Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Acute Cerebral Ischemia in Patient with COVID 19: Debut of the Thrombectomy Service in Kuwait - Case Report
*Corresponding author: Lazar Lazovic, Interventional Neuroradiologist, Medical Imaging Department Ibn Sina Hospital, PO box 25427 Safat 13115, Kuwait.
Received: April 29, 2024; Published: May 02, 2024
DOI: 10.34297/AJBSR.2024.22.002957
Abstract
Background: We present atypical case of acute ischemic stroke in a young patient with COVID 19, requiring mechanical thrombectomy and intracranial stenting of underlying Intracranial Atherosclerotic Disease (ICAD).
Case Presentation: A 36-year-old Kuwaiti male, that was receiving therapy for COVID 19 bilateral pneumonia, developed left side weakness and neglect due to right MCA occlusion, National Institutes of Health Stroke Scale score was 18. Right cerebral ischemic lesion and occlusion of right MCA were confirmed by CT and CTA. The patient was shifted to thrombectomy capable center and thrombectomy was performed. The underlying stenosis of MCA was stented resulting in TICI 3 recanalization. Functional outcome at 90 days measured with modified Ranking scale was 0.
Conclusion: Even though the evidence for stenting in these cohort is lacking in the literature, given the high rate of mortality of COVID-19 patients with acute cerebral ischemia, we advocate for stenting as it may provide beneficial outcomes, as occurred in our case. We believe that clinicians performing mechanical thrombectomies should consider more aggressive endovascular treatment for selected patients in the setting of COVID 19.
Keywords: Cerebral ischemia, COVID 19, Intracranial arteriosclerosis, Stenting, Thrombectomy
Abbreviations and Acronyms: MCA: Middle Cerebral Artery; ICA: Internal Carotid Artery; LVO: Large Vessel Occlusion; ICAD: Intracranial atherosclerotic disease; TICI: Thrombolysis in Cerebral Infarction; mRS: modified Ranking scale; NIHSS: National Institutes of Health Stroke Scale; ASPECTS: Alberta stroke program early CT score; PCR: Polymerase Chain Reaction; DSA: Digital Subtraction Angiography; COVID 19: Coronavirus disease 2019; NECT: Non-enhanced Computed Tomography; CTA: Computed Tomography Angiography; SARS-CoV 19: Severe Acute Respiratory Syndrome Coronavirus 19
Introduction
Mechanical thrombectomy is well established treatment option for patients with acute ischemic stroke due to Large Vessel Occlusion (LVO). [1,2]. There is a growing body of published evidence that the Coronavirus Disease 2019 (COVID 19), by producing procoagulable state, may be associated with acute ischemic stroke secondary to LVO [3,4]. Despite many challenges to the commencement of this service in Kuwait, a pilot project in a ‘drip and ship model’ has been launched. We report the first case of young patient in whom COVID-19 disease in our opinion led to progression of Intracranial Atherosclerotic Disease (ICAD) leading to complete right Middle Cerebral Artery (MCA occlusion and acute cerebral ischemia.
Case Summary
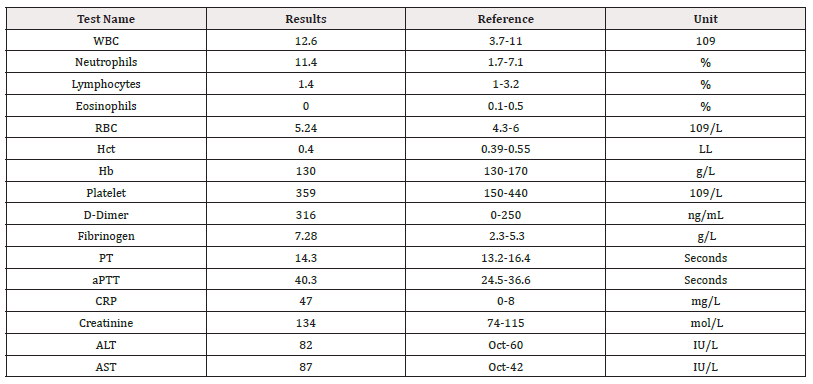
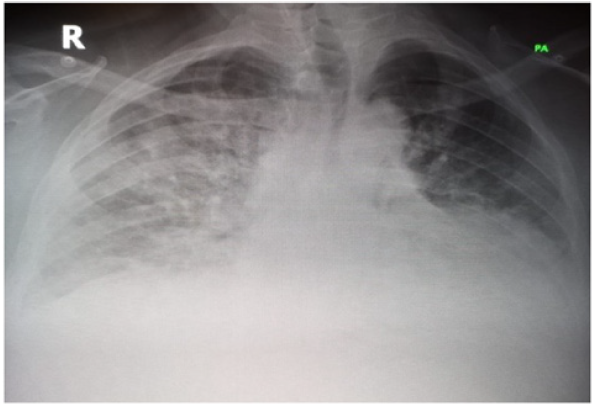
A 36-year-old Kuwaiti male with clinical history of diabetes mellitus type 2, hypertension and obesity was admitted due to bilateral lung disease caused by Severe Acute Respiratory Syndrome Coronavirus 19 (SARS CoV 19) infection. Infection was confirmed by Polymerase Chain Reaction (PCR) test, laboratory tests (Table 1) and chest x-ray (Figure 1).
He was treated symptomatically in the medical ward with oxygen via nasal prongs. Ten days after his swab he developed acute left side weakness and neglect. The National Institutes of Health Stroke Scale (NIHSS) was 18. Brain Non-Enhanced Computed Tomography (NECT) and Computed Tomography Angiography (CTA) were performed, and signs of acute brain ischemia of right cerebral hemisphere were identified (ASPECT score 7) with acute occlusion of M1 segment of right MCA (Figures 2,3).
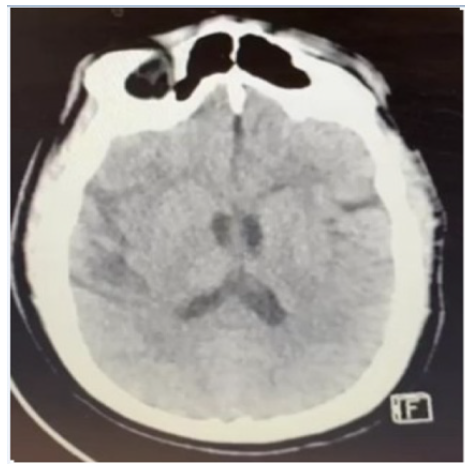
Figure 3: Non contrast brain CT: Insular “ribbon sign” and blooming of basal ganglia at the right side-early signs of cerebral ischemia.
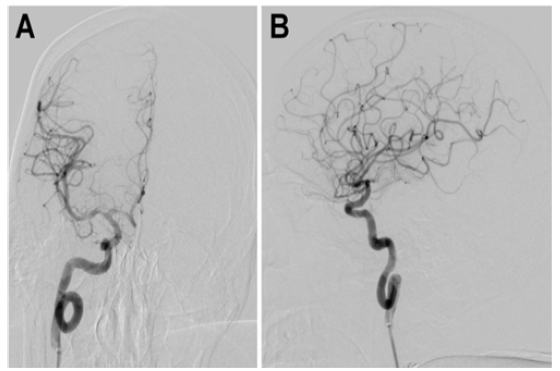
Due to anticoagulation therapy, he did not receive tPA. The transfer to a thrombectomy-capable center was arranged with the neurointerventional team. After general anesthesia initiation in negative pressure room, digital subtraction angiography DSA was performed and occlusion of M1 segment of right MCA was confirmed (Figure 4a and 4b).
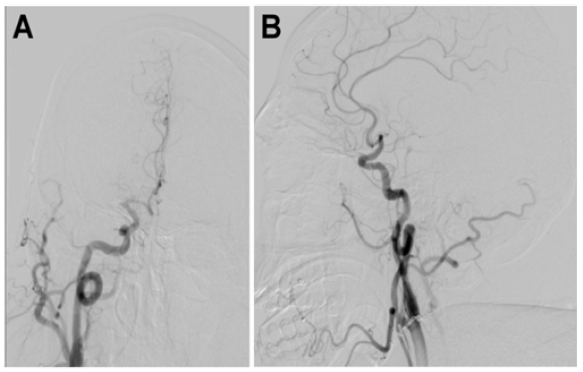
Figure 4: Digital subtraction angiography (DSA): (A) Towns projection-occlusion of M1 segment of right MCA, (B) Lateral projection- occlusion of M1 segment of right MCA.
FlowGate2 balloon guide 8F (Stryker Neurovascular, Fremont, CA, USA) was introduced within right Internal Carotid Artery (ICA) and CAT 6 Distal Access Catheter (Stryker Neurovascular, Fremont, CA, USA) was placed up to supraclinoid segment of ICA. Occlusion was passed with microcatheter and microguide wire. First pass recanalization made with stent retriever EMBOTRAP™ 2 (CERENOVUS, Johnson & Johnson Medical Co, US) size 5x33mm under double aspiration. Follow up angiography revealed Thrombolysis in Cerebral Infarction (TICI) grade 3 recanalization with remaining stenosis of proximal M1 segment of MCA (Figure 5a).
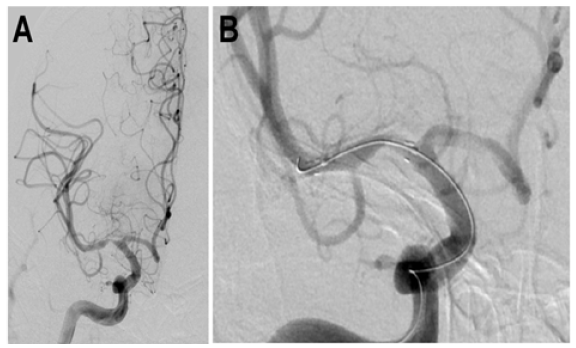
Figure 5: Digital subtraction angiography (DSA): (A) Anteroposterior projection- First pass recanalization with proximal stenosis, (B) Anteroposterior projection-Angioplasty of stented stenotic segment of right MCA.
Patient was loaded with Aspirin 500mg over naso-gastric tube and 0,4mcg/kg of Tirofiban as IV bolus. Bolus of Tirofiban was followed with infusion of 0,1mcg/kg/min for next 24 hours. Stenting of MCA was done using Neuroform Atlas stent (Stryker Neurovascular, Fremont, CA, USA) 3x15mm followed by angioplasty of the stent using Gateway PTA Balloon Catheter (Stryker Neurovascular, Fremont, CA, USA) 2,5x15mm (Figure 5b).
Symptoms-onset to admission to Ibn Sina hospital was 180 minutes. Door to reperfusion time was 60 minutes and groin to reperfusion time was 18 minutes. Final angiogram, done 30 minutes after stent placement, showed appropriate stent opening and complete reperfusion of MCA (Figure 6a and 6b).
24 hours later follow-up NECT and CTA revealed no hemorrhage or ischemic changes with preserved flow throughout the stent (Figure 7a and 7b).
Infusion of Tirofiban was discontinued and patient was loaded with 300mg of Clopidogrel. He continued with Aspirin 81mg and Clopidogrel 75mg once daily for three months. NIHSS score dropped to 2. Functional outcome at 90 days measured with mRS was 0.
Discussion
The usual presenting symptoms and signs of COVID-19 disease include fever, cough, and shortness of breath. However, reported series from Wuhan, China showed 36% of patients had neurological manifestations. Acute cerebrovascular disease was reported in 6% of severely affected patients [5]. Despite high reperfusion rates achieved by usage of different thrombectomy equipment and techniques, reported mortality rates in patients with COVID 19 disease remained high, ranging from 29% to 35% [6,7]. Moreover, ICAD accounts nearly to 50% of acute ischemic strokes in Asian population making endovascular treatment even more challenging [8-10]. Besides genetic predispositions, our patient had other acquired ICAD risk factors such as hypertension, diabetes, and hyperlipidemia. By now different pathological mechanisms of cerebral ischemia in COVID-19 disease are proposed and some of them can accelerate the atherosclerotic disease to complete vessel occlusion. The described mechanism includes hypercoagulable state, hyperserotonemia, cardiac damage followed by distal embolization and antiphospholipid syndrome [11]. Our patient had acute COVID-19 lung infection which itself may be the reason of D-dimer elevation to 316ng/ml, however, it may be associated with thromboembolic complication as well.
Angiotensin Converting Enzyme 2 (ACA 2) receptors are found in alveolar epithelium of the lungs, as well as in the vascular endothelium [12]. Consequently, patients with severe COVID 19 may be at danger of thrombosis and cerebral ischemia, due to both hypercoagulable state and direct vascular endothelial injury that may lead to plaque rupture. Furthermore, autopsy studies done in stroke patients found high prevalence of non-stenotic atherosclerotic plaques, 6% of which had superimposed thrombi therefore were considered casual in ischemic event [13]. Ischemic stroke in our patient is caused by MCA occlusion. TICI 3 recanalization was achieved after the first pass using stent retriever. Follow up DSA revealed remaining narrowing of proximal M1 segment of MCA, presumably atherosclerotic in nature. Recently published results of trial of intracranial stenting showed reasonably low risk of periprocedural complications and death with intracranial stenting [14].
Even though intracranial stenting is still nor acclaimed as an initial treatment of intracranial atherosclerotic disease [15], the decision to stent MCA in acute setting was made on the grounds that activation of immune and inflammatory factors together with hypercoagulable state may be the reason of plaque disruption, serving as a source of thrombosis. In our opinion, leaving unstable plaque unsecured in COVID 19 positive patient carries more risks of re-occlusion and unfavorable outcome [16] and outweighs the risks of intracranial stenting. Considering that platelet count more than 220g/L is one of the identified factors for early re-occlusions [16] and our patient’s platelet count reached 359g/L we opted for an aggressive anti-aggregation therapy. In support of our hypothesis that underlying atherosclerotic plaque rupture is in the etiology of MCA thrombosis and not material induced spasm, goes the fact that we noticed an insufficient stent expansion at the site of narrowing. An additional balloon angioplasty of the stent was necessary for full expansion. Our patient showed immediate neurological improvement measured by NIHSS score drop from 18 to 8. He recovered from lung infection and brain stroke, and functional outcome at 90 days, mRS was 0.
Conclusion
It is well known now that besides the respiratory system, COVID 19 significantly affects cardiovascular system and can lead to acute cerebral ischemia. Even though the evidence for stenting in these cohort is lacking in the literature, given the high rate of mortality of COVID-19 patients with acute cerebral ischemia, we advocate for stenting as it may provide beneficial outcomes, as occurred in our case. In addition, we believe that some key points, such as defining a binding algorithm, pointing out the factor time in acute stroke care and the importance of multidisciplinary stroke team are crucial at the beginning of the acute stroke care journey. We believe that clinicians performing mechanical thrombectomies should consider more aggressive endovascular treatment for selected patients in the setting of COVID 19We take great pride in establishing the first such center in Kuwait with ongoing dedication to its further development.
Declaration
Consent to Participate
All authors read and approved the final manuscript.
Ethics approval
Non applicable
Consent for Publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Availability of Data and Materials
Non applicable
Conflict of Interest
None
Funding
Non applicable
Authors' Contributions
The first draft of the manuscript was written by Lazar Lazovic and all authors commented on previous versions of the manuscript.
Acknowledgements
Lazar Lazovic Medical Imaging Department, Ibn Sina Hospital, Ministry of Health, Kuwait City, Kuwait
Lamya Alsarraf Medical Imaging Department, Ibn Sina Hospital, Ministry of Health, Kuwait City, Kuwait
Athari Salmeen Neurology Department, Jaber Al-Ahmad Al-Sabah Hospital, Ministry of Health, Kuwait City, Kuwait
Khalifah Alshayeji Neurology Department, Jaber Al-Ahmad Al-Sabah Hospital, Ministry of Health, Kuwait City, Kuwait
Mahdi BenMoosa Neurology Department, Jaber Al-Ahmad Al-Sabah Hospital, Ministry of Health, Kuwait City, Kuwait
Ghada Adel Hamden Anesthesia and Intensive Care Department, Ibn Sina Hospital, Ministry of Health, Kuwait City, Kuwait
Petar Bosnjakovic Medical Imaging Department, Ibn Sina Hospital, Ministry of Health, Kuwait City, Kuwait
References
- Berkhemer OA, Puck Fransen SS, Debbie Beumer, Lucie van den Berg A, Hester Lingsma F, et al. (2015) A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 372(1): 11-20.
- Cagnazzo F, Michel Piotin, Simon Escalard, Benjamin Maier, Marc Ribo, et al. (2021) European multicenter study of ET-COVID-19. Stroke 52(1): 31-39.
- Mayank Goyal, Bijoy Menon K, Wim van Zwam H, Diederik Dippel WJ, Peter Mitchell J, et al. (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 387(10029): 1723-1731.
- Hernández Fernández F, Hernán Sandoval Valencia, Rosa Angélica Barbella Aponte, Rosa Collado Jiménez, Óscar Ayo Martín, et al. (2020) Cerebrovascular disease in patients with COVID-19: neuroimaging, histological and clinical description. Brain 143(10): 3089-3103.
- Hoffmann M, Hannah Kleine Weber, Simon Schroeder, Nadine Krüger, Tanja Herrler, et al. (2020) SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 181(2): 271-280.e8.
- Mao L, Huijuan Jin, Mengdie Wang, Yu Hu, Shengcai Chen, et al. (2020) Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol 77(6): 683-690.
- Mazighi M, Julien Labreuche, Fernando Gongora Rivera, Charles Duyckaerts, Jean Jacques Hauw, et al. (2008) Autopsy prevalence of intracranial atherosclerosis in patients with fatal stroke. Stroke 39(4): 1142-1147.
- Kleindorfer DO, Amytis Towfighi, Seemant Chaturvedi, Kevin M Cockroft, Jose Gutierrez, et al. (2021) 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American heart association/American stroke association. Stroke 52(7): e364-e467.
- Mosimann PJ, Johannes Kaesmacher, Dominic Gautschi, Sebastian Bellwald, Leonidas Panos, et al. (2018) Predictors of unexpected early reocclusion after successful mechanical thrombectomy in acute ischemic stroke patients. Stroke 49(11): 2643-2651.
- Michael J Alexander, Alois Zauner, John C Chaloupka, Blaise Baxter, Richard C Callison, et al. (2019) WEAVE Trial: Final Results in 152 On-Label Patients. Stroke 50(4): 889-894.
- Styczen H, Volker Maus, Lukas Goertz, Martin Köhrmann, Christoph Kleinschnitz, et al. (2022) Mechanical thrombectomy for acute ischemic stroke in COVID-19 patients: multicenter experience in 111 cases. J NeuroInterventional Surg 14(9): 858-862.
- Thachil J, Ning Tang, Satoshi Gando, Anna Falanga, Marco Cattaneo, et al. (2020) ISTH interim guidance on recognition and management of coagulopathy in COVID‐19. J Thromb Haemost 18(5): 1023-1026.
- Stamm B, Deborah Huang, Regina Royan, Jessica Lee, Joshua Marquez, et al. (2022) Pathomechanisms and treatment implications for stroke in COVID-19: a review of the literature. Life 12(2): 207.
- Wagner DD, Lukas A Heger (2022) Thromboinflammation: from atherosclerosis to COVID-19. Arterioscler Thromb Vasc Biol 42(9): 1103-1112.
- Wong LKS (2006) Global burden of intracranial atherosclerosis. Int J Stroke 1(13): 158-159.
- Yaghi S, Shyam Prabhakaran, Pooja Khatri, David S Liebeskind (2019) Intracranial atherosclerotic disease: mechanisms and therapeutic implications. Stroke 50(5): 1286-1293.





 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.