Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Preoperative Assessment of Patients with Obstructive Sleep Apnea - Implications for Anesthesiologists
*Corresponding author: Sara Bar Yehuda, Anesthesiology Department, Shamir Medical Center, Zerifin, Israel.
Received: May 10, 2024; Published: May 15, 2024
DOI: 10.34297/AJBSR.2024.22.002979
Abstract
Background: Obstructive Sleep Apnea (OSA) is a sleep-disordered breathing, with high prevalence among patients who are about to be operated. The anatomical and clinical characteristics of OSA play a major role in the development of complications of the anesthesia process. However, OSA remains undiagnosed. The STOP-BANG questionnaire is used to identify OSA. The aim of the current study was to identify patients with OSA risk factors among patients who were about to have an elective surgery.
Methods: It was a retrospective study in which demographic and clinical data of patients who underwent elective surgeries were collected. The score of the STOP-BANG questionnaire was recorded.
Results: A total of 282 patients were divided to STOP-BANG (22%) and no STOP-BANG groups. The most common comorbidities in both groups were hypertension, obesity and diabetes mellitus. Hypertension and obesity were the most common morbidities among the Intermediate risk group as identified by the STOP-BANG questionnaire.
Conclusions: The current study further demonstrated that risk factors for OSA which exist in patients who are about to undergo a surgical procedure but were not diagnosed with OSA prior to the surgery. In light of the data, it is recommended that the STOP-BANG questionnaire (or any other OSA screening questionnaires) must be filled and a special anesthesia strategy must be adopted for those adult patients with a risk for OSA before the surgery.
Keywords: Obstructive sleep apnea, Anesthesia, Complications, Perioperative screening, Stop-Bang
Abbreviations: OSA: Obstructive Sleep Apnea, P-SAP: Perioperative Sleep Apnea Prediction Score
Introduction
Obstructive Sleep Apnea (OSA) is a form of sleep-disordered breathing, which is prevalent among patients about to undergo surgery [1,2]. Patients with OSA experience recurrent closure of the upper airway during sleep, causing airflow interruption till full cessation. As a result of these apneic episodes and hypoxemia, arousal periods occur, disrupting the continuity and completeness of sleep [3].
The upper airway obstruction during sleep is usually caused by the anatomical narrowing of the upper airway, rendering it more susceptible to complete collapse when the pharyngeal tone decreases [3]. The decreased tone of the upper airway dilator muscles is a main factor of OSA pathogenesis. Blocking the airway induces a reduction in the ventilation and blood gas changes, stimulating both respiratory exertion and upper airway dilator muscle activity. This chain of events starts as a neuro-mechanical pressure that triggers the arousal from sleep, terminating the apnea event [4].
The impaired function of the upper airways in OSA induces intrathoracic pressure oscillations which leads to an increase in the activity of the sympathetic nervous system. The resulting hypoxia and the arousal from the sleep further increase the sympathetic nervous system activity. Due to the apnea, saturation is decreased and there is a demand for cardiac oxygen. Moreover, after the apneic episode, the blood pressure and heart rate markedly increase [5]. The variations in the upper airway and craniofacial anatomy that characterize OSA patients have been found to play a major role in the development of complications of the anesthesia process before and during surgery. Data from a systematic review conducted by Nagappa, et al., revealed that the rate of difficult intubation incidences was 3.46-fold higher in OSA vs. non-OSA patients. Not only that, but also the rate of difficult mask ventilation frequencies was 3.39-fold higher in the OSA vs. non-OSA patients and the rate of combined difficult intubation and difficult mask ventilation occurrences was 4.12-fold higher in the OSA vs. non-OSA patients [6]. It was also reported that premature exhumation in OSA patients caused airway collapse, which was then followed by the rapid development of severe negative pressure pulmonary edema from spontaneous ventilation against the obstructed airway [7]. It is well established that general anesthesia can be a risk for hypoxemia development and consequently major respiratory complications, intensive care units’ admissions and increased length of stay among OSA patients [8]. Drugs commonly used during general anesthesia (such as hypnotics, opioids and muscle relaxants) have been shown to reduce the tone of the upper-airway dilating muscles, the protective airway reflexes and the central respiratory drive, thereby inducing hypoxia and arousal [9].
Thus, patients with OSA who are about to undergo a surgical procedure requiring general anesthesia present significant challenges to anesthesiologists necessitating a special anesthesia strategy [10]. Implementation of specific perioperative actions could prevent critical, life-threatening conditions during surgery as well as serious postoperative events.
However, the majority of the pre-operated OSA patients remain undiagnosed [11]. Polysomnography is the gold standard of OSA diagnosis, yet the time and cost requirements caused this test to be problematic for routine preoperative use. Instead, patient interview, review of medical records, physical examination and the use of screening questionnaires can serve as clinical predictors of OSA existence. OSA screening questionnaires include the STOP-BANG Questionnaire, the Perioperative Sleep Apnea Prediction Score (P-SAP) and the Berlin Questionnaire [12].
The STOP-BANG questionnaire ranks the snoring, tiredness, observed apnea, blood pressure, body mass index, age, neck circumference and gender of the patient. It can be completed quickly and easily. This test has demonstrated a high sensitivity of 93% in detecting moderate to severe sleep apnea (apnea-hypopnea index> 15 events/h) and 100% in detecting severe sleep apnea (apnea-hypopnea index>30 events/h). Owing to its ease of use and high sensitivity, the STOP-BANG questionnaire has been widely utilized among patients with various medical conditions [12].
The issue of whether adult patients at risk for OSA should be identified prior to surgery remains unsolved at present. The identification of OSA risk factors, especially obesity, congestive heart failure and aging, should alert the anesthetists to the possibility of OSA existence, encouraging the use of STOP-BANG questionnaire. In a retrospective cohort study, conducted by Seet, et al. the demographic, medical and perioperative outcome data of 5,432 patients who underwent elective surgery were collected. Intraoperative and early postoperative complications were noted in 7.4% of the patients. The rate of those unexpected adverse events was higher among patients with STOP-BANG scores≥3 compared to those with a STOP-BANG score of 0. Patients with STOP-BANG scores≥5 had a fivefold increased risk of unexpected intraoperative and early postoperative adverse events. Thus, the STOP-BANG score may be used as a preoperative predictive tool for the risk of intraoperative and early postoperative complications [13].
The aim of the current study was to identify patients with OSA risk factors among patients who were about to undergo an elective surgery.
Methods
This was a retrospective study in which data were collected from files of patients who underwent elective surgery between January 2018 and March 2020, upon receiving the approval of the local ethical committee (Registration no. ASF-0057-20). The study was conducted in a regional general hospital, in which there was no mandatory guidelines to complete the STOP-BANG questionnaire pre-operatively. Hence, the anesthesiologists could choose to fill in the STOP-BANG questionnaire according to their discretion. The data included the age and gender of the patients, the type of surgical procedures they underwent, their comorbidities and the score of the STOP-BANG questionnaire, if answered by the anesthesiologists. The STOP-BANG questionnaire consists of eight yes-or-no questions based on the major risk factors for OSA by indicating symptom or physical attributes often associated with OSA (snoring, tiredness: observed apnea, high blood pressure, body mass index that is higher than 35 m/kg2, age over 50 years, neck circumference greater than 16 inches and gender. A STOP-BANG score of 2 or less is considered low risk, and a score of 5 or more is high risk for having either moderate or severe OSA [12]. The study included patients over the age of 50 years, who underwent elective orthopedic surgery, general surgery or laparoscopic aid surgery for various conditions. Patients with sleep apnea diagnosed before surgery were not included in the study.
Results
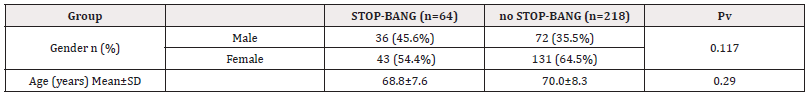
A total of 282 patients were included in this study. The STOP-BANG questionnaire was filled in before surgery for 64 patients (22.7%) (STOP-BANG group). Females were the majority (63.8%) of the patients in the group of patients in which STOP-BANG questionnaire was not filled before surgery (no STOP-BANG group, n=203). The ratio between males and females was almost the same, 45.3% vs. 54.7% respectively in the STOP-BANG group. There was also no significant difference in the patients' age between the two groups, 68.7±7.8 years in the STOP-BANG group and 70.0±8.2 years in the no STOP-BANG group (Table 1).
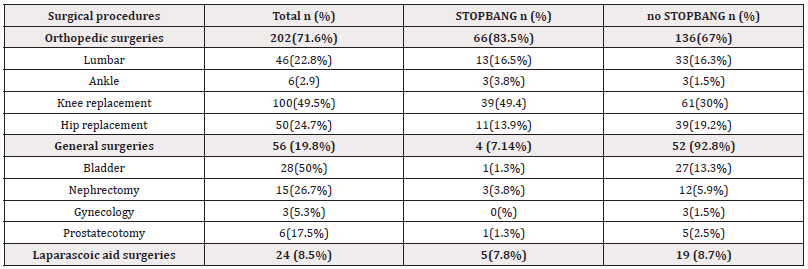
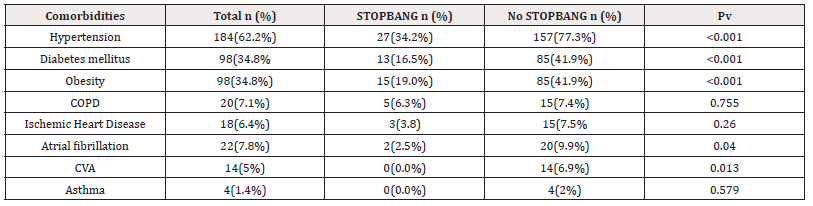
Overall, most of the patients underwent orthopedic operations (71.6%). This was also noted in the STOP-BANG group (85.9%) and in the no STOP-BANG group (67.4%) (Pv=0.006). The most common type of orthopedic surgery was a knee replacement (47.5% total, 51.6 % in the STOP-BANG group and 30.7% in the no STOP-BANG group (Table 2). The most common comorbidities in both groups were hypertension, obesity and diabetes mellitus (Table 3).
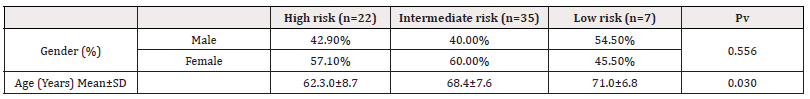
The data was then divided into 3 groups according to the degree of risk received from the STOP-BANG scores: Low risk (STOP-BANG score 0-2), Intermediate risk (STOP-BANG score 3-4) and High risk (STOP-BANG score 5-8). There was no significant difference between the number of males and females in all the groups (42.9% vs. 57.1% in the Low-risk group, 40.0% vs. 60.0% in the intermediate risk group and 54.5% vs. 45.5% in the High-risk group, respectively, Pv = 0.556). The patients in the high-risk group were significantly older than in the Low-risk group of patients (62.3±8.7 years of age in the Low-risk group vs. 71.0±6.8 years of age in the High-risk group, Pv=0.03) (Table 4a).
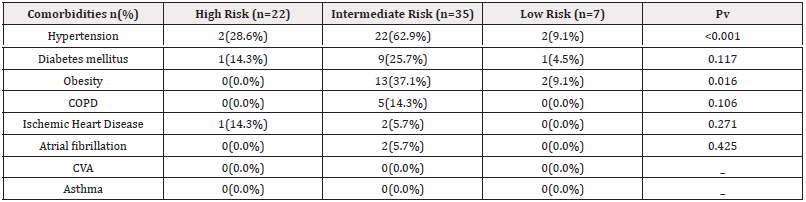
Hypertension and obesity were significantly the most common morbidities among the Intermediate risk group compared to the other two risk groups. Hypertension was present in 62.9% of the patients from the Intermediate risk group compared to 28.6% in the Low-risk group and 9.1% in the High-risk group (Pv<0.001). Obesity was reported in 37.1% of the patients from the Intermediate risk group compared to 0.0% in the Low-risk group and 9.1% in the High-risk group (Pv<0.001) (Table 4b).
Discussion
It is well established that the prevalence of OSA in the surgical population is high, between 3 and 17% depending on age and gender [14] with a great risk of peri– and intra-operative complications for those patients. Problems with intubation and extubating, hypnotics, opioids and muscle relaxants commonly used during general anesthesia, as well as body positioning are among the risk factors contributing to the development of anesthesia complications. Indeed, in 2018, the Society of Anesthesia and Sleep Medicine recommended that known or suspected OSA should be considered as a risk factor for difficult intubation, difficult mask ventilation, or a combination of both during anesthesia [15].
Therefore, it is necessary to identify the patients with OSA in order impotent precautions before and during the anesthesia process. For example, to extubate those patients while awake and able to respond to command, use of a local or regional instead of general anesthesia, as well as using lateral, upper body elevation or 30° reverse Trendelenburg position [16,17].
The most value finding of the current study was that patients who were about to undergo various elective operations presented a high rate of comorbid, such as hypertension, obesity and diabetes mellitus, which are the most common risk factors associated with OSA. The data also revealed that obesity and hypertension were the most common morbidities among the intermediate risk group of the STOP-BANG (score 3-4). These data suggest that patients who about to undergo surgery suffer from the same comorbidities were diagnosed among patients who were suspected to suffer from OSA, as was noted by the STOP-BANG questionnaire. 0Identifying those patients and taking preoperative precautions could prevent the complications due to the anesthesia process.
In the medical center in which the study was conducted there were no mandatory guidelines to complete the STOP-BANG questionnaire before the operation. This might explain the low percentage of STOP-BANG questionnaires completed (22.7%). It seems that although the clinical risk factors for OSA are present, the anesthesiologists rarely suspect patients might have OSA. Alternatively, the anesthesiologists are not aware of the existence of the STOP-BANG questionnaire, or of the risks underlying the anesthesia process for OSA patients.
The existence of a routine mandatory process to diagnose OSA prior to surgery is very rare. Moreover, most anesthesiologists have almost no knowledge regarding peri-operative care of OSA patients. In addition, there are few limited guidelines regarding the preoperative care of OSA patients [15]. An interesting survey was conducted by Erbaş, et al., who monitored the practice of anesthesiologists in the diagnosis of patients with OSA. While, 97% of 134 participants in the study thought that identifying patients with OSA was important, 43% did not know that the STOP-BANG questionnaire could be used as a clinical tool to trace the OSA patients. However, it is worth noting that 84% were aware of the fact that OSA patients might have difficulty with intubation and thus 35% chose inhalation anesthetics and 48% used total intravenous anesthesia [18]. In another study, a survey was conducted among Canadian anesthesiologists to evaluate their perspectives on the peri-operative management of patients with diagnosed or suspected OSA. About half of the participants pointed out the patients who may suffer from OSA just upon a clinical suspicion and not upon following any systematic screening. Many of them (47%) were not aware of the existence of any institutional policy to guide the peri-operative management of patients with OSA [19]. Bamgbade, et al. assessed the practice of the peri-operative care of OSA patients among 4100 anesthesiologists in the United Kingdom. Most of them rarely or only occasionally encountered OSA patients. OSA screening tests were ordered if the patients had tonsillar hypertrophy, head/neck tumor, BMI >35, increased neck circumference, craniofacial anomaly, and a right sided electrocardiography anomaly. Most of the anesthesiologists indeed encouraged a different anesthesia strategy for those patients, such as administering neuraxial anesthesia without sedation or ensuring patients' being awake, a semi sitting and normal breathing before extubation [10].
The necessity of identifying OSA patient’s peri-operatively was well demonstrated by a study conducted by Namen et, al. In this study, a protocol for an active intervention was developed. The intervention included identification of OSA patients’ status, alerting the peri-operative caregivers, and providing information about anesthesia adjustments (including the limiting of opioids and sedatives, changing body position, as well as enhanced monitoring). The success of the intervention was evaluated by the rate of medical emergency team activations. It was found that, compared with historical cases, a significant reduction in the numbers of medical emergency team activations was noted in the intervention group. Those incidences included rapid responses, reintubation, code blue and code strokes. Most of them were markedly observed in patients with risk and high risk for OSA [20].
Conclusion
The prevalence of OSA in surgical patients is increasing and is associated with an increased risk for various peri- and intra- operative complications due to the anesthesia process. There is extensive evidence that peri-operative management of those patients may limit the risk of potential complications. This includes early OSA diagnosis and risk evaluation, peri-operative therapy and an appropriate anesthetic regimen. The current study further demonstrated that risk factors for OSA exist in patients who are about to undergo surgical procedures. Nevertheless, many of the patients are not diagnosed and there is a lack of knowledge and clinical experience among anesthesiologists regarding the importance of peri-operative identification and care of OSA patients. Improving the anesthesiologists’ knowledge and optimization of peri-operative care of OSA patients is a critical target in keeping the safety and health of patients who are about to undergo elective surgery. In order to achieve this target, a mandatory requirement of peri-operative identification of OSA should be implemented in clinical institutions. In addition, strict and precise guidelines on how to manage the anesthetic procedure, pre, during and post-operation should be formulated. The current study has a few limitations. This was a retrospective study with a small sample of patients, encompassing and heterogeneous surgical types. Also, he STOP-BANG test was performed on a small sample.
Declarations
Ethics Approval and Consent to Participate
This study was permitted by the Clinical Research Ethics Committee of Shamir Medica Center, Israel (ASF-0057-20). Due to the non-interventional study design, the Institutional Review Board of The Shamir medica center waived the need for written informed consent from participants.
Consent for Publication
Not applicable
Availability of Data and Materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Competing Interests
We declare that we have no conflicts of interest to this work.
Funding
Not applicable.
Authors’ Contributions
IP, GI, AH, and ZHBZ were responsible for designed this study and collected the data. AH and BYS was responsible for study execution and manuscript writing. ZHBZ and IP revised it critically. All authors have read and approved the final version of the manuscript.
Competing Interests
We declare that we have no conflicts of interest to this work.
References
- Singh M, Liao P, Kobah S, et al. (2013) Proportion of surgical patients with undiagnosed obstructive sleep apnoea. Br J Anaesth. 110(4): 629-636.
- Devaraj U, Rajagopala S, Kumar A, et al. (2017) Undiagnosed obstructive sleep apnea and postoperative outcomes: a prospective observational study. Respiration 94(1): 18-25.
- Weingarten TN, Sprung J (2022) Perioperative considerations for adult patients with obstructive sleep apnea. Curr Opin Anaesthesiol 35(3): 392-400.
- Jordan AS, Odonoghue FJ, Cori JM, Trinder J (2017) Physiology of Arousal in Obstructive Sleep Apnea and Potential Impacts for Sedative Treatment. Am J Respir Crit Care Med 196(7): 814-821.
- Parati G, Lombardi C, Castagna F, et al. (2016) Heart failure and sleep disorders. Nat Rev Cardiol 13(7): 389-403.
- Nagappa M, Wong DT, Cozowicz C, et al. (2018) Is obstructive sleep apnea associated with difficult airway? Evidence from a systematic review and meta-analysis of prospective and retrospective cohort studies. PLoS One 13(10): e0204904.
- Baluch A, Mahbubani S, Al-Fadhli F, Kaye AD, Frost EAM (2009) Anesthetic care of the patient with obstructive sleep apnea. Middle East J Anaesthesiol. 20(2):143-152.
- Liu SS, Chisholm MF, Ngeow J, et al. (2011) Postoperative hypoxemia in orthopedic patients with obstructive sleep apnea. HSS J 7(1): 2-8.
- Ehsan Z, Mahmoud M, Shott SA, Amin RS, Ishman SL (2016) The effects of anesthesia and opioids on the upper airway: A systematic review. Laryngoscope 126(1): 270-284.
- Bamgbade OA, Oluwole O, Khalaf WM, Namata C, Metekia LM (2021) Perioperative care of obstructive sleep apnea patients: A survey of European anesthesiologists. Saudi J Anaesth 15(2): 101-108.
- Heinzer R, Vat S, Marques-Vidal P, et al. (2015) Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 3(4): 310-318.
- Chung F, Memtsoudis SG, Ramachandran SK, et al. (2016) Society of Anesthesia and Sleep Medicine Guidelines on Preoperative Screening and Assessment of Adult Patients with Obstructive Sleep Apnea. Anesth Analg 123(2): 452-473.
- Seet E, Chua M, Liaw CM (2015) High STOP-BANG questionnaire scores predict intraoperative and early postoperative adverse events. Singapore Med J 56(4): 212-216.
- Peppard PE, Young T, Barnet JH, et al. (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177(9): 1006-1014.
- Memtsoudis SG, Cozowicz C, Nagappa M, et al. (2018) Society of Anesthesia and Sleep Medicine Guideline on Intraoperative Management of Adult Patients with Obstructive Sleep Apnea. Anesth Analg 127(4): 967-987.
- Cozowicz C, Memtsoudis SG (2021) Perioperative Management of the Patient with Obstructive Sleep Apnea: A Narrative Review. Anesth Analg 132(5): 1231-1243.
- Corso RM, Gregoretti C, Braghiroli A, Fanfulla F, Insalaco G (2014) Practice Guidelines for the Perioperative Management of Patients with Obstructive Sleep Apnea: navigating through uncertainty. Anesthesiology 121(3): 664-665.
- Erbaş M, Kiraz HA, Şimşek T, et al. (2015) Turkish Anaesthesiologist's Experiences of Anaesthetic Management of Patients with Obstructive Sleep Apnea (OSA). Turk J Anaesthesiol Reanim 43(4): 253-262.
- Cordovani L, Chung F, Germain G, et al. (2016) Perioperative management of patients with obstructive sleep apnea: a survey of Canadian anesthesiologists. Can J Anaesth 63(1): 16-23.
- Namen AM, Forest D, Saha AK, et al. (2022) Reduction in medical emergency team activation among postoperative surgical patients at risk for undiagnosed obstructive sleep apnea. J Clin Sleep Med 18(8): 1953-1965.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.