Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Association Between Impaired Uterine Perfusion and Inherited Thrombophilia in Infertile Patients
*Corresponding author: Arianna Pacchiarotti MD PhD, Via Pandosia, IVF Center San Filippo Neri-Responsible medical treatment, Prof University Sapienza Rome.
Received: May 29, 2024; Published: June 10, 2024
DOI: 10.34297/AJBSR.2024.22.003017
Abstract
Introduction: Heritable thrombophilia’s are a group of genetic disorders of blood coagulation, resulting in an increased risk of thrombosis. Among this group, the most common deficiencies are related to mutations of the protein C, protein S and anti-thrombin III genes.
Woman with decreased placental blood flow during pregnancy have been found to be carriers of prothrombotic mutations, and a reduced pregnancy rate (PR) has been reported in women with impaired uterine perfusion
Objective: The aim of this study is to evaluate the possible association between impaired uterine arteries and genetic polymorphism of trombophilic markers in patients with unexplained infertility.
Material and methods: In our prospective study, we evaluated the uterine artery perfusion through transvaginal colour-pulsed Doppler ultrasonography. The study was conducted on a cohort of 148 infertile patients aged between 26-37 years old.
Results: Our results showed a statistically significant association between trombophilic polymorphism mutations and impaired uterine arteries only with simultaneous presence of two or three mutations.
Conclusions: This study shows that the increased resistance of the uterine arteries is positively correlated to the presence of at least two genetic polymorphisms for acquired thrombophilia: such polymorphisms, when combined, show a high statistical significance in causing uterine blood flow alterations. The mutations studied by our group could cause alteration in the uterine blood flow, resulting in failure both in a spontaneous pregnancy and in those induced by Medically Assisted Procreation.
Introduction and Aim of the Study
Heritable thrombophilias are a group of genetic disorders of blood coagulation, that result in an increased risk of thrombosis. Heritable deficiencies of the endogenous anticoagulants have been recognized for some years now: the first description of familiar deficiency of anti-thrombin III in 1965 was followed by the report on protein C deficiency in 1981 and shortly after by the discovery of the deficiency in protein S. In 1993, Bertina, et al., described the condition of activated protein C resistance (APC-R) observed by plasma-based clotting assay [1], and shortly afterwards, the point mutation R506Q, at cleavage site factor V, resulting in factor V Leiden mutation [2].
Mild-to-moderate hyperhomocysteinemia is also a demonstrated risk factor for arterial and venous thrombosis [3].
A recent study described guanine-to-adenine mutation at nucleotide 20210 in the prothrombin gene is associated with higher serum concentrations of prothrombin, and an increased risk of venous thromboembolism, heart attack and cerebral vein thrombosis. Woman with decreased placental blood flow during pregnancy have been found to be carriers of prothrombotic mutations [4,5].
Uterine receptivity is one of the most important factors in determining successful implantation [6-9]. Several studies showed that failure to conceive might be associated with an increased resistance in the uterine arteries [10,11]. Implantation of fertilized eggs requires dilatation of endometrial blood vessels [9]. A reduced pregnancy rate (PR) has been reported in women with impaired uterine perfusion [10-13].
Uterine artery perfusion is usually investigated through transvaginal colour-pulsed Doppler ultrasonography (US), assessing the blood flow in the ascending branch of the uterine artery, which is depicted by a waveform in the spectral analysis. The qualitative assessment of the waveform gives the operator relevant information about the blood flow through the uterine artery: for instance, the presence of an appropriate diastolic flow reflects an adequate blood flow in the vessel, while the detection of a protohistoric notch suggests high impedance [8,14,15].
In the literature, the most accurate index to predict an impaired uterine artery blood flow is the pulsatility index (PI) [16,17]. In fact, this index is shown to be very useful to quantify the diastolic blood flow, which can’t be estimated through the evaluation of the Resistance Index (RI).
A mean value of PI>3.0 is predictive of pregnancy failure, whereas a PI value between 2 and 2.99 is considered the best value for a woman, because most likely she will become pregnant [14], whereas a resistance index (RI)>0.92 is predictive of pregnancy failure [10].
Given these premises, the aim of our study was to evaluate the possible association between impaired uterine arteries and genetic polymorphism of trombophilic markers in patients with unexplained infertility.
Materials and Methods
Between January 2013 and May 2014, we evaluated 148 consecutive infertile patients through basal uterine arteries Doppler velocimetry. In this prospective study, computerized randomization was made between aged 26-37 years patients with the following criteria:
1) male or tubal infertility;
2) serum levels of FSH and LH on day 3 of the ovarian cycle<12 IU/L;
3) regular menstrual cycle;
4) normal uterine cavity;
5) absence of antiphospholipid syndrome (APS) and Lupus anti-coagulant;
6) normal Body Mass Index.
Uterine arteries Doppler velocimetry evaluation in the midluteal phase of menstrual cycle was performed through a Duplex Colour Doppler machine (Sonoace 8000 SE) provided with an endocavitary 6.5 MHz probe. A high-pass filter at 50 Hz was kept in order to ensure that low frequencies patterns were not artificial. The flow velocimetry waveforms were obtained from the ascending main branch of the uterine arteries on both sides (left and right) of the uterine cervix in a longitudinal plane before it enters the uterus, thus keeping the insolating angle between the vessel and the ultrasound beam <30°. The Doppler gate was positioned when a vessel with good colour signal was identified on the screen. The Pulsatility Index (PI) was manually calculated when at least three similar consecutive waveforms of good quality were obtained. Doppler evaluation was performed only by one operator to avoid inter-observer variation. Furthermore, the mean value of two measurements was considered to avoid intra-observer variation.
The PI was calculated whenever we performed uterine arteries Doppler velocimetry in non-pregnant women, since in these patients it is frequently observed the absence of end diastolic flow: in these cases, RI is always 1.0. Furthermore, the RI does not consider differences in the quality of the diastolic blood flow. The PI, on the contrary, is useful in quantifying diastolic blood flow. According to these premises, PI should be performed to better evaluate uterine arteries blood flow.
Patients were divided into two groups: Group A (study group)-49 patients with high pulsatility index in at least one of uterine arteries; Group B (control group)-99 patients with normal uterine arteries.
The cut off considered was PI>3.0, as what it is stated in the literature [14].
All patients underwent a screening, through PCR procedure, for the three main trombophilic markers: factor V Leiden gene mutation, mutation G20210A of prothrombin (PT) and homozygous mutation of gene C677T of methylenetetrahydrofolate reductase (MTHFR) [18-20].
Oligonucleotides used as primers were: 5V-CATACTACAGTGACGTGGAC-3Vand 5V-TGTTCTCTTGAAGGAAATGC- 3V for FV Leiden; 5VTCTAGAAACAGTTGCCTGGC3V and 5V-ATAGCACTGGGAGCATTGAAGC- 3V for the mutation G20210A of PT gene; 5V-AGGGAGCTTTGAGGCTGACCTGAA-3V e 5V-ACGATGGGGCAAGTGATGCCCATG-3V for the C677T mutation of the MTHFR gene.
Main outcomes were PI, presence of trombophilic polymorphism alone or combined.
Statistical analysis was performed using the JMP software (version 4.0.4; SAS Corp., Cary, NC). The parameters were compared using the student’s t-test for independent data and χ2-test, setting the significance level at p ≤ 0.05. The ANOVA test was also used to analyze continuous variables, including primary and secondary outcome parameters. The difference between treatments was evaluated using a one-sided, 95% confidence interval. No adjustment for multiplicity was performed. The difference had greater significance when the linear mixed model, which controls for intrasubject variation was used to compare data across all time points (P ≤ 0.001). Statistical Power calculation was based on an α level of 0.05 (two-tailed test) with 80% power to detect a 20% difference with 23 evaluable patients per group.
Results
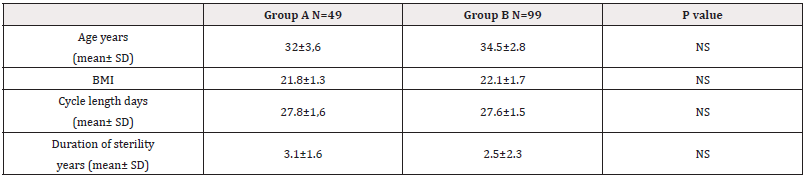
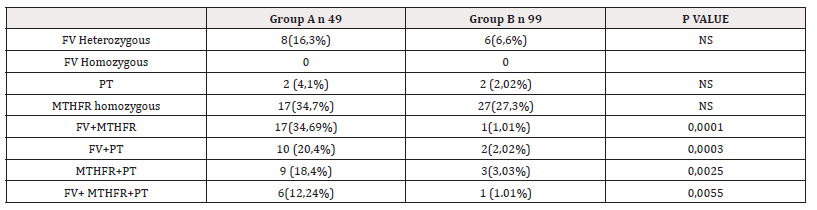
Patients resulted similar for demographic data (Table 1). We did not find patients with homozygous mutation of factor V Leiden. Furthermore, we did not consider MTHFR heterozygous mutation because of its frequency in the general population, which made it not meaningful for our study.
Our results showed a statistically significant association between trombophilic polymorphism mutations and impaired uterine arteries only with simultaneous presence of two or three mutations: factor V Leiden and gene C677T of methylenetetrahydrofolate reductase (34,69% vs 1,01% respectively in group A and B P=0,0001); factor V Leiden and mutation G20210A of prothrombin gene (20,4% in Group A vs 2,02% in group B , p=0.0003); gene C677T of methylenetetrahydrofolate reductase mutation and factor V Leiden and mutation G20210A of prothrombin gene (18,4% in study group vs 3,03% in control group P=0,0025) and factor V Leiden mutation, mutation G20210A of prothrombin gene and gene C677T of methylenetetrahydrofolate reductase mutation (12,24% vs 1.01% in group A and B respectively) (Table 2).
Conclusion
This study shows that the increased resistance of the uterine arteries is positively correlated with the presence of at least two genetic polymorphisms for acquired thrombophilia.
The identification of these polymorphisms allows to set the most accurate treatment immediately, avoiding therapies that may not work. It also gives us important information on the possible therapeutical management to be set during the entire pregnancy [5].
Anyway, we need to point out that screening tests, for both infertile and pregnant women, do not always include these polymorphisms, due to their high frequency in the general population.
The purpose of this study is to demonstrate that these polymorphisms, taken individually, are not sufficient to explain an alteration in blood flow, especially for what concerns the uterus; on the other hand, they seem to have a higher statistical significance when combined [21]. The mutations studied by our group could cause alteration in the uterine blood flow, resulting in implantation failure both in a spontaneous pregnancy and in those induced by Medically Assisted Procreation.
Implantation failure is one of the main limitations that have always afflicted experts in the field of infertility.
Edassery, et al., identified antigens associated with the most frequent immunoreactions for ovarian autoimmunity associated with infertility [22].
A significant difference in endometrial cadmium concentration was found between women with unexplained infertility and fertile women. This suggests that cadmium may be a contributing factor in the etiology of unexplained infertility [23,24].
Oxidative stress plays, as well, an important role in oocytes quality of patients with infertility [25].
In 2008 Bellver, et al., tried to find an association between thrombophilia and thyroid autoimmunity in unexplained infertility, implantation failure and recurrent spontaneous abortion; they concluded that prevalence of acquired and inherited thrombophilia is high, but they are not associated with unexplained infertility, implantation failure and recurrent spontaneous abortion; despite that, there is evidence of a higher prevalence of thyroid autoimmunity in these patients [26].
In 1997 Tohma suggested the importance of the evaluation of uterine blood flow in unexplained infertility [27].
Patients with increased resistance of the uterine arteries should be adequately treated before beginning an IVF attempt [28]. For this purpose, there are several different medications that can be used, the first line treatment being acetylsalicylic acid, followed by either heparin or nitroglycerin in case of failure of the previous treatments [29].
Acknowledgements
None.
Fundings
None.
Author Contributions
Pacchiarotti A.: design of the study, validation and final approval of the version of the article.
Gangale M.F., Sangiuliano C. and Pannuzzi C.: acquisition, analysis and interpretation of data; drafting of the article, critical revisions.
ORCID
Arianna Pacchiarotti: 0000-0003-685X
Conflict of Interest
The authors declare that they have no conflict of interest to declare
Data availability statement: All data generated or analyzed during this study are included in this published article [and/or its supplementary material].
Data Availability Statement
All data generated or analyzed during this study are included in this published article [and/or its supplementary material].
References
- Bertina RM, Koeleman BP, Koster T, Rosendaal FR, Dirven RJ, et al. (1994) Mutation in blood coagulation factor V associated with resistance to activated protein C. Nature 369(6475): 64-67.
- Ivanov PD, Komsa Penkova RS, Konova EI, Kovacheva KS, Simeonova MN, et al. (2009) Association of inherited thrombophilia with embryonic and postembryonic recurrent pregnancy loss. Blood Coagul Fibrinolysis 20(2): 134-140
- Pacchiarotti A, Mohamed MA, Micara G, Linari A, Tranquilli D, et al. (2007) The possible role of hyperhomocysteinemia on IVF outcome. J Assist Reprod Genet 24(10): 459-462.
- Grandone E, Margaglione M (2003) Inherited thrombophilia and gestational vascular complications. Best Pract Res Clin Haematol 16(20): 321-332.
- Chatzidimitriou M, Chatzidimitriou D, Mavridou M, Anetakis C, Chatzopoulou F, et al. (2017) Thrombophilic gene polymorphisms and recurrent pregnancy loss in Greek women. Int J Lab Hematol 39(60): 590-595.
- Kupesic S (2004) Vascularisation de l'utérus en 3D et implantation [Three-dimensional ultrasonographic uterine vascularization and embryo implantation]. J Gynecol Obstet Biol Reprod (Paris) 33: 18-20.
- Kupesic S, Kurjak A (1997) The assessment of uterine and ovarian perfusion in infertile patients. Eur J Obstet Gynecol Reprod Biol 71:151-154.
- Nakatsuka M, Habara T, Noguchi S, Konishi H, Kudo T (2003) Impaired uterine arterial blood flow in pregnant women with recurrent pregnancy loss. J Ultrasound Med 22(1): 27-31.
- Conti E, Zezza L, Ralli E, Caserta D, Musumeci MB, et al. (2013) Growth factors in preeclampsia: a vascular disease model. A failed vasodilation and angiogenic challenge from pregnancy onwards? Cytokine Growth Factor Rev 24: 411-425.
- Battaglia C, Larocca E, Lanzani A, Valentini M, Genazzani AR (1990) Doppler ultrasound studies of the uterine arteries in spontaneous and IVF stimulated ovarian cycles. Gynecol Endocrinol 4(4): 245-250.
- Giugliano E, Cagnazzo E, Vesce F, Giugliano B, Caserta D, e al. (2014) Doppler velocimetry of the ovarian artery as a tool to detect LH surge in stimulated cycles. Gynecol Endocrinol 30(9): 627-631.
- Giugliano E, Cagnazzo E, Giugliano B, Vesce F, Caserta D, et al. (2014) Can Doppler study of the ovarian artery predict the fertility outcome of intrauterine insemination? J Clin Ultrasound 42(6): 331-335.
- Malinowski AK (2021) The Pathophysiology of Hypercoagulability and Infertility. Semin Reprod Med 39(1-2): 34-61.
- Salle B, Bied Damon V, Benchaib M, Desperes S, Gaucherand P, et al. (1998) Preliminary report of an ultrasonography and colour Doppler uterine score to predict uterine receptivity in an in-vitro fertilization programme. Hum Reprod 13(6): 1669-1673.
- El Mazny A, Abou Salem N, Elshenoufy H (2013) Doppler study of uterine hemodynamics in women with unexplained infertility. Eur J Obstet Gynecol Reprod Biol 171(1): 84-87.
- Steer CV, Campbell S, Tan SL, Crayford T, Mills C, et al. (1992) The use of transvaginal color flow imaging after in vitro fertilization to identify optimum uterine conditions before embryo transfer. Fertil Steril 57(2): 372-376
- Shui X, Yu C, Li J, Jiao Y (2021) Development and validation of a pregnancy prediction model based on ultrasonographic features related to endometrial receptivity. Am J Transl Res 13(6): 6156-6165.
- Pietropolli A, Giuliani E, Bruno V, Patrizi L, Piccione E, et al. (2014) Plasminogen activator inhibitor-1, factor V, factor II and methylenetetrahydrofolate reductase polymorphisms in women with recurrent miscarriage. J Obstet Gynaecol 34(3): 229-234.
- Long S, Goldblatt J (2016) MTHFR genetic testing: Controversy and clinical implications. Aust Fam Physician 45(4): 237-240.
- Yengel I, Yorulmaz T, Api M (2020) Association between FVL G1691A, FII G20210A, and MTHFR C677T and A1298C polymorphisms and Turkish women with recurrent pregnancy loss. Med Glas (Zenica) 17(1): 129-135.
- Milenkovic J, Milojkovic M, Mitic D, Stoimenov TJ, Smelcerovic Z, et al. (2020) Interaction of thrombophilic SNPs in patients with unexplained infertility-multifactor dimensionality reduction (MDR) model analysis. J Assist Reprod Genet 37(6): 1449-1458.
- Edassery SL, Shatavi SV, Kunkel JP, Hauer C, Brucker C, et al. (2010) Autoantigens in ovarian autoimmunity associated with unexplained infertility and premature ovarian failure. Fertil Steril 94(7): 2636-2641.
- Tanrıkut E, Karaer A, Celik O, Celik E, Otlu B, et al. (2014) Role of endometrial concentrations of heavy metals (cadmium, lead, mercury and arsenic) in the aetiology of unexplained infertility. Eur J Obstet Gynecol Reprod Biol 179: 187-190.
- Lee S, Min JY, Min KB (2020) Female Infertility Associated with Blood Lead and Cadmium Levels. Int J Environ Res Public Health 17(5): 1794.
- Gharagozloo P, Aitken RJ (2011) The role of sperm oxidative stress in male infertility and the significance of oral antioxidant therapy. Hum Reprod 26(7): 1628-1640.
- Bellver J, Soares SR, Alvarez C, Muñoz E, Ramírez A, et al. (2008) The role of thrombophilia and thyroid autoimmunity in unexplained infertility, implantation failure and recurrent spontaneous abortion. Hum Reprod 23(2): 278-284.
- Tohma H, Hasegawa I, Sekizuka N, Tanaka K (1997) Uterine blood flow. Assessment in an intrauterine insemination program for unexplained infertility. J Reprod Med 42(8): 463-466.
- Han AR, Han JW, Lee SK (2021) Inherited thrombophilia and anticoagulant therapy for women with reproductive failure. Am J Reprod Immunol 85(4): e13378.
- Ralli E, Zezza L, Lillo R, Conti E, Comito C, et al. (2013) Tromboembolismo venoso in gravidanza: attuale stato dell'arte [Venous thromboembolism in pregnancy: current state of the art]. Minerva Med 104(5): 563-578.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.