Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Surgical Approach for Multiple Indeterminate Liver Lesions: A Case Report
*Corresponding author:Atta Nawabi, The University of Kansas Medical Center, Department of Surgery, 3901 Rainbow Boulevard, Kansas City, KS 66160, USA.
Received: February 22, 2024; Published: February 27, 2024
DOI: 10.34297/AJBSR.2024.21.002871
Abstract
The incidence of liver lesions has increased with the widespread use of cross-sectional imaging in recent years. It is important to differentiate benign lesions from malignant disease. Hepatic lesions have recognizable radiographic characteristics on triphasic CT or MRI. I imagining or clinical picture is unclear a tissue sample for definitive diagnosis should be obtained. Currently the gold standard is percutaneous needle biopsy generally performed by interventional radiology. In unique cases, an open approach may be indicated. Here, we present a case of a patient with multiple liver lesions identified on imaging and symptoms concerning malignancy. She had undergone multiple percutaneous needle biopsies which were all inconclusive. The decision was made to perform an open excisional liver biopsy with periportal lymphadenectomy.
Keywords: Liver lesions, Multiple liver lesions, Metastatic liver lesions, Liver biopsy
Introduction
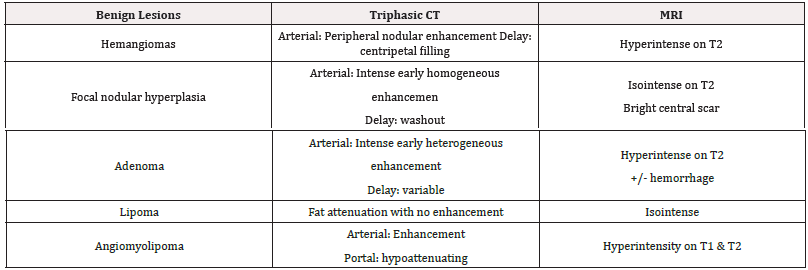
When a solid hepatic lesion is identified, it is important to differentiate a benign lesion from a malignant one [1]. Common benign liver lesions include hemangiomas, focal nodular hyperplasia, and hepatic adenomas with less common lesions being lipomas and angiomyolipoma. These lesions have very specific radiographic findings on triphasic CT and MRI as outlined in Table 1, and if clearly defined they require no additional workup [2]. When assessing multiple liver lesions, underlying hepatic disease should be considered. Multiple liver lesions in a non-cirrhotic patient usually indicate liver metastasis whereas multiple liver lesions in a cirrhotic is more likely diffuse hepatocellular carcinoma [3]. Other less common hepatic lesions include lymphoma, with 40% of hepatic lymphomas being diffuse and hepatic tuberculosis. If the lesion is clearly defined on cross-sectional imaging, then a biopsy is not always required. However, in cases where there is uncertainty, questionable radiographic features or concern for malignancy then a biopsy should be obtained [4]. The current gold standard is a percutaneous needle biopsy, generally performed by interventional radiology; however, several alternative approaches exist including plugged biopsy, transvenous, laparoscopic and open techniques.
Presentation of Case
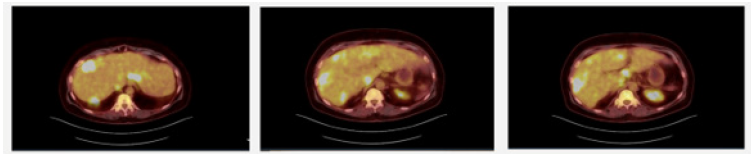
We present a 53-year-old female with diffuse hepatic lesions and widespread lymphadenopathy who was referred to Hepato- pancreato-biliary clinic for evaluation after several failed and inconclusive needle biopsies. She originally presented to her primary care physician for evaluation due to a 4-month history of fevers, chills, drenching night sweats, fatigue, postprandial pain and 40-pound weight loss. Routine labs were unremarkable besides thrombocytosis. CT abdomen and pelvis demonstrated porta hepatis lymphadenopathy and multiple liver lesions (Figure 1). On PET scan she was found to have innumerable masses in the liver and axillary, mediastinal, porta hepatis and retroperitoneal lymphadenopathy with FDG uptake concerning metastatic disease (Figure 2). She was sent to interventional radiology for CT-guided biopsy which revealed necrotizing granulomatous inflammation. Auramine-protamine and AFB staining were negative. She was referred to infectious disease, but extensive workup was negative. Repeat IR biopsy showed fibroinflammatory cells with chronic lymphoplasmacytic and histiocytic inflammation. Given numerous inconclusive results with percutaneous biopsies she was referred to surgery clinic by infectious disease for excisional biopsy. Given her concerning symptoms, lymphoma was also a consideration making surgery a reasonable approach for excisional biopsy with lymphoma protocol. She was seen and evaluated in clinic where we discussed laparoscopic vs an open approach and she elected to undergo an open biopsy. Intraoperatively she was found to have innumerable liver lesions and diffuse porta hepatis lymphadenopathy. Multiple excisional biopsies were obtained from hepatic segments 4, 5, and 6. These were sent for frozen section and permanent. Some of the lesions were sent for microbiology and others sent for cultures, including TB, fungal, anaerobic and aerobic. The hilar lymph nodes were sent for per lymphoma protocol. The frozen section came back as chronic inflammation, non-diagnostic. Permanent biopsies all revealed necrotizing granulomatous inflammation. Cultures were negative for infectious organisms.
Discussion
Liver lesions are incidentally found with more frequency given widespread use of cross-sectional imaging. While most lesions are benign, it is important to differentiate these from malignant lesions, including hepatic cellular carcinoma and metastatic disease. If a hepatic lesion is identified, it should undergo proper workup starting with triphasic CT and MRI. Benign liver lesions have specific radiographic features and rarely require additional imaging or workup. If there are multiple liver lesions as there is concern for malignancy, more information should be gathered. In cirrhotic patient hepatic cellular carcinoma should be top on the differential whereas in non-cirrhotic patients, metastatic disease is more likely. If there is high suspicion for malignancy then an alpha-fetoprotein, serum carcinoembryonic antigen and CA19-9 should be obtained. If the lesion is clearly defined on cross-sectional imaging and clinically correlated, then a biopsy is often not indicated. However, in cases where there is uncertainty or questionable features a biopsy can be obtained to rule out malignancy. Currently the gold standard is percutaneous needle biopsy generally performed by interventional radiology; however, plugged, transvenous, laparoscopic and open techniques are also well described. A plugged biopsy is similar to a percutaneous biopsy; however, it is used when a larger specimen is needed as the tract is then “plugged” with thrombin to reduce risk of bleeding [5]. A trans jugular approach is particularly useful in cirrhotic or patients at a high risk of bleeding [6]. Laparoscopic biopsy is unique as it allows for direct visualization and targeted liver biopsies. This approach is useful in patients that have had prior inconclusive results from other methods. It is also useful if metastasis is suspected as it can aid in identifying a primary source. In complex or unique situations that have failed prior minimally invasive options, an open surgical approach should be considered. As with the case presented, patients that have concerning symptoms and in need of multiple large excisional biopsies with hilar lymphadenectomy, an open approach should be considered as it allows full visualization, access to multiple segments for adequate sampling, and ability to retrieve large full thickness biopsies and control bleeding.
Conclusion
While imaging and clinical context may narrow the differential, it is important to obtain tissue samples for definitive diagnosis, especially when there is high suspicion of malignancy. For biopsies that are not concordant or indeterminate, additional biopsy methods should be utilized. In this case, the initial presentation and imaging appeared to be metastatic in nature. Final pathology however has guided additional work up to include infectious and autoimmune etiology.
Acknowledgement
None.
Conflict of Interest
None.
References
- Assy N, Nasser G, Djibre A, Beniashvili Z, Elias S, et al. (2009) Characteristics of common solid liver lesions and recommendations for diagnostic workup. World J Gastroenterol 15(26): 3217-3227.
- Horton KM, Bluemke DA, Hruban RH, Soyer P, Fishman EK (1999) CT and MR imaging of benign hepatic and biliary tumors. Radiographics 19(2): 431-451.
- Cherif Boutros, Steven C Katz, N Joseph Espat (2010) Management of an Incidental Liver Mass, Surgical Clinics of North America, 90(4): 699-718.
- Algarni AA, Alshuhri AH, Alonazi MM, Mourad MM, Bramhall SR (2016) Focal liver lesions found incidentally. World J Hepatol 8(9): 446-451.
- Singhal S, M D Pradeep, Inuganti S, Botcha S, Deepashree DT, et al. (2021) Percutaneous ultrasound-guided plugged liver biopsy - a single-centre experience. Pol J Radiol 86: e239-e245.
- Behrens G, Ferral H (2012) Transjugular liver biopsy. Semin Intervent Radiol 29(2):111-117.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.