Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Endovascular Treatment of a Ruptured Giant Splenic Artery Aneurysm with Viabahn Stent-Grafts: A Case Report
*Corresponding author: Roberto Castellana, Department of Diagnostic and Interventional Radiology, U. Parini Regional Hospital, Viale Ginevra 3,11100 Aosta, Italy.
Received: April 26, 2024; Published: May 1, 2024
DOI: 10.34297/AJBSR.2024.22.002955
Abstract
Background: Endovascular techniques are typically the preferred approach for treating patients with splenic artery aneurysms.
Case Presentation: We present the case of a 57-year-old man with upper left abdominal pain for 6 months. CT angiography revealed a 5 cm aneurysm of the splenic artery and endovascular treatment was recommended. While performing the procedure, the splenic artery aneurysm ruptured. Consequently, two Viabahn stent-grafts were deployed, successfully excluding the aneurysm. At the 6-month follow-up CT scan, evidence of the correct exclusion location of the stent-grafts was observed. The patient became completely asymptomatic at follow-up.
Conclusions: The endovascular treatment of ruptured giant splenic artery aneurysms may be successfully performed with Viabahn stent-grafts.
Keywords: Splenic artery aneurysm, Visceral artery aneurysm, gia$nt aneurysm, Endovascular treatment, Stent-graft, Case report
List of Abbreviations: CT: Computed Tomography; SAA: Splenic Artery Aneurysms
Background
Vascular artery aneurysms are a rare condition, with estimated prevalence rates ranging from 0.01% to 0.2% [1]. Splenic artery aneurysms (SAAs) constitute the most prevalent type (60%) of visceral artery aneurysms [2].
Various treatment options are presently available for SAAs, encompassing open or laparoscopic surgery as well as endovascular techniques. [3]. Due to its reduced invasiveness and lower morbidity compared to surgery, the endovascular approach is generally preferred for unruptured SAAs. [1,4]. Endovascular techniques include embolization with coils, liquid embolic agents, glue, and percutaneous thrombin injection; endovascular repair with stent-grafts, flow-diverting stents, neurovascular double-layer stents, overlapping uncovered stents and combined techniques [1].
Although endovascular treatment of SAAs can usually be safely performed, complications may occur. Splenic infarction, abscesses, coil migration, splenic artery dissection and artery rupture have been described [1,5].
Unlike transcatheter embolization, which carries a potential risk of causing ischemia in the target organ, stent grafting effectively seals off the aneurysm while blood flow through the affected visceral artery is maintained effectively [1].
We report the case of an intra-procedural rupture of a giant (≥ 5cm) SAA, successfully managed by the placement of Viabahn stent-grafts.
The article adheres to the CARE (Case Report) guidelines, and the CARE checklist is documented in Table 1. The patient provided informed consent for publication.
Case Presentation
We present the case of a 57-year-old man who complained of upper left abdominal pain for 6 months. A CT angiography showed a 5 cm splenic artery aneurysm (Figure 1). His past medical history was not significant, and he had no significant comorbidities.

Figure 1: Preoperative CT angiography. MIP (A) and 3D reconstructions (B and C) show a 5 cm splenic artery aneurysm (arrows). The diameter of the splenic artery is 5 mm (D).
After a multidisciplinary discussion, because of the symptoms and the risk of spontaneous rupture in relation to the remarkable size of the aneurysm, endovascular treatment was recommended. A Cardiatis Multilayer Flow Modulator stent (7X60mm) was initially chosen (Cardiatis, Isnes, Belgium). Under conscious sedation and local anesthesia, the right femoral artery access was obtained and a guidewire was delivered into the distal end of the splenic artery. A 7 Fr guiding multipurpose catheter (Destination, Terumo Medical Corp., Somerset, NJ) was placed over the guidewire. Then, a super-stiff guidewire (Steerable 200 cm) replaced the catheter in order to deliver the Cardiatis stent. Unfortunately, during these maneuvers, the rupture of the SAA occurred. Due to this complication, the treatment strategy was modified. An occluding balloon-catheter was deployed, and, subsequently, two 8 mm Viabahn stent-grafts were successfully placed under digital subtraction angiography roadmap guidance to exclude the aneurysm. Repeated angiography confirmed good location and shape of stent-grafts. Patency of the distal portion of the splenic artery was evidenced and no obvious residual aneurysm was visualized (Figure 2).
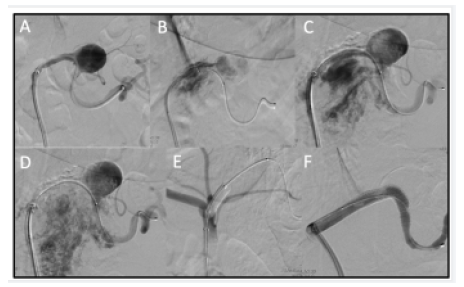
Figure 2: Digital subtraction angiography (A-F). During the catheterization, the rupture of the aneurysm occurred (B-D). The treatment strategy changed: an occluding balloon-catheter and two 8 mm Viabahn stent-grafts were deployed under digital subtraction angiography roadmap guidance, to exclude the aneurysm (E,F).
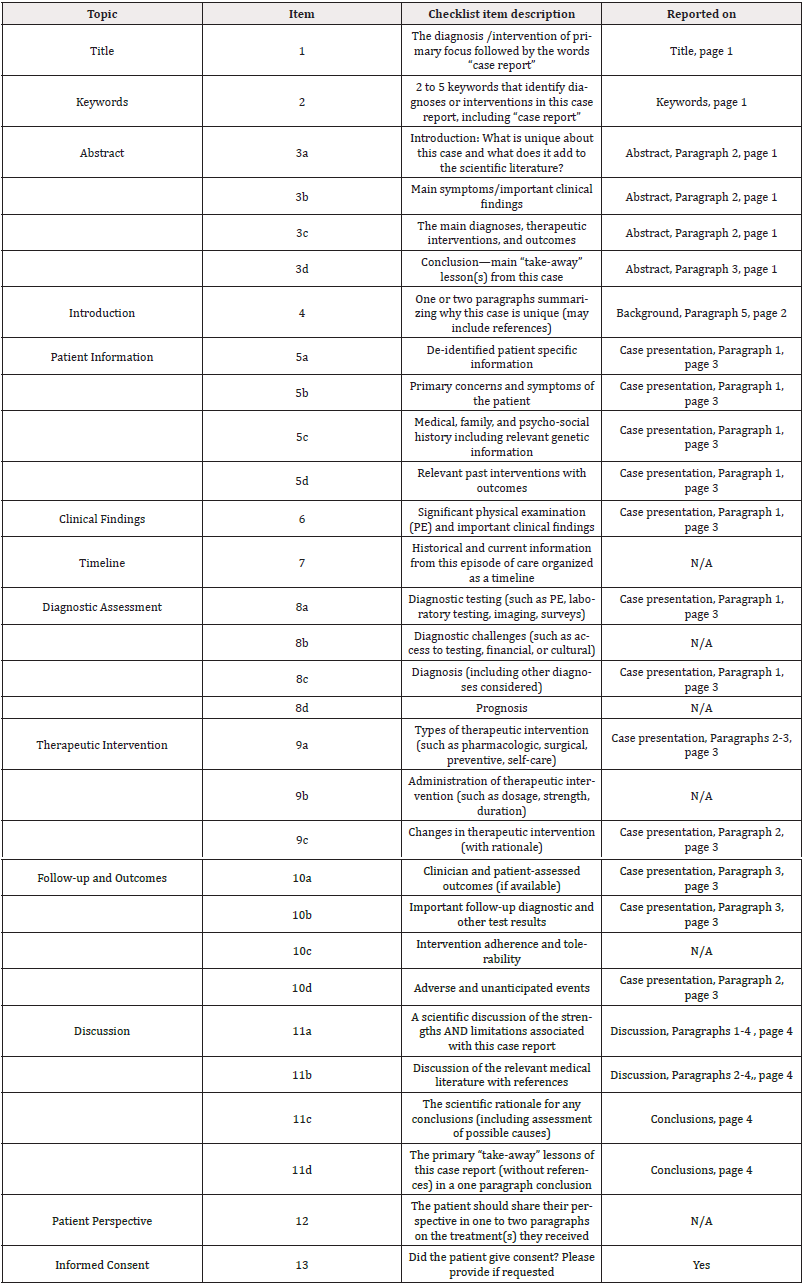
Complete exclusion of the aneurysm and patency of the splenic artery were confirmed at 6 months CT follow-up imaging (Figure 3). The patient became completely asymptomatic at follow-up.
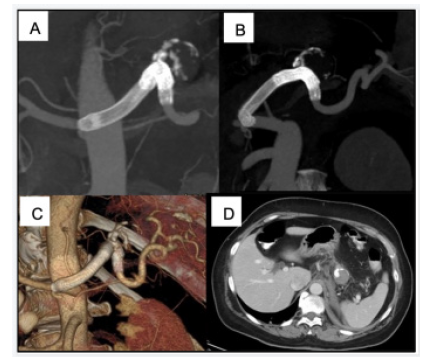
Figure 3: CT angiography at 6-month follow-up: MIP (A) and 3D (B, C) reconstructions show complete exclusion of the aneurysm, patency of the splenic artery, and correct location of stent-grafts. Axial CT image (D) evidence normal splenic parenchyma in the venous phase, without signs of complications.
Discussion
In our case report we successfully treated an intraoperative rupture of a giant SAA using Viabahn stent-grafts.
In patients with ruptured SAA discovered at laparotomy, the recommended treatment is surgery, with ligation of the splenic artery, with or without splenectomy [3]. However, in case of ruptured SAA diagnosed on preoperative imaging studies, both the surgical and endovascular techniques are appropriate options [1,3,6].
In our case, the SAA rupture occurred during the endovascular treatment and, therefore, the exclusion of the aneurysm was first approached endovascularly. Instead of a Cardiatis multilayer flow modulator, that maintains a reduced flow in the aneurysmal sac, we decided to use a Viabahn stent-graft, that can completely exclude the aneurysm.
The use of a Viabahn stent-graft in the treatment of acute ruptured SAAs has been rarely reported. Varnagy, et al., [7] and Ouchi, et al., [8] reported two cases of the successful endovascular exclusion of spontaneously ruptured SAAs using Viabahn stent-grafts in a 44-year-old-man and a 43-year-old man, respectively. Furthermore, Venturini, et al., reported the use of Viabahn stent-grafts in 25 emergency procedures for ruptured splenic artery pseudoaneurysms [1].
Conclusions
Endovascular treatment of SAAs has become the preferred first-line approach for patients with symptomatic, unruptured, or asymptomatic large-size aneurysms. The use of a Viabahn stent-graft can be an alternative to surgery for ruptured SAAs and is the recommended option when an SAA rupture occurs during endovascular procedures.
Declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent For Publication
Written consent to publish this case was obtained from the father of the patient.
Availability of Data and Materials
Not applicable.
Competing Interests
The authors declare that they have no competing interests.
Funding
No funding was obtained for this study.
Authors’ Contributions
RC was a major contributor in writing all the parts of the case report. CMEWP and MN provided valuable assistance in the writing process. During the writing process, GF, MR, MA, PP, MT, FL and DF contributed with critical feedback, playing a pivotal role in enhancing the report's overall quality and clarity. All authors contributed to the writing and review of the manuscript and approved the final version for submission.
Acknowledgments
Not applicable.
References
- Venturini M, Marra P, Colombo M, Panzeri M, Gusmini S, et al. (2018) Endovascular Repair of 40 Visceral Artery Aneurysms and Pseudoaneurysms with the Viabahn Stent-Graft: Technical Aspects, Clinical Outcome and Mid-Term Patency. Cardiovasc Intervent Radiol 41(3): 385-397.
- Uy PPD, Francisco DM, Trivedi A, O Loughlin M, Wu GY (2017) Vascular Diseases of the Spleen: A Review. J Clin Transl Hepatol 5(2): 152-164.
- Chaer RA, Abularrage CJ, Coleman DM, Eslami MH, Kashyap VS, et al. (2020) The Society for Vascular Surgery clinical practice guidelines on the management of visceral aneurysms. J Vasc Surg 72(1S): 3S-39S.
- Lagana D, Carrafiello G, Mangini M, Fontana F, Dizonno M, et al. (2005) Endovascular treatment of splenic artery aneurysms. Radiol Med 110(1-2): 77-87.
- Ekeh AP, Khalaf S, Ilyas S, Kauffman S, Walusimbi M, et al. (2013) Complications arising from splenic artery embolization: a review of an 11-year experience. Am J Surg 205(3): 250-254.
- Lim HJ (2020) A review of management options for splenic artery aneurysms and pseudoaneurysms. Ann Med Surg (Lond) 59: 48-52.
- Varnagy D, Sendzischew M, Hertz JA, Sendzischew H (2007) Endovascular management of a ruptured splenic artery aneurysm. Vasc Endovascular Surg 41(1): 68-72.
- Ouchi T, Kato N, Nakajima K, Higashigawa T, Hashimoto T, et al. (2018) Splenic Artery Aneurysm Treated With Endovascular Stent Grafting: A Case Report and Review of Literature. Vasc Endovascular Surg 52(8): 663-668.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.