Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Adjunctive Care in Sequential Diabetic Foot Wounds: Case Study
*Corresponding author: Jonathan R T Lakey, Departments of Surgery and Biomedical Engineering, University of California Irvine, Irvine CA 92617, USA.
Received: April 2, 2024; Published: April 10, 2024
DOI: 10.34297/AJBSR.2024.22.002916
Abstract
Background: Diabetic foot wounds are an enormous health care burden worldwide. Diabetic foot wound care requires close follow up to monitor for impediments to wound healing. The main factors that lead to stalled wound healing include infection, peripheral vascular disease, and uncontrolled diabetes. Adjunctive therapies are often added to address impediments to healing and have positively impacted the way we manage diabetic wounds. Adjunctive therapies are tailored to the needs of each patient’s wounds and improve wound healing rates and outcomes.
Case Report: We present a patient who had two sequential left diabetic foot wounds. Although wound healing was stalled, both wounds healed by 16 weeks with aggressive use of adjunctive wound care techniques. We discuss adjunctive wound care therapies including, Negative Pressure Wound Therapy (NPWT), Hyperbaric Oxygen Therapy (HBOT), skin substitutes, and Physiologic Insulin Resensitization (PIR). PIR is a novel modality with much promise as a wound care adjunctive therapy. We compare the two wounds and discuss the different adjunctive therapies used for each wound.
Conclusion: We conclude that adjunctive therapies give an optimal opportunity for wound healing as they address common factors that may delay healing, specifically in complex diabetic wound care. PIR, one of the therapies we discuss, serves as a modality that not only expedites wound healing but also helps improve HgbA1c and gain better control on factors that may impede wound healing.
Keywords: Diabetic foot ulcer, Physiologic insulin resensitization, adjunctive therapy, negative pressure wound therapy, skin substitute, and hyperbaric oxygen therapy
Introduction
Diabetes mellitus is one of the fastest growing and most financially burdensome illnesses worldwide. According to the Centers for Disease Control and Prevention (CDC), “around 14.7% of the adult U.S. population (37.1 million) have diabetes, and another 38% (96 million) of U.S. adults have prediabetes [1]”. Additionally, diabetes can lead to various complications, including diabetic peripheral neuropathy, diabetic foot wounds, cardiovascular disease, and diabetic kidney disease [2,3].
15 Fifteen percent of diabetic patients will have a diabetic foot wound, commonly located on the plantar surface of the foot. In addition, 6 percent will be hospitalized due to infection or other wound complications. In the United States, diabetes is the leading cause of non-traumatic lower-extremity amputations with 14-24 percent of diabetics with a foot ulcer requiring an amputation. It has been shown that 85 percent of diabetes-related amputations were preceded by a foot ulcer [4].
A diabetic foot wound occurs in 15 percent of diabetic patients and is commonly located on the plantar surface of the foot. Of those who develop a diabetic foot wound, 6 percent will be hospitalized due to either infection or other ulcer-related complications. Diabetes is the leading cause of non-traumatic lower extremity amputations in the United States, and approximately 14-24 percent of patients with diabetes who develop a foot ulcer will require an amputation. Foot ulceration precedes 85 percent of diabetes-related amputations [4].
Wound care may generally be divided into standard and adjunctive techniques. Standard care of a diabetic foot wound includes cleansing the wound, offloading, dressing changes and debridement as indicated. It also includes attention to glycemic control and evaluation for Peripheral Arterial Disease (PAD) and infection. Standard measures are what everyone gets. Adjunctive therapies are used selectively. These include skin substitutes, HBOT, NPWT, pulse lavage and the like. We introduce Physiologic Insulin Resensitization (PIR) as a new adjunct to wound care. PIR is a complementary therapy to traditional treatments for diabetes. With PIR, short-acting insulin is given episodically every 4-8 minutes mimicking the body’s normal insulin release. An intravenous pump is used. There is concurrent administration of glucose. Doses of insulin are carefully adjusted to maintain a target steady blood sugar level. The treatment lasts for 2-3 hours and is done 1-3 times weekly [5]. Evidence has shown that PIR utilized as a treatment modality, can reverse There is consistent evidence that this treatment modality can reverse the diabetes-associated complications of neuropathy, diabetic ulcers, nephropathy, and retinopathy, and that lowers HbA1c [6].
In a classic study from 2003, Sheehan et al. identified that the healing rate at 4 weeks predicts healing at 12 weeks in diabetic foot wounds. Specifically, Sheehan et al found that for those that achieved 53% or more reduction in wound area by 4 weeks, 58% of these patients healed by 12 weeks. Whereas, for those that did not achieve 53% or greater wound area reduction at 4 weeks, only 9% healed at 12 weeks.
In this article, we report two sequential diabetic foot wounds in one patient. We describe his progress in wound size reduction and correlate that to adjunctive therapy usage.
Case Report
GD is a 57-year-old male with a history of uncontrolled type 2 diabetes mellitus, hypertension, hyperlipidemia, diabetic peripheral neuropathy, gastroparesis, and PAD. He underwent a prior right below knee amputation relating to a diabetic foot wound and PAD several years earlier. He presented on February 11, 2022, for evaluation of new wounds on his left 2nd and 3rd toes. An extensive work up was initiated including an arterial duplex ultrasound, x-ray imaging, and an MRI to assess for osteomyelitis. Lab work revealed his HgbA1c was 12.5. X-rays were negative for fracture, dislocation, and foreign body. MRI findings indicated probable osteomyelitis in the 2nd and 3rd metatarsal heads. His arterial duplex 2/14/22 showed triphasic signals throughout with intact tibial vessels. He was then admitted to the hospital for antibiotic treatment and wound care. At 1 week following presentation (2/18/22), the patient underwent trans-metatarsal amputation of his left 2nd and 3rd toes and the wound was left open. Following the surgery, index measurements showed 7.5 x 5.2 x 3.5, this will be considered day 0 of wound care. A wound vac was placed post-operative day 2. He was discharged on day 4, with home health and outpatient care.
He was seen weekly in the clinic for wound vac changes and assessment of his wound. The wound vac was discontinued after 5 weeks. At these times his wounds were assessed with utilization of a MolecuLight bacterial autofluorescence exam (MolecuLight, Inc, ON, Canada). Red fluorescence, indicating critical colonization, was noted after 6 weeks of wound care on 4/4/22. Betadine soaks were added to his wound care regimen at this time. He underwent twenty sessions of hyperbaric oxygen treatments from week 2 through week 6 (2/28/22-3/28/22). He had Theraskin skin substitute placed once weekly starting from week 9 through week 12. Collagen powder was added to dressing changes beginning at 12 weeks on 5/17/22.
In summary, the course of wound care for this patient’s first wound began on 2/18/2022 and lasted until 6/3/2022 for a total of 15 weeks. The adjunctive therapies utilized for this wound included NPWT, HBOT, Theraskin skin substitutes, and collagen powder. Eliminating and managing infection was an important component for this wound to ensure optimal environment for wound healing.
After four weeks of wound care, wound surface area was reduced by 36.5%. At twelve weeks, wound surface area was reduced by 84%. Even though wound surface area was not reduced by 53% by the fourth week, his wound was deemed closed on June 3, 2022, after 15 weeks of aggressive wound care. As exemplified by this case, adjunctive therapies have made healing possible for this complex diabetic foot wound (Figure 1,2).
On November 29, 2022, he re-presented with a new first metatarsal head plantar wound. A repeat arterial duplex now showed evidence of a hemodynamically significant lesion in his left anterior tibial artery. Given the location of the wound, this vessel was felt to be angiosome-specific. On 12/8/22 he underwent left anterior tibial atherectomy and balloon angioplasty via access from the right common femoral artery. At this time, he also underwent debridement and inpatient hospitalization. The wound deteriorated. His HgbA1c was noted to be 12.3. He was taken to surgery 12/13/22. A plantar space abscess was encountered. The first toe was not felt salvageable and was amputated mid metatarsal. Index wound measurements taken at the time of surgery were 11.3 x 7.7 x 3.8. The wound vac was instituted post op day 3. He was discharged home on 12/18/22, Day 5 post index wound measurements, with home health and the wound vac changes three times weekly.
He was seen weekly in the clinic. No positive MolecuLight exams were noted through the course of his wound care. The wound vac was discontinued after 6 weeks on 1/23/23. He had Zenith amnionic skin substitutes placed weekly from weeks 7- week 14. Purocal collagen was added to dressing changes beginning 12 weeks since initial wound measurements on 3/3/22. He had twenty-five PIR treatments from week 6 through week 16, (1/16/23-4/6/23). His HgbA1c during week 4 (1/7/2023) was 8.1 and on 4/22/23 it was 8.6 which shows improvement since his previous HgBA1c of 12.3.
In summary, the course of wound care for this patient’s second wound began on 12/13/2022 and lasted until 4/6/2023 for a total of 16 weeks. The adjunctive therapies utilized for this wound included NPWT, Zenith amniotic skin substitutes, purocal collagen powder, and PIR. Managing and controlling his chronic conditions of peripheral vascular disease and uncontrolled Type 2 Diabetes Mellitus were important to allow for healing of this patient’s second wound because if not managed, may lead to stalled wound healing. His peripheral vascular disease was managed by treating the hemodynamically significant lesion with atherectomy and balloon angioplasty. The patient’s Type 2 DM was better controlled by utilizing PIR treatments in conjunction with his current diabetic treatment regimen.

Figure 1: A. Wound at week 1, size 7.5 x 4.1 x 3.0 B. Wound at week 4, size 5.5 x 4.5 x 3.0 C. Wound at week 12, size 4.2 x 1.5 x 0.1.
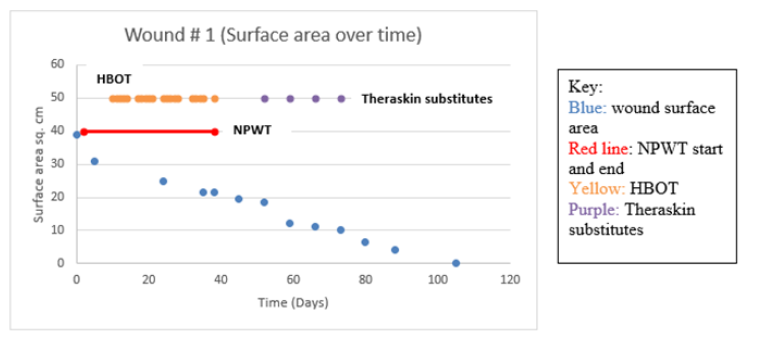
Figure 2: Depicts the progress in wound surface area reduction in square cm over time shown in blue; the adjunctive therapies utilized included; Hyperbaric Oxygen Therapy (HBOT) shown in yellow and Theraskin substitutes shown in purple. The red line depicts the duration of Negative Pressure Wound Therapy (NPWT).
After four weeks of wound care, wound surface area was reduced by 41%. At twelve weeks, wound surface area was reduced by 89%. Even though wound surface area was not reduced by 53% by the fourth week, his wound was deemed closed on April 6, 2023, after 16 weeks of aggressive wound care. As exemplified by this case, adjunctive therapies have made healing possible for this complex diabetic foot wound (Figure 3,4).
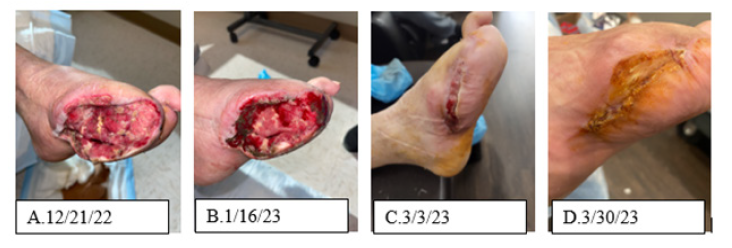
Figure 3: A. Wound at week 1, size 10.5 x 5.8 x 3.0 B. Wound at week 4, size 9.8 x 4.2 x 0.3 C. Wound at week 12, size 6.7 x 1.4 x 0.1 D. Wound at week 16, size 1.1 x 0.3 x 0.1

Figure 4: Depicts the progress in wound surface area reduction in square cm over time shown in blue; the adjunctive therapies utilized included; Zenith Allograft skin substitutes shown in purple, Physiologic Insulin Resensitization (PIR) treatments shown in pink. The red line depicts the duration of Negative Pressure Wound Therapy (NPWT).
Discussion
Diabetic foot wound care is an involved process. It includes evaluating the barriers to healing and addressing them. The barriers commonly include peripheral arterial disease, poor glycemic control, and infection. Standard wound care in a diabetic foot wound management includes surgical debridement, dressings to facilitate an optimal moist wound environment and exudate control, wound off-loading, vascular assessment, infection management, and glycemic control [7]. Our patient in this report received all the elements of standard care.
Critical bacterial colonization, though not frank infection, may stall wound healing. MolecuLight is a handheld device that enables rapid determination of the presence of critical colonization [8]. Our patient in this report underwent frequent MolecuLight evaluations. Management was adjusted when a positive study returned.
Along with standard care, adjunctive therapies are used selectively. For diabetic foot wounds, adjunctive therapies are utilized to intervene with wound healing when there is a failure to show more than 50% wound area reduction in 4 weeks, indicates the need for adjunctive wound therapy [9]. There are multiple adjunctive therapies available, such as NPWT, HBOT, bioengineered cellular therapies, and extracellular matrix products such as collagen.
NPWT improves wound healing by multiple factors, such as minimizing reducing edema, removing bacterial products contaminants, and helping to approximate wound edges [10]. These properties alone allow for an optimal wound environment and can help expedite wound healing. NPWT is especially helpful in deep wounds due to its ability to approximate wound edges at a quicker rate than a wound without NPWT. Another adjunctive therapy worth discussion is Studies regarding Hyperbaric Oxygen Therapy (HBOT) which studies have shown on angiogenesis demonstrates an increased rate of blood vessel formation [11]. In addition, It has also been shown that the prolonged use of hyperbaric oxygen therapy has also been shown to decrease the recruitment and adhesion of neutrophils, increases oxygen dispersion to damaged tissues, reduces inflammation, and accelerates healing in patients with diabetic ulcers [12]. HBOT also proves to have antimicrobial activity which can allow an optimal environment for wound healing. HBOT accomplishes its antimicrobial activity by its The mechanisms related to the antimicrobial activity of HBOT include direct bactericidal effects through the formation of Reactive Oxygen Species (ROS), the immunomodulatory effect of HBOT that increase the antimicrobial effects of the immune system, and the synergistic effects of HBOT with antibiotics [13]. In our presented case, GD had NPWT early in the treatment of both wounds. He had HBOT early in the course of the first wound.
Normal healthy skin provides serves as a protective barrier against microbes [14] and water loss. Wounds are disruptions of the skin’s structural and functional integrity [14]. Wound healing is the restoration of this structural and functional integrity. Healing is understood to proceed through phases: hemostatic, inflammatory, proliferative, and remodeling. The phases overlap but are understood to feature particular cells and particular cytokines as the phases progress [15]. When healing stalls, often the wound is described as “stuck in the inflammatory phase.”
“Skin substitutes” are a broad collection of various combinations of cellular and acellular components that are . They are both human and animal-derived [15]. While they do not actually substitute for skin, they do provide a source of growth factors, cytokines, and enzymes that promote healing or liberate the wound from the inflammatory phase [16]. S That is, skin substitutes help improve wound healing by providing the necessary cells and factors required for tissue growth and regeneration, not by replacing skin.
In our presented case, GD had TheraSkin® used to treat his first wound and Zenith amniotic membrane for his second wound. TheraSkin® is a cadaveric-derived allograft. Tissue is harvested within 24 hours postmortem from an organ donor who cleared standard safety screenings for organ procurement [17]. It is biologically active and cryopreserved with both epidermis and dermis. Its cellular and extracellular composition provides growth factors, cytokines, and collagen that. It promotes healing but does not replace skin. Zenith amniotic membrane is a human amniotic based allograft. Its extracellular matrix is rich in collagens, glycosaminoglycans, proteoglycans, and cytokines. Studies show that it stimulates re-epithelialization, promotes angiogenesis, and aids in reducing inflammation and scarring [18].
Collagen is, a key component of the extracellular matrix that, plays a critical roles in the regulation of the phases of wound healing and has been utilized as an adjunct wound therapy to promote healing [19]. Chronic wounds that are “stuck in the inflammatory phase” likely have increased destruction of extracellular matrix components. This destruction involves an elevated amount of metalloproteinases and an improper activation of soluble mediators of the wound healing process. Collagen may promote healing by dampening these destructive processes acting on extracellular matrix [20]. In our presented case, GD had collagen used in treating both wounds.
Physiologic Insulin Resensitization (PIR) is a complementary therapy to traditional diabetes management. It involves infusing a patient with regular insulin in episodic bursts every 4-8 minutes for 2-4 hours per treatment for 1-3 treatments per week. The insulin concentration and dose amount are carefully chosen based on calculated insulin resistance and are adjusted throughout the infusion. Glucose is concurrently given during the infusion and blood sugar is maintained at a pre-determined level. An FDA-approved pump is used to deliver the insulin. PIR is a patented modality that could have significant benefit in diabetic wound healing.
There is evidence that PIR can has been shown to reverse the diabetes-associated complications of neuropathy, nephropathy, and retinopathy. PIR has also been shown to, and lower HbA1c values [6]. The mechanism of action is unknown. Insulin receptors are located on every cell in the body. They have a 4-8minute cycling time for insulin pulses. Theoretically, PIR promotes upregulation of insulin receptors hence its name. The underlying metabolic derangement with diabetes is failure of glucose uptake by cells. In a PIR treatment both insulin and glucose are given, and the blood glucose level is kept steady. Therefore, in a PIR treatment, glucose is driven into the cells [6,21]. In our presented case, GD had PIR treatment with his second wound.
Limitations
This case report describes the care received by a single patient at a single facility for two sequential diabetic foot wounds. He received standard and adjunctive care including PIR, a novel therapy that we describe. Conclusions should not be drawn from a single case. We are in the process of beginning an IRB-approved clinical trial to evaluate PIR as an adjunctive wound therapy.
Conclusion
In this case study we presented a patient who had two sequential left diabetic foot wounds. He received standard care as well as aggressive use of adjunctive wound care modalities. In both, he failed to achieve 50% wound area reduction at 4 weeks. As predicted by the Sheehan et al study of 2003, he failed to heal at 12 weeks with both wounds. However, our patient did heal both wounds by 16 weeks with aggressive use of adjunctive wound care techniques including: NPWT, HBOT, skin substitutes, topical collagen, and PIR. PIR is a novel therapy and warrants further study in diabetic wound care.
Acknowledgement
None.
Conflict of Interest
None.
References
- National Diabetes Statistics Report. Centers for Disease Control and Prevention.
- World Health Organization. Diabetes.
- Tomic D, Shaw JE and Magliano DJ (2022) The burden and risks of emerging complications of diabetes mellitus. Nat Rev Endocrinol 18(9): 525-539.
- Diabetic wound care: Foot health: Patients. APMA. 2019.
- Harley E and Smith AM Effect of Physiologic Insulin Resensitization Therapy in Patients with Diabetes, Department of Internal Medicine, Mercer University School of Medicine.
- Greenway F, Loveridge B, Grimes RM, Tucker TR, Alexander M, et al (1884) Physiologic Insulin Resensitization as a Treatment Modality for Insulin Resistance Pathophysiology 23(3): 1884.
- Everett E and Mathioudakis N (2018) Update on management of diabetic foot ulcers. Ann N Y Acad 1411(1): 153-165.
- Mościcka P, Cwajda Białasik J, Jawień A and Szewczyk MT (2023) Fluorescence - modern method of the diagnosis of chronic wounds on the example of venous leg ulcer. Postepy Dermatol Alergol 40(1): 66-671.
- Hingorani A, LaMuraglia GM, Henke P, Meissner MH, Loretz L, et al (2016) The management of diabetic foot: a clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. J Vasc Surg. 63(2 Suppl): 3S-21S.
- Ji S, Liu X, Huang J, Bao J, Chen Z, et al (2021) Consensus on the application of negative pressure wound therapy of diabetic foot wounds. Burns Trauma. 9: tkab018.
- Buckley CJ, Cooper JS (2023) Hyperbaric Oxygen Effects On Angiogenesis. [Updated 2023 Sep 4]. In: StatPearls [Internet]. Treasure Island.
- Burgess JL, Wyant WA, Abdo Abujamra B, Kirsner RS, Jozic I (2021) Diabetic Wound-Healing Science. Medicina (Kaunas). 8;57(10): 1072.
- Zhou D, Fu D, Yan L, Xie L (2023) The Role of Hyperbaric Oxygen Therapy in the Treatment of Surgical Site Infections: A Narrative Review. Medicina (Kaunas) 59(4): 762.
- Snyder D, Sullivan N, Margolis DK and Schoelles SM (2020) Skin Substitutes for Treating Chronic Wounds [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US).
- Research Protocol: Skin Substitues for Treating Chronic Wounds. Content last reviewed January 2020. Effective Health Care Program, Agency for Healthcare Research and Quality, Rockville.
- Savoji H, Godau B, Hassani MS, Akbari M (2018) Skin tissue substitutes and biomaterial risk assessment and testing. Front Bioeng Biotechnol 26(6): 86.
- Bay C, Chizmar Z, Reece EM, Yu JZ, Winocour J, Vorstenbosch J, et al (2021) Comparison of Skin Substitutes for Acute and Chronic Wound Management. Semin Plast Surg 35(3): 171-180.
- Roy A, Mantay M, Brannan C and Griffiths S (2022) Placental Tissues as Biomaterials in Regenerative Medicine. Biomed Res Int.
- Mathew-Steiner SS, Roy S, Sen CK (2021) Collagen in Wound Healing. Bioengineering (Basel) 8(5): 63.
- Mathew Steiner SS, Roy S and Sen CK (2021) Collagen in Wound Healing. Bioengineering (Basel) 8(5): 63.
- Lewis ST, Greenway F, Tucker TR, Alexander M, Jackson LK, et al (2023) A Receptor Story: Insulin Resistance Pathophysiology and Physiologic Insulin Resensitization's Role as a Treatment Modality. Int J Mol 24(13): 10927.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.