Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Dysbiotic Oropharyngitis Syndrome and Hybrid Treatment
*Corresponding author: Faramarz Ashoori, Departments of Otorhinolaryngology-Head and Neck Surgery, McGovern Medical School, The University of Texas Health Science Center at Houston (UTHealth); 6431 Fannin St, MSB 5.003 (C), Houston, TX 77030, USA.
Received: May 17, 2024; Published: May 22, 2024
DOI: 10.34297/AJBSR.2024.22.002989
Abstract
This observation comprises a newly identified syndrome, Dysbiotic Oropharyngitis Syndrome (DOS), characterized by a triad of oropharyngitis, dysbiosis, and Parkinson’s disease. The hybrid treatment of allopathic and homeopathic measures was practical, affordable, and long-lasting.
Keywords: Dysbiosis; Oropharyngitis; Parkinson’s; Levofloxacin; Terbinafine; Fluconazole
Introduction
There is mounting evidence to suggest that dysbiosis plays a role in neurodegenerative diseases such as Parkinson’s disease. [1] It has also been shown that probiotics could help treat pharyngotonsillitis. [2] The present report explored practical connections between three major health problems: a new type of recalcitrant ulcerative bacteria-Candida oropharyngitis, Advanced Parkinson’s Disease (APD), and Entero-Oral Dysbiosis (EOD) in the form of a syndrome. The report discusses the underlying mechanisms and provides a holistic approach to treatment, which could be beneficial in similar scenarios.
Case History
An 85-year-old woman visited us to treat her oropharyngitis, which lasted for a year, regardless of using various antibacterial and anticandida agents. She asked for effective and affordable treatment. Her vitals were normal, and apart from symptoms and signs of Advanced Parkinson’s Disease (APD), she did not have other systemic diseases. She was mentally alert. She had no teeth and was on PEG for gastric feeding. The feeding formula lacked supplemental probiotics and prebiotics. The oral cavity showed patches of ulcers, purulent exudate, and thrush-like lesions (Figures 1A, 1B & 1C). She had oral tremors and dystonia, which led to the exposure of her mouth to the air, causing xerostomia. She complained of having obstipation regardless of taking various stool softeners. She did not have drug allergies. Her medications included Carbidopa/Levodopa, Zolpidem, Nystatin, Augmentin, and synthetic stool softeners. Her lab results showed average values for CD4 and CD8 counts, CBC, CMP, TSH, T3, T4, IgG, IgM, IgE, and IgA, and vitamins B1, B12, and D. Based on the lab results and medication history, we concluded that the patient was not immunocompromised. Hybrid treatment included allopathic and homeopathic (for prevention) measures, as shown in the green panel in Figure 2. Allopathic treatment included Fluconazole (200mg tablet once daily for eight weeks), Terbinafine HCl (250mg tablet once daily for eight weeks), Levofloxacin (500 mg tablet once daily for two weeks), and oral debridement (Figures 1D & 1E). Homeopathic treatment and prevention, which continued through the 5-year course of following-up, included an oral spray of diluted yogurt (half-and-half with water, three times daily) to improve oral microbiome and salivary flow to address oral dysbiosis. We suggested administering diluted yogurt via PEG three times daily to enhance enteral dysbiosis. We recommended prune juice (one cup once a day) to treat obstipation and improve enteral dysbiosis by supplying natural prebiotics. Complete recovery was achieved within eight weeks, with no recurrence after a five-year follow-up (Figure 1F).
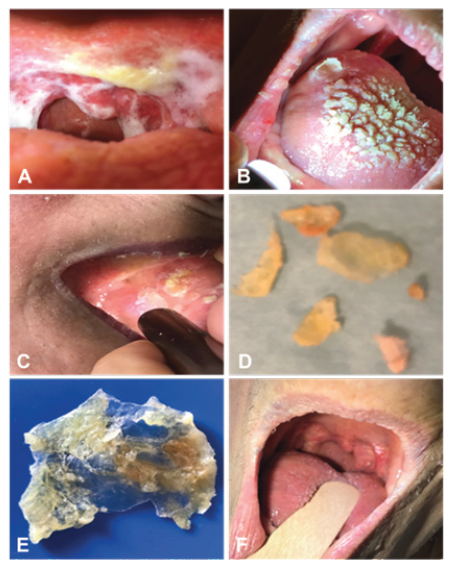
Figure 1: Oropharyngeal cavity before and after treatment. A: The inflamed throat is covered with purulent exudate. B: The tongue’s mucosa is inflamed and covered with thrush-like lesions. C: Sublingual ulcers. D: Debrided oral ulcers. E: A sheet of debrided necrotized palatal mucosa embedded with biofilm. F: The oropharyngeal mucosa has completely healed after eight weeks of hybrid therapy, with no recurrence in five years.
Discussion
Several reports suggest gut and oral microbiome alteration in Parkinson’s disease. [3] Our observation is the first clinical evidence linking Entero-Oral Dysbiosis (EOD), a new type of ulcerative oropharyngitis, and APD in the form of the syndrome. The syndrome’s pathophysiology and treatment mechanisms are shown in Figure 2. Despite the patient’s advanced age and severe illness, based on the wish of the patient and kin, we proposed a hybrid treatment. For allopathic treatment we used Terbinafine and Fluconazole because they are reported to treat resistant and colonized candidiasis. [4] We used Levofloxacin to eradicate resistant and colonized bacteria. It could also improve tremors related to Parkinson’s by suppressing GABAergic activity in the brain. [5] The patient’s caregivers also reported some improved oral tremors while on Levofloxacin. Homeopathic prevention was chosen because no side effects have been reported for long-term use. We chose yogurt because it contains affordable cultured probiotics that can survive in the gut. [6] We recommended using prune juice to treat obstipation because of the successful previous report. [7] Characterizing oropharyngitis associated with APD and EOD as a syndrome caused by a cluster of complex interconnected factors leading to recognizable symptoms and signs was in light of the definition of the syndrome. [8] Looking at this illness as a syndrome helped us to understand the pathophysiology and implement etiopathological treatment strategies. Although these findings are specific to this case, the increasing number of patients with Parkinson’s disease, dysbiosis, or those on enteral feeding should draw attention to identifying and managing similar cases.

Figure 2: Pathophysiology (red) and hybrid therapy (green) of Dysbiotic Oropharyngitis Syndrome (DOS). The major components of DOS were APD, EOD, and a new type of ulcerative oropharyngitis. Apparently, two groups of internal and external factors could cause EOD to lead to DOS. Internal factors such as motor neuropathy could cause oromandibular tremors and dystonia, exposing the oral cavity to air and causing xerostomia, oral dysbiosis, and ulcerative oropharyngitis. Autonomic neuropathy could cause xerostomia and obstipation. Changing the natural microbiome and metabolome of the mouth and gut could lead to EOD. External factors (not shown) such as poor oral hygiene, misuse of antibacterial and antifungal agents, and prolonged use of enteral feeding formula lacking probiotics and prebiotics may also contribute to EOD and developing DOS. To effectively treat DOS, we created a hybrid treatment using allopathic and homeopathic measures, which turned out to be effective and confirmed our hypothesis.
Conflict of Interest Disclosures
None reported.
Acknowledgment
We thank the patient for granting permission to publish this information and Dr. Joseph Jankovic, MD, Professor and Distinguished Chair in Movement Disorders at Baylor College of Medicine in Houston, Texas, for his initial diagnosis and treatment of the patient’s Parkinson’s Disease.
References
- Wang Q, Luo Y, Chaudhuri RK, Reynolds R, Tan KE, Pettersson S (2021) The role of gut dysbiosis in Parkinson’s disease: mechanistic insights and therapeutic options. Brain 144(9): 2571-2593.
- La Mantia I, Gelardi M, Drago L, C Vicini, C Berardi, et al. (2020) Probiotics in the add-on treatment of pharyngotonsillitis: a clinical experience. J Biol Regul Homeost Agents 346(1): 11-18.
- Jo S, Kang W, Hwang YS, Lee SH, Park KW, et al. (2022) Oral and gut dysbiosis leads to Functional alterations in Parkinson’s disease. npj Parkinson's disease pp. 8.
- Ghannoum MA, Elewski B (1999) Successful Treatment of Fluconazole-Resistant Oropharyngeal Candidiasis by combination of Fluconazole and Terbinafine. Clin Diagn Lab Immunol 6(6): 921-923.
- Ayoubi NE, Sawaya R, Raja Sawaya R (2016) Does Levofloxacin Improve Parkinsonian Features or is the improvement only coincidental? Clin Neuropharmacol 39(6): 335-336.
- Elli M, Callegari ML, Ferrari S, Bessi E, Cattivelli D, et al. (2006) Survival of Yogurt Bacteria in the Human Gut. Appl Environ Microbiol. 72(7): 5113-5117.
- Koyama T, Nagata N, Nishiura K, Miura N, Kawai T, et al. (2022) Prune juice containing sorbitol, pectin, and polyphenol ameliorate subjective complaints and hard feces while normalizing stool in chronic constipation: A randomized placebo-controlled tial. Am J Gastroenterol 117(10): 1714-1717.
- Franz C, Bryant KT, Richard Ph, Ann KM and Fred W (2003) Diagnoses, Syndromes, and Disease: A knowledge representation problem. AMIA Annu Symp Proc pp. 802.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.