Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
A Retrospective Analysis of Clinicopathological Features and Therapeutic Outcomes of Metastatic Kidney Cancer
*Corresponding author: Oumaima Talbi*, Khadija Hinaje, Kaoutar Maadin, Lamiae Amaadour, Karima Oualla, Zineb Benbrahim, Samia Arifi and Nawfel Mellas, A Retrospective Analysis of Clinicopathological Features and Therapeutic Outcomes of Metastatic Kidney Cancer.
Received: April 22, 2024; Published: April 25, 2024
DOI: 10.34297/AJBSR.2024.22.002941
Abstract
Kidney cancer is a primary malignant tumor of the renal parenchyma, with clear cell carcinoma being the most common histological type. At the time of diagnosis, up to 30% of patients have metastatic disease. Kidney cancer is resistant to chemotherapy and radiotherapy, but with the advent of immunotherapy and targeted therapies (anti-angiogenic), the prognosis of metastatic renal cell carcinoma (mRCC) has significantly improved.
The aim of our work is to analyze the different epidemiological, clinical, histoprognostic, and therapeutic aspects of kidney cancer in our context through a retrospective study involving 95 patients with locally advanced or metastatic kidney cancer collected in the medical oncology department of the Hassan II University Hospital in Fez from January 2016 to September 2023.
The average age of our patients was 60 years, ranging from 40 to 65 years, with a male predominance with a sex ratio of 1.3. Discovery was incidental in four patients (4%), and symptomatic in 91% of cases. Metastases were present in all our patients, with the preferred locations of these metastases being lymph node (46%) and pulmonary (23%).
Surgical intervention was performed in 20 patients, with 13% of patients undergoing nephrectomy before the diagnosis of metastatic disease (i.e., those with metachronous metastases). Five patients underwent cytoreductive nephrectomy. None of our patients underwent distant metastasis resection. The Fuhrman grade was specified in 95% of cases, distributed as grade 4 (16.8%), grade 3 (34.7%), grade 2 (38.9%), and grade 1 (9.5%). 36% (34) of patients were at unfavorable risk, 35% (33) at intermediate risk, and 26% (25) at favorable risk according to the IMDC classification of metastatic kidney cancer.
In the first line, 3 (4.5%) patients received systemic treatment based on a combination of immunotherapy such as Pembrolizumab and a VEGFR inhibitor such as axitinib, 37 (49%) received Sunitinib alone, 21 (28%) received Pazopanib, 13 (17%) received Bevacizumab, and 7 (10.4%) were placed under surveillance.
Among patients who progressed (N=55), 54% (N=30) received second-line treatment. The most commonly used second-line treatments were sunitinib (N=11), axitinib (N=7), pazopanib (N=5), bevacizumab (N=5), and everolimus (N=2). The use of these drugs depended on their availability at Hassan II University Hospital.
After a median follow-up of 12 months, the median progression-free survival was 7.2 months (95% CI, 3 to 23), and the median overall survival was 13 months (95% CI, 3.33 to 6.5).
Kidney cancer mortality remains high despite progress; however, the reform of the national healthcare system and the generalization of medical coverage have allowed greater accessibility to new therapies.
Introduction
Kidney cancer is a primary malignant tumor developed from the renal parenchyma. It represents 3% of all malignant tumors in adults and ranks third among urological cancers after prostate and bladder cancer [1,2]. It is characterized by a male predominance, with a sex ratio of about two men to one woman. The median age at the time of kidney cancer diagnosis is 67 years in men and 70 years in women.
Kidney cancer has variable incidence rates according to geographical regions. In Morocco, kidney cancer accounted for 32.7% of urinary system cancers, which represented 1.3% of all cancers recorded in 2020 according to the Global Cancer Observatory [3]. Several risk factors are involved, including smoking, obesity, hypertension, and chronic kidney disease [4]. Additionally, there are various hereditary conditions predisposing to kidney cancer. Approximately 2 to 3% of all renal cell carcinomas (RCC) are hereditary, with several autosomal dominant syndromes described, each with distinct genetic bases and phenotypes, the most common being Von Hippel-Lindau (VHL) disease. Patients with multiple and bilateral lesions and/or other associated disorders should be tested for these germline mutations as their recognition is important.
Kidney cancer is histologically heterogeneous, with various histological types. Clear cell renal cell carcinomas (ccRCC) represent 80% of malignant renal tumors in adults, with the remaining 20% consisting of several histological subtypes with different histological, molecular, and cytogenetic profiles [5]. Papillary and chromophobe RCCs represent 80% of non-ccRCCs.
Its diagnosis has significantly evolved over the past decades, with increasing incidental detection in developed countries. Diagnosis is typically suggested by ultrasound and further investigated by computed tomography, which assesses local invasiveness, potential lymph node involvement, or distant metastases. Magnetic resonance imaging (MRI) can provide additional information on local advancement and venous involvement of the tumor thrombus. Renal tumor biopsy provides histopathological confirmation of malignancy with high sensitivity and specificity.
Management of renal cell carcinomas (RCC) has undergone unprecedented changes. Recent discoveries have renewed interest in targeted therapy and immunotherapy in metastatic RCC.
The aim of this study is to evaluate the clinical, epidemiological, histological, and therapeutic aspects of metastatic kidney cancer at the Hassan II University Hospital Medical Oncology Department in Fes.
To achieve this objective, we will divide this work into two parts, a first part for background information, and a second part where we will present our results before discussing them while relying on literature data.
Patients and methods
Our study is a retrospective analysis involving 95 patients diagnosed with metastatic kidney cancer, collected from the Medical Oncology Department of Hassan II University Hospital in Fez over a seven-year period from January 2016 to September 2023.
The included patients were aged >18 years and had histologically confirmed metastatic kidney cancer. Data collection was conducted from consultation records and patient files. Kaplan-Meier survival analysis was used to determine overall and progression-free survival rates. Cox proportional hazards modeling analysis was employed to compare outcome parameters. A significance level of p<0.05 was used for all tests. Statistical software SPSS version 22 (IBM Corporation, New York, USA) was used for all analyses.
Result
In total, data from 95 cancer patients were reviewed, The age of the patients ranged from 40 to 65 years, with a mean age of 60 years. In our series, there were 53 male patients (56%) and 42 female patients (44%), resulting in a sex ratio of 1.3.
The most common clinical manifestation was lower back pain; specifically, lumbalgia was observed in 64 of our patients, accounting for 67% of cases. Through the study of our series, the general condition data, assessed using the WHO performance status scale, were as follows: 65% had an Eastern Cooperative Oncology Group (ECOG) performance status of 0 to 1, 20% had an ECOG of 2, and 15% had an ECOG of 3.
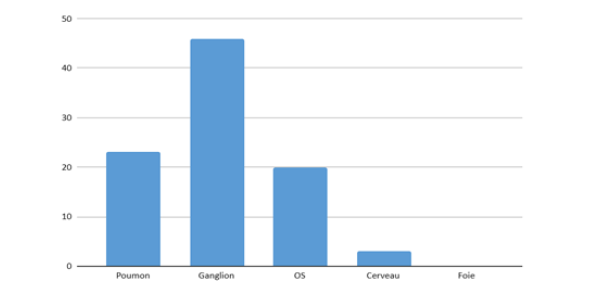
Following this clinical symptomatology, 35 patients underwent renal ultrasound. Radiological staging was based on an extension assessment performed for all patients. It consisted of a thoraco-abdomino-pelvic CT scan with additional cerebral imaging in case of neurological symptoms. At the end of this assessment, distant nodal metastases were identified in 46%, pulmonary metastases in 23% of patients, bone metastases in 20%, and brain metastases in 3% (Figure 1).
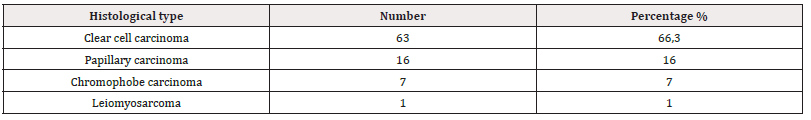
Renal biopsy was performed in 76 patients as they were metastatic from the outset. Twelve cases underwent prior nephrectomy to provide histological evidence of their kidney cancer, 3 underwent extended nephrectomy for hemostatic emergency, and cytoreductive nephrectomy was instituted in 5% of patients. Anatomopathological study revealed a predominance of clear cell renal carcinoma in 63 patients, accounting for 66.3%; papillary carcinoma was found in 16 patients (16%), chromophobe carcinoma in 7 patients (7%), and leiomyosarcoma in one patient. The different histological varieties are listed in (Table 1).
Based on clinical and biological data, three prognostic groups were defined. The majority of patients were classified as intermediate prognosis, accounting for 39% (34), while 31% and 26% of patients were classified as poor and good prognosis, respectively.
On the therapeutic front and in a metastatic setting, whether it occurred de novo or recurred after curative surgical treatment, 75 patients received targeted therapy as monotherapy. Among them, 49% (N=37) were treated with Sunitinib, 28% (N=21) with Pazopanib, and 17% (N=13) with Bevacizumab. The pembrolizumab/axitinib combination was administered as first-line treatment in 4.5% (N=3) of cases.
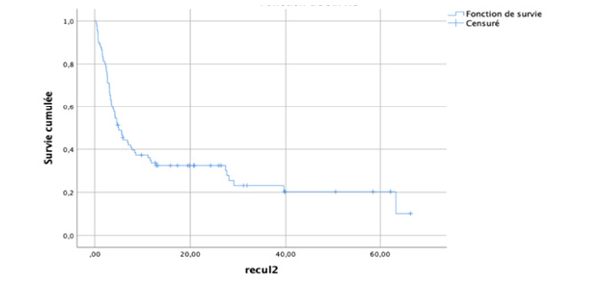
The median overall survival was 13 months (Figure 2), while the progression-free survival was 7,2 months.
Discussion
Kidney cancer is the third most common cancer of the urogenital system, following prostate and bladder cancer. It represents 3% of solid adult cancers. An increase in the number of kidney cancer cases has been recorded in the past 25 years, particularly in high-incidence countries such as Europe and North America. However, this growth has slowed since the year 2000, especially in certain European countries (Sweden, Finland, Poland, and the Netherlands). The lowest incidence rates are observed in Africa, Asia, and the Pacific Islands (less than 1.5/100,000 inhabitants).
This recent increase in incidence appears to be associated with earlier stages, likely due to a high frequency of incidentally discovered kidney cancer following widespread use of medical imaging.
In our series, the average age of patients was 60 years, with extremes ranging from 40 to 65 years. The most affected age groups were those between 60 and 69 years old (37%). The average age of our patients indicates that kidney cancer is a condition of the elderly, with a typical presentation in the sixth and seventh decades of life [6].
The clinical profile of our series was comparable to that of JANANE [7], regarding 47 cases of kidney cancer in 2003. The array of clinical signs varies, with the most dominant reason for consultation being unilateral lumbago (81%), followed by hematuria (25%) and a lumbar mass (10%).
CT scan is the reference examination for assessing regional extension, with sensitivity evaluated between 60 and 92% and specificity between 91 and 100%. Local extension is similarly assessed by CT scan and MRI [8,9], which allows for the detection of neoplastic infiltration of the renal lodge, adrenal gland, and renal sinus fat. The condition of the renal sinus fat and renal lodge can be readily analyzed.
The histological report established by the pathologist, regardless of the surgical specimen, should include data necessary for the optimal therapeutic management of the patient, based on the recommendations of the National Cancer Institute (INCa). These histopathological data will allow for the determination of the histological subtype, Hist prognostic criteria, and the pTNM 2009 stage. In the case of total nephrectomy, the histological subtype of the renal tumor according to the WHO 2004 classification, tumor size, Fuhrman nuclear grade, estimated percentage of sarcomatoid component, tumor necrosis, vascular emboli, locoregional invasion involving hilar fat, perirenal fat, and/or beyond the Gerota's fascia, presence of tumor emboli in the renal vein or its branches, invaded lymph nodes, invasion of the adrenal gland, associated lesions, and pTNM 2009 [10] classification will be assessed.
In our series, renal biopsy was performed in 76 patients as they were metastatic from the outset. Twelve cases underwent prior nephrectomy to provide histological evidence of their kidney cancer, 3 underwent extended nephrectomy for hemostatic emergency, and cytoreductive nephrectomy was instituted in 5% of patients. In our series, all clinical, radiological, and anatomopathological diagnostic elements were consistent with literature data. In the absence of randomized studies on the role of nephrectomy in the era of immunotherapies, first-line systemic treatment remains recommended for intermediate and poor-risk groups. The role of deferred nephrectomy needs to be determined in patients who respond well.
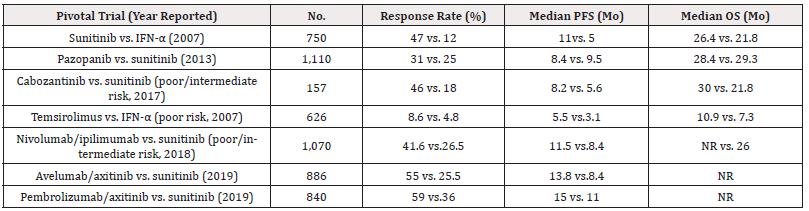
Treatment with first-generation TKIs like sunitinib, sorafenib, and pazopanib in patients with mRCC leads to the development of primary and acquired resistance to these drugs. Therefore, these therapeutic agents may be replaced by more effective TKIs such as cabozantinib, axitinib, lenvatinib, and tivozanib. Treatment with cabozantinib has demonstrated an increase in progression-free survival (PFS) among mRCC patients compared to sunitinib (Table 2) [11]. Axitinib, a multi-receptor anti-angiogenic inhibitor, has shown higher objective response rates and improved median PFS compared to sorafenib in clinical trials.
The combination of axitinib, cabozantinib, and lenvatinib with various PD-1 immune checkpoint inhibitors as first-line therapy has shown superior efficacy in patients with advanced RCC compared to monotherapy approaches (Table 2) [12,13]. Therefore, the latest guidelines recommend the use of these TKIs in combination with immunotherapeutic agents as first-line treatment.
Conclusion
The overall survival outcomes among patients with nccRCC who underwent cytoreductive nephrectomy or received TKI therapy were modest throughout the study period. However, the reform of the national health system and the generalization of medical coverage have allowed greater accessibility to new therapies.
References
- Jemal A, Ward E, Hao Y, Xu J, et al. (2008) Cancer statistics. CA Cancer J Clin 58(2): 71-96.
- Parkin DM, Whelan SL, Ferlay J, Teppo L, Thomas D (2002) Cancer Incidence in five continents vol VIII. IARC Scientific publications No 155. France: International Agency for Research on Cancer.
- (2020) Estimated Cancer Incidence, Mortality and Prevalence Morocco in 2020.
- Kernion JB, Belldegrun A (1992) Renal tumors. In: Campbell’s Urology. Edited by PC Walsh, AB Retick, TA Stamey, and ED Vaughan. Philadelphia: WB. Saunders Company 27: 1053-1093.
- Hsieh JJ, Purdue MP, Signoretti S, et al. (2017) Renal cell carcinoma. Nat Rev Dis Primers 3: 17009.
- Ziya Kirkalia, Can Obek (2003) Clinical Aspects of Renal Cell Carcinoma Eau update series 1(4): 1189-196.
- A Janane, H Hachi, F Tijami, A Jalil, M Othmani, et al. (2003) Cancer du rein: à propos de 47 cas Carcinoma of the kidney: about 47 cases. Annales d’urologie 37(2): 57-60.
- Schwartz LH, Panicek DM, Koutcher JA, Brown KT, Getrajdman GI, et al. (1995) Adrenal masses in patients with malignancy: prospective comparison of echo-planar, fast spin-echo,and chemical shift MR imaging. Radiology 197(2): 421 -425.
- Crow J, Slavin G, Kreel L (1981) Pulmonary metastases: a pathologic and radiologic study. Cancer 47(11): 2595-2602.
- Lonser RR, Glenn GM, Waither M, Chew EY, Libutti SK, et al. (2003) Von Hippel-Lindau disease. Lancet 361(9374): 2059-67.
- Choueiri TK, Hessel C, Halabi S, Sanford B, Michaelson MD, et al. (2018) Cabozantinib versus sunitinib comme traitement initial du carcinome rénal métastatique à risque intermédiaire ou faible (essai randomisé Alliance A031203 CABOSUN): survie sans progression par examen indépendant et mise à jour de la survie globale. EUR J Cancer 94: 115-125.
- Bedke J, Albiges L, Capitanio U, Giles RH, Hora M, et al. (2021) The 2021 updated European Association of Urology Guidelines on Renal Cell Carcinoma: Combination therapies based on immune checkpoint inhibitors for treatment-naïve metastatic clear cell renal cell carcinoma are the standard of care. Eur Urol 80(4): 393-397.
- Albiges L, Flippot R, Escudier B (2021) Inhibiteurs de points de contrôle immunitaires dans le carcinome rénal métastatique à cellules claires: l’expression de PD-L1 est-elle utile? Eur Urol 79: 793-795.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.