rupture.
Patients with bladder perforation initially present with nonspecific abdominal pain. Diagnosis in cases of spontaneous rupture without an identifiable cause, as seen in our patients, can be complex and delayed. Symptoms may encompass macroscopic hematuria, suprapubic pain, dysuria, urinary difficulties, peritonitis, hemodynamic instability, acute renal failure, and sepsis [6-15].
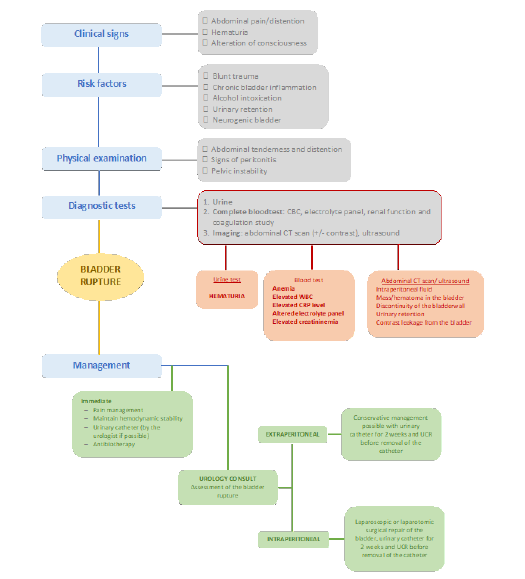
Accurate diagnosis often occurs during surgical intervention performed by the surgical team, akin to our initial patient case. Hence, we aimed to develop an algorithm to streamline patient management in emergency settings (cf. algorithm).
Patients presenting with acute abdominal pain alongside identifiable risk factors and suspicious findings upon physical examination should undergo, at a minimum, urinalysis, and blood tests. In the event of hematuria detected in the urine test, abdominal imaging becomes imperative. Following initial pain management, consideration should be given to seeking urological consultation for image visualization and potential insertion of a urinary catheter upon suspicion or confirmation of a bladder rupture. Initiation of prophylactic antibiotic therapy can be considered to forestall potential infections and septic complications. If an intraperitoneal bladder rupture is identified, it is essential to contemplate laparoscopic or laparotomic interventions for treatment.
Conclusion
Despite its rarity as a cause of acute abdominal pain, spontaneous bladder rupture should be included in the list of potential differential diagnoses. We aim to effectively raise awareness regarding spontaneous bladder rupture, facilitating early detection and appropriate management to optimize outcomes for these patients (Figure 2).
References
- Sawalmeh H, Al Ozaibi L, Hussein A, Al Badri F (2015) Spontaneous rupture of the urinary bladder (SRUB); A case report and review of literature. Int J Surg Case Rep 16: 116‑11
- Mitchell T, Al Hayek S, Patel B, Court F, Gilbert H (2011) Acute abdomen caused by bladder rupture attributable to neurogenic bladder dysfunction following a stroke: a case report. J Med Case Reports 5(1): 254.
- Kivlin D, Ross C, Lester K, Metro M, Ginsberg P (2015) A Case Series of Spontaneous Rupture of the Urinary Bladder. Curr Urol mai 8(1): 53‑5
- Perdoncin M, Ezeh E, Ugonabo O, Robertson R, Gilkerson C (2023) A Busted Sac: A Case of Spontaneous Bladder Rupture Secondary to Acute Urinary Retention in a Healthy Middle-Aged Male. J Investig Med High Impact Case Rep 11: 232470962211482.
- Bartholomew R, Ahmeti M (2021) A Case of Idiopathic Recurrent Spontaneous Bladder Rupture. De Nardi P, é Case Rep Surg 30 août 2021: 1‑4.
- Coccolini F, Moore EE, Kluger Y, Biffl W, Leppaniemi A, et al (2019) Kidney and uro-trauma: WSES-AAST guidelines. World J Emerg Surg 14(1): 54.
- Huang Y, Zhou Z, Li Y, Wang X (2022) Spontaneous rupture of the urinary bladder due to binge drinking: A possibly avoidable accident. Asian J Surg 45(12): 2844‑284
- Zhang X, Zhang G, Zhang L, Sun C, Liu N, et al (2017) Spontaneous rupture of the urinary bladder caused by eosinophilic cystitis in a male after binge drinking: A case report. Medicine (Baltimore) 96(51): e9170.
- Elsaharty SA, Tjong E and Gadiok G (2020) Spontaneous Intraperitoneal Urinary Bladder Rupture Due to Alcohol-Intoxication. Urology 145: e12‑6
- Muneer M, Abdelrahman H, El Menyar A, Zarour A, Awad A, et al (2015) Spontaneous Atraumatic Urinary Bladder Rupture Secondary to Alcohol Intoxication: A Case Report and Review of Literature. Am J Case Rep 16: 778‑781
- Dooldeniya MD, Khafagy R, Mashaly H, Browning AJ, Sundaram SK, et al (2007) Lower abdominal pain in women after binge drinking. BMJ 335(7627): 992‑993
- Daignault MC, Saul T, Lewiss (2012) RE Bedside ultrasound diagnosis of atraumatic bladder rupture in an alcohol-intoxicated patient: a case report. Crit Ultrasound J 4(1): 9.
- Mouracade P, Saussine C (2008) La cystite interstitielle en 2008. Prog En Urol 18(7): 418‑4
- Verhamme KMC, Sturkenboom MCJM (2008) Stricker BHC, Bosch R. Drug-Induced Urinary Retention: Incidence, Management and Prevention. Drug Saf 31(5): 373‑388
- Grover S, Srivastava A, Lee R, Tewari AK, Te AE (2011) Role of inflammation in bladder function and interstitial cystitis. Ther Adv Urol 3(1): 19‑33




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.