Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Vaginal Metastasis from Breast Cancer: A Case Report and Review of the Literature
*Corresponding author:Khadija Hinaje, Department of medical oncology, Hassan II University Hospital, University Sidi Mohamed Ben Abdellah, Fez, Morocco.
Received: February 06, 2024; Published: February 09, 2024
DOI: 10.34297/AJBSR.2024.21.002856
Abstract
Background: Breast cancer metastasis accounts for the majority of deaths from breast cancer. This neoplasm frequently relapses at distant sites such as bone, lung, brain and liver but rarely in the lower female genital tract.
Case Presentation: A 70-year-old woman admitted to Department of Medical Oncology for a locally advanced breast cancer. Extensive work-up revealed isolated vaginal mass compatible with breast cancer metastasis. The patient was a candidate for neoadjuvant chemotherapy followed by surgery of both lesions simultaneously.
Conclusion: This case report shows the importance of histopathological examination to achieve an accurate diagnosis. Isolated vaginal metastases are an indication for surgical resection. Therapeutic management must be decided in multidisciplinary consultation meetings.
Keywords: Vaginal metastasis, Lobular carcinoma, Breast cancer, Case report
Introduction
Breast cancer is the most common type of cancer and the primary cause of cancer mortality in women [1]. The majority of deaths from breast cancer are not due to the primary tumor itself but are the result of metastasis to other organs in the body [2]. The neoplasm frequently relapses at distant sites such as bone, lung, brain and liver [3]. Metastases to the genital organs are less common, with the ovaries being the common site of metastases to the genital organs, but the vagina is rare [4]. We present a case of vaginal metastasis in a patient with previously diagnosed breast cancer.
Case Presentation
In February 2021, a 70-year-old woman, with a 7-year history of hypertension and dyslipidemia, was referred to our Department of Medical Oncology for a locally advanced breast cancer cT4d N0 Mx. The patient underwent mammography and a biopsy revealed, at the histology and immunohistochemical examination, an inva sive lobular carcinoma grade I of Scarff-Bloom-Richardson (SBR), with loss expression of E-Cadherin. In addition, the tumor presented high expression of Estrogen Receptor (ER): 100% and Progesterone Receptor (PR): 100 %, however, Human Epidermal growth factor Receptor 2 (HER2) was negative (score 0).
A total-body Computed Tomography (CT) examination highlighted, other than breast lump and subcentimetric lymphatic findings, a hypodense formation, of about 55 mm, at the level of the uterine cavity. We completed a pelvic ultrasound that revealed a slightly enlarged uterus measuring 90x60 mm, with endometrial thickening of 40 mm very suspicious of malignancy.
An operative hysteroscopy was performed, and numerous biopsies were taken. Endometrial biopsies were negative, while the biopsy performed in the vagina (Figure 1) highlighted a suspicious cells expressing cytokeratin 7, E-Cadherin was negative, ER expression was 30% positive, RP was 50% positive and HER 2 was negative (score 0), compatible with breast carcinoma as a metastasis from the patient’s primary tumor (Figure 2).
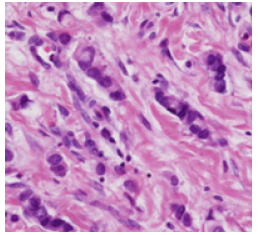
Figure 1: Hematoxylin and eosin-stained sections (x 400) of metastatic breast invasive lobular carcinoma in the vagina.
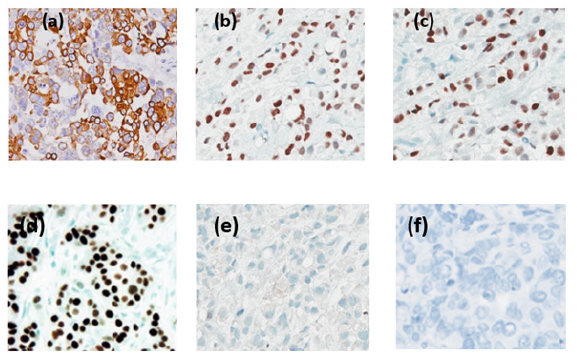
Figure 2: Immunohistochemical study of vagina biopsy that is positive for CK7 (a), GATA 3 (b), ER (c), PR (d), and negative for E-cadherin (e) and HER2 (f).
We took charge of the case and gave indications to start neoadjuvant chemotherapy with 4 AC60 followed by 12 paclitaxel weekly. Four months after having begun the chemotherapy, the patient underwent an evaluation CT showing overall disease stability according to RECIST criteria. The pelvic Magnetic Resonance Imaging (MRI) revealed an endocervical uterine lesion process measuring 32 mm without parametrial invasion, with no sub peritoneal or lumbo-aortic pelvic lymphatic extension.
The case was discussed at a multidisciplinary meeting. It went out with the continuation of neoadjuvant treatment, and then proceed with surgery of both lesions simultaneously. The patient completed her taxane therapy for breast cancer, but as soon as his treatment ends, she manifested a brutal worsening of dyspnea, which required her transfer to the emergency, where she died of pulmonary embolism (Figures 1,2).
Discussion
The common sites of distant metastases from breast cancer are lung, bone, liver, and supraclavicular lymph nodes [4]. Metastases to the female genital tract from breast cancer are unusual and represents less than 1% [5]. It’s most often involves the ovaries, but the vagina is rare.
Mazur and al [6] analyzed the origin of metastasis in the female genital tract (Table 1). According to those authors, only 149 out of 325 cases presented extragenital primitivity. In that series, of the twenty vaginal secondary tumors, only three (15%) originated from breast cancer (Table 1).
The lobular histotype of breast cancer seems to metastasize to the genital tract more frequently than ductal tumors [7], probably for hematogenous dissemination. Most primary vaginal cancer cases are squamous cell carcinomas [8], and other histological subtypes, such as adenocarcinomas, are extremely rare [9]. Therefore, histopathological examination is obviously essential for an accurate diagnosis. In other words, when the histopathological examination of a vaginal tumor shows an adenosquamous carcinoma, the possibility of a metastasis from the breast must be considered and further analyzed.
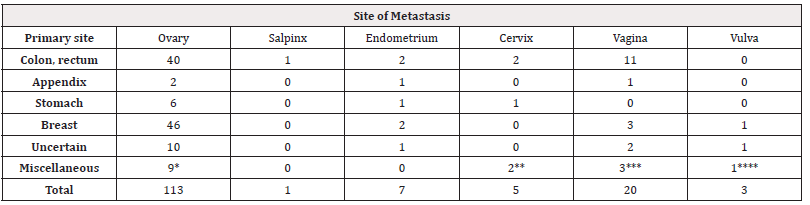
Table 1: Female genital metastasis from extragenital tumors (6).
Note*: Total number of tumors: 149. *Jejunal adenocarcinoma (1), ileal carcinoid (1), gallbladder (1), pancreas (3), lung (1), kidney (1), rhabdomyosarcoma of parotid (1). **Melanoma of thoracic skin (1), lung (1). ***Bladder (2), kidney (1). ****Kidney (1).
Regarding clinical signs, vaginal metastases are frequently asymptomatic. Clinical presentations include vaginal bleeding, vaginal masses, vaginal discharge, vaginal staining, and perineal discomfort. MRI evaluation is very useful in identifying a vaginal lesion and differentiating between adenocarcinoma from squamous cell carcinoma. Adenocarcinomas usually have a T2w hyperintense signal, whereas squamous cell carcinomas appear with T2w intermediate and low T1w (T1-weighted) signals on MRI [9].
Data regarding the behavior and treatment of vaginal metastasis is limited. Treatment options include surgical resection, radiotherapy, and chemotherapy, both monotherapy and combination therapies [10]. Bellati and al have reported the first case of an isolated vaginal metastasis from breast cancer treated by surgery [11]. Twelve months later, the patient is still free from disease. It showed that surgery could be considered a valid option for the treatment of isolated vaginal metastasis of breast cancer. A combination of surgical resection and radiotherapy are commonly used for patients with isolated vaginal metastases [12]. Systemic therapy is used for patients with extensive metastases. Therefore, the existence of vaginal metastasis would not have implied a different approach in terms of systemic therapy, considering the locally advanced stage of the primitive tumor at the time of diagnosis.
Conclusion
Vaginal metastasis from breast cancer is a rare entity. Histopathological examination is crucial to achieve an accurate diagnosis. Isolated vaginal metastases are an indication for surgical resection. Given the complexity of these cases, therapeutic management must be decided in multidisciplinary consultation meetings.
References
- Jemal A, Bray F, Center MM, Ferlay J, Ward E, et al. (2011) Global cancer statistics. CA Cancer J Clin 61: 69-90.
- Weigelt B, Peterse JL, van‘t Veer LJ (2005) Breast cancer metastasis: markers and models. Nat Rev Cancer 5(8): 591-602.
- Cheng YC, Naoto T Uemo (2011) Improvement of survival and prospect of cure in patients with metastatic breast cancer. Breast cancer 19(3): 191-199.
- Geng Z, Zhang Q, Jia P, Miao J, Lin Q (2022) Severe vaginal bleeding due to vaginal metastasis from renal cell carcinoma with inferior vena cava tumor thrombus: A case report. Med(Baltim) 101(3): e28586.
- Sanuki Fujimoto N, Takeda A, Amemiya A, Ofuchi T, Ono M, et al. (2008) Pattern of tumor recurrence in initially nonmetastatic breast cancer patients: distribution and frequency of metastases at unusual sites. Cancer 113(4): 677-682.
- Kong M, Jin J, Cai X, Shen J, Ma D, et al. (2017) Characteristics of lymph node metastasis in resected adenosquamous lung cancer. Medicine (Baltimore) 96(48): e8870.
- Borst MJ, Ingold JA (1993) Metastatic patterns of invasive lobular versus invasive ductal carcinoma of the breast. Surgery 114(4): 637-641.
- Yang J, Delara R, Magrina J, Magtibay P, Langstraat C, et al. (2020) Management and outcomes of primary vaginal Cancer. Gynecol Oncol 159(2): 456-463.
- Sadatomo A, Koinuma K, Horie H, Lefor AK, Sata N (2015) An isolated vaginal metastasis from rectal cancer. Ann. Med. Surg. (Lond.) 5: 19-22.
- Korkmaz M, Eryilmaz MK, Kerimoglu U, Karaagac M, Demirkiran A, et al. (2021) Vaginal metastasis in solid tumours: our four cases and review of the literature. J Egypt Natl Canc Inst 33(1): 3.
- Bellati F, Palaia I, Gasparri ML, Musella A, Panici PB (2012) First case of isolated vaginal metastasis from breast cancer treated by surgery. BMC Cancer 12: 479.
- Benhayoune K, El Fatemi H, El Ghaouti M, Bannani A, Melhouf A, et al. (2015) Vaginal metastasis of pancreatic cancer. Pan Afr Med J 20: 124.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.