Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Prevalence of Vitamin D Deficiency in Type 2 Diabetic Patients with And without Foot Ulcer
*Corresponding author: Uzair Akbar Ali, University Hospital Waterford, Ireland.
Received: April 29, 2024; Published: May 08, 2024
DOI: 10.34297/AJBSR.2024.22.002965
Abstract
Background: Vitamin D, in addition to its role in calcium homeostasis, also functions to activate innate immunity and accelerates the healing process. About one billion people across the world are either deficient or insufficient in vitamin D. Studies have reported that vitamin D deficiency is a risk factor for developing diabetes.
Objective: The study aims to evaluate the relationship between vitamin D levels and the presence of foot ulcers in type 2 diabetic patients.
Methods: The convenience sample method was used in this pilot cross-sectional study to recruit adult patients with type 2 diabetes, both with and without diabetic foot ulcers. Vitamin D levels in all subjects were measured prospectively during data collection.
Results: A study of 156 participants (63.5% males, 36.5% females) with an average age of 72.31 years and an average diabetes duration of 10.98 years found a statistically significant difference in mean vitamin D levels between those with foot ulcers (34.73 nmol/L) and those without (43.81 nmol/L) (p < 0.027). The average vitamin D level for the sample was 39.27 nmol/L (95% CI 35.2 - 43.3, p < 0.001).
Conclusion: The study highlights the high prevalence of vitamin D deficiency among individuals with type 2 diabetes, particularly those with diabetic foot ulcers. It suggests a correlation between lower vitamin D levels and foot ulcers, suggesting the importance of vitamin D in managing diabetic complications. Further research is needed to understand its therapeutic benefits.
Keywords: Vitamin D, Diabetic foot ulcers, Type 2 Diabetes, Calcium homeostasis
Introduction
The global prevalence of diabetes has surged over the years, affecting around 422 million adults in 2014, up from 108 million in 1980. Obesity is one of several causes contributing to the global doubling of diabetes cases since 1980 [1]. Diabetes prevalence has increased significantly in the Irish population, according to a meta-analysis and systematic review conducted between 1998 and 2015. During this time, the prevalence rose significantly, from 2.2% in 1998 to 5.2% in 2015. Complication rates also rose, with retinal going from 6.5% to 25.2%, neuropathy from 3.2% to 32%, and nephropathy from 2.5% to 5.2% [2]. According to the International Diabetes Federation Atlas (2013), by 2030, the adult population aged 20 to 79 years would have an estimated 278,850 diabetes cases [3]. Diabetes prevalence has risen as a result of improved screening procedures, increasing awareness, and population expansion. Type 2 diabetes, which affects 90-95% of diabetics, is the world's seventh greatest cause of mortality. The World Health Organization defines diabetic foot disease as "foot ulceration associated with neuropathy and varying degrees of ischemia and infection."[4]. Approximately 15% of individuals with type 2 diabetes mellitus will have lower extremities problems throughout their lifetime [5]. The global annual incidence of diabetic foot ulceration among diabetics is 6.3% [6]. Individuals with diabetic foot illness have a 2.5-fold increased risk of mortality within five years than those without [7]. More than 50% of diabetic foot ulcer patients experience an infection, and 20% of those with moderate to severe diabetic foot ulcers require some kind of amputation. This situation contributes to mortality rates that for all diabetic patients surpassing 70% within five years, and for those receiving renal replacement treatment, they approach 74% after two years. [8]. Diabetic foot ulceration not only increases death rates among diabetics, but it also places a huge financial strain on healthcare systems. Diabetic foot issues are frequently more expensive to treat than common malignancies [9]. The CODEIRE study, which was conducted in Ireland, evaluated the direct healthcare expenses associated with controlling type 2 diabetes. The data found that diabetes-related charges consumed 10% of the national health budget, with hospitalization for complications accounting for 49% of that spending [10]. Given that these problems are frequently avoidable, prioritizing illness prevention and related complications would be a cost-effective strategy. Diabetic foot disease not only jeopardizes physical health but also reduces overall quality of life. According to Sana A AlSadrah's research, people with type 2 diabetes mellitus who have foot illness have not only physical morbidities but also mental health repercussions [11].
Vitamin D is available in two forms, namely vitamin D2 (ergocalciferol) and vitamin D3. Vitamin D deficiency can develop when sources are insufficient or unavailable. Vitamin D, when received by diet, is absorbed in the small intestine together with fats and other fat-soluble vitamins. Furthermore, exposure to the sun's UV rays allows for the non-enzymatic production of vitamin D3, which enters the bloodstream [12]. Vitamin D2 and D3 are both physiologically inactive unless they are activated and metabolized in two steps. The liver and kidneys convert vitamin D into its active form. Individuals with liver and renal abnormalities, such as diabetes, are particularly vulnerable to vitamin D insufficiency because vitamin D is not properly activated for biological function. The active form of vitamin D is known as 1,25-dihydroxycalcitriol. Measuring vitamin D levels (25 hydroxyvitamin D) is the most accurate way to assess an individual's vitamin D status. Vitamin D levels are regarded ideal between 30-80 ng/ml, whereas values between 21-29 ng/ml are defined as vitamin D insufficiency and levels below 20 ng/ml as vitamin D deficiency [13]. In addition to the variables listed above, the Western diet is often lacking in vitamin D-rich foods, making the Western population more susceptible to vitamin D deficiency [14,15]. A study of elderly Irish adults (aged 50-98) found that the prevalence of vitamin D insufficiency was 13.1%. Furthermore, the study discovered that the frequency of vitamin D deficiency was higher among smokers, obese adults, and physically inactive people [16].
Zehra Ozfirat stated in her review study that there is strong epidemiological evidence that vitamin D insufficiency has a role in the development of type 2 diabetes [17]. However, a thorough examination of the available literature on the relationship between vitamin D level and diabetic foot disease reveals a dearth of major study in this area, highlighting the need for future exploration. Nonetheless, a thorough evaluation of the literature suggests a link between vitamin D insufficiency and diabetic foot problems, as well as infection. It also implies that vitamin D supplementation may be beneficial in diabetic foot condition, while no precise dosage is indicated [18]. While the majorities of studies suggest association between vitamin D deficiency to diabetic foot disease, one study found that patients with foot ulcers had higher vitamin D levels [19]. More large-scale randomized controlled trials are required to determine a definitive association. A recent systematic review and meta-analysis of seven publications and 1,115 patients found that those with diabetic foot disease had considerably lower vitamin D levels than those without foot ulcers. According to this investigation, there is a significant risk of developing diabetic foot disease due to vitamin D insufficiency. It also implies that vitamin D supplementation might be a beneficial therapeutic choice for people who have both diabetes and ulcers on their feet [20]. It is imperative to recognize the limitations of this research, such as the relatively small sample sizes and the incorporation of both prospective and retrospective cohort studies.
This study investigates the relationship between diabetic foot ulcers, a serious diabetes-related condition, and vitamin D insufficiency. It seeks to comprehend the function of vitamin D in the onset and evolution of ulcers, with the goal of maybe discovering vitamin D supplementation as a viable therapeutic option for individuals with diabetic foot ulcers.
Methods
A convenience sample of 156 adult patients with type 2 diabetes seeking diabetic, vascular, and podiatry treatments at Waterford University Hospital participated in this prospective cross-sectional study. The purpose of the study was to look into whether type 2 diabetic patients had foot ulcers. Individuals were chosen one after the other until the target sample size was reached. T Yamane's method was used to compute the sample size, which was then accompanied by an 8% margin of error. Exclusion criteria included patients with end-stage renal or hepatic disease, type 1 diabetes, gestational diabetes, and those who had used calcium or vitamin D supplements during the previous six months. The single-blind trial was carried out between June and August of 2020. Patients in Group 1 had both type 2 diabetes and foot ulcers, while patients in Group 2 had type 2 diabetes but no foot ulcers. Wegner's categorization was used to examine diabetic foot ulcers in each group, which had 78 participants. An open wound or sore that usually develops on the sole of the foot in diabetics is referred to as a diabetic foot ulcer.
Demographic information, such as a history of diabetes and cigarette smoking, was obtained. The BMI was computed by dividing weight in kilos by height in meters squared. Glycated hemoglobin (HbA1c) levels were determined in non-fasting venous blood samples using dipotassium or tripotassium ethylenediaminetetraacetic acid (K2EDTA or K3EDTA) tubes. The cation exchange procedure was carried out utilizing a Tosoh G8 HPLC Analyzer. The findings were published in units of the International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) [21,22]. Serum 25-(OH) D3 levels were measured using an immunoassay on a Cobas 602 Roche analyzer utilizing the electrochemiluminescence (ECLIA) method. The concentrations were measured in nmol/L D. The IOM standards classified deficiency, inadequacy, and adequacy as <30 nmol/L, 30-50 nmol/L, and >50 nmol/L. The Glomerular Filtration Rate (GFR) was determined using the shortened Modification of Diet in Renal Disease (MDRD) equation. Non-fasting plasma samples were evaluated for calcium and phosphate levels using Roche Diagnostics' Cobas 8000 modular analyzer series (USA) [23].
The principal investigator placed the obtained data into a Microsoft Office Excel datasheet. The Statistical Processing for The Social Sciences (SPSS) program for Windows, version 23, was used for data coding and analysis. The analysis included figuring out the average vitamin D levels in each group of research participants. An independent student's t-test was used, with a significance level set at p < 0.05, to compare the means of vitamin D levels between the two groups and compare them with the mean values reported in the TILDA data. For categorical variables, percentages and frequencies were computed. The University Hospital Waterford Research Ethics Committee granted ethical permission for the project.
Results
The study enrolled 156 patients, with 99 (63.5%) males and 57 (36.5%) females. The individuals' average age was 72.31 years (95% CI 70.5-74.1), and the average duration of diabetes was 10.98 years (95% CI 9.91-12.1). Notably, the elderly patients (>80 years old) had the largest proportion of vitamin D insufficiency. Table 1 shows the demographic characteristics of the study participants, as well as their average vitamin D levels.
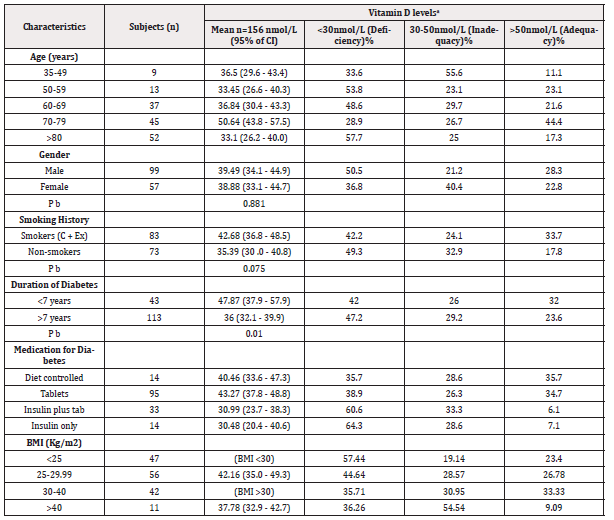
Table 1: Characteristics of study participants and mean plasma 25 (OH) D concentrations (nmol/L). aCutoffs based on the IOM guidelinees34. bp value after applying independent sample t-test
Note*: BMI is categorized as 25-29.9 (overweight), 30-40 (obesity), and >40 (morbid obesity).
The majority of the participants (n=95, 60.9%) were treated with oral hypoglycemic medications, whereas 33 (21.15%) used a combination of oral hypoglycemic drugs and insulin regimens. In terms of body mass index (BMI), 26.92% of the participants (n=42) were obese, and 11 people (7.05%) had morbid obesity, defined as a BMI more than 40. In addition, 21 patients (31.6%) were current smokers, while 62 individuals (39.74%) were former smokers. Mean vitamin D levels did not differ significantly between smokers (42.68 nmol/L, 95% CI 36.8 - 48.5) and non-smokers (35.39 nmol/L, 95% CI 30 - 40.8) (p < 0.75).
The study discovered that 45.5% of the patients (n=71) had vitamin D deficiency and 28.20% (n=44) had vitamin D insufficiency. There was no significant difference in mean vitamin D levels between males and females (p <0.607). Type 2 diabetes patients with foot ulcers exhibited a higher frequency of vitamin D insufficiency than those without foot ulcers (p < 0.027). This suggests that persons with diabetic foot ulcers are more likely to have lower vitamin D levels, establishing a link between vitamin D insufficiency and the incidence of foot ulcers in type 2 diabetes (Figure 1).
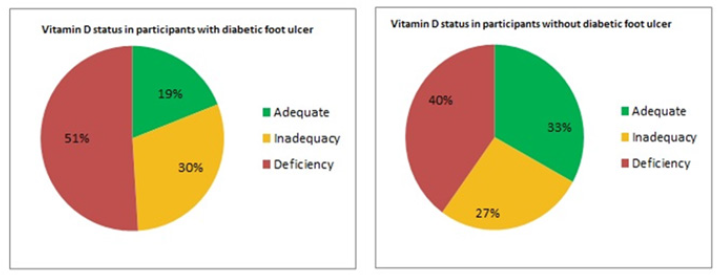
Figure 1: Prevalence of vitamin D deficiency and inadequacy in type 2 diabetic patients with and without diabetic foot ulcers (Group 1 and 2 patients).
Among the patients in Group 1, the majority (58.97%) had grade 1 ulcers (n=46), whereas 30.77% had grade 3 ulcers. Only one patient was diagnosed with partial foot gangrene (grade 4). Among these patients, 19 had undergone amputations, with 10 having amputations during the research period and 9 having previous procedures. There was no significant correlation detected between the severity of foot ulceration and mean vitamin D levels (p<0.66). This implies that the severity of foot ulcers in type 2 diabetic patients may not be directly connected to their vitamin D levels.
The study population had an average estimated glomerular filtration rate (eGFR) of 47.69 ml/min/1.73 m² (95% CI 45.3-50). The study eliminated 20 patients with a GFR of less than 15 ml/min/1.73 m². Patients with a GFR of 15-30 ml/min/1.73m² had significantly lower vitamin D levels, with an average of 30.11 nmol/L (95% CI 22.5-37.7, p < 0.019). The sample population's mean calcium and phosphate levels were 2.36 mmol/L (95% CI 2.34-2.38), and 1.86 mmol/L (95% CI 0.34-3.38). The average glycated hemoglobin (HbA1c) level in the included patients (n=156) was 58.69 mmol/mol (95% CI 55.8-61.5). There was no significant difference in mean vitamin D levels between individuals with HbA1c greater than 60 mmol/mol and those with HbA1c less than 60 mmol/mol (p < 0.73).
Discussion
Diabetics with foot ulcers have lower vitamin D levels, a higher frequency of vitamin D deficiency, and more severe vitamin D deficit compared to non-ulcerated diabetic patients [24]. In our study, 45.5% (n=71) of the patients showed vitamin D insufficiency, while 28.20% (n=44) did not have enough vitamin D. These figures imply that a significant number of people with type 2 diabetes have poor vitamin D levels. This is much higher than the prevalence reported in a prior study on older Irish persons, which found a deficiency prevalence of 13.1% (95% CI 12.1-14.2) and an inadequacy prevalence of 29.4% (95% CI 27.8-30.8) over all months. These findings highlight the increased sensitivity of people with type 2 diabetes to vitamin D deficiency, emphasizing the importance of focused therapies and monitoring to improve their vitamin D status (Table 2).
The study excluding patients taking vitamin D or calcium supplements may introduce confounding factors, such as increased awareness of health, healthier dietary habits, and higher social stratum. These factors may contribute to higher vitamin D levels and potentially impact the association between vitamin D deficiency and diabetic foot ulcers. Future research should consider these potential confounding factors to gain a clearer understanding of the relationship between vitamin D levels, supplementation, and the development of diabetic foot ulcers. Previous studies have found that individuals with diabetic foot ulcers have significantly lower vitamin D levels and a higher number of VDD individuals compared to those without DFUs. High-dose vitamin D has been shown to promote healing in chronic diabetic foot ulcers, and severe deficiency of vitamin D may increase the risk of diabetic foot infections [18,20,25,26].
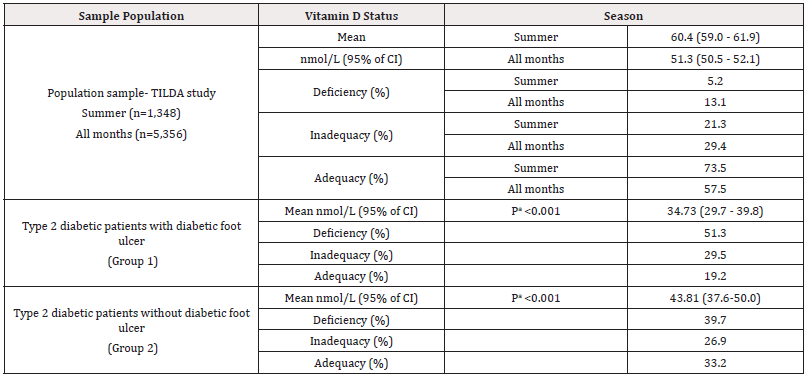
Table 2: Comparison of prevalence of vitamin D deficiency and inadequacy in the study population with a study based on data taken from TILDA study36 in Ireland. a denotes independent sample t-test used
The study of diabetic foot ulcers highlights the importance of considering other potential confounders such as body mass index (BMI), gender, and glycated haemoglobin (HbA1c) in the development of ulcers. These variables can potentially confound the association between vitamin D levels and ulcer presence. Studies have shown that BMI can mediate the effects of dietary types on type 2 diabetes mellitus, HbA1c and pregnancy outcomes, socioeconomic status impacts chronic diabetes control, obesity and HbA1c levels, and trends of HbA1c and BMI in people with type 2 diabetes. These studies highlight the multifaceted nature of diabetic foot ulcers and the need to account for various confounding factors [27,28,29,30].
Numerous variables can have a substantial impact on the outcomes, with climate and geographic location being key factors. Tropical countries, which have prolonged and severe solar exposure, differ significantly from European climates, influencing the outcomes. Notably, the study was done against the backdrop of the Covid-19 pandemic, which presented unique problems. Quarantine procedures, restrictions on outside activities, and the cocooning phenomena surfaced as key factors, limiting the study's scope. Expanding on this topic, it is critical to go deeper into these limits and explain their consequences for the research findings. Examining these intricacies through a sophisticated perspective can yield a more thorough and nuanced knowledge, improving the larger scholarly conversation.
A p-value of less than 0.05 shows a higher frequency of vitamin D deficiency among type 2 diabetic individuals with diabetic foot ulcers than those without ulcers (refer to Table 2). Interestingly, the study found no significant association (p < 0.667) between ulcer disease severity and vitamin D levels among the group. Future studies involving correlation statistics with a bigger sample size are needed to shed additional light on this issue. More extensive research in this area will provide a more comprehensive understanding of the association between vitamin D insufficiency and the prevalence of diabetic foot ulcers, perhaps leading to important advances in diabetes care.
The study's findings revealed a significant incidence of vitamin D shortage and inadequacy in the sample population, with greater rates reported among type 2 diabetic individuals with diabetic foot ulcers. Despite these important findings, more research is needed to understand the complex link between vitamin D levels and the genesis and severity of diabetic foot infections. Furthermore, the prospective benefits of vitamin D administration in diabetic foot ulcer patients are unknown, necessitating additional research to fully understand its therapeutic potential. By addressing these knowledge gaps through rigorous research efforts, we can expand our understanding of the role of vitamin D in diabetic foot care and perhaps improve clinical outcomes for affected patients.
The study has limitations, including convenience sampling, small sample size, single-center design, and lack of a control group without diabetes or foot ulcers. The cross-sectional design and lack of detailed information on potential confounding factors like sun exposure, dietary habits, and comorbidities also hinder causality and temporal relationships. The assessment of foot ulcer severity using Wegner's classification may not fully capture the range of ulcer severity, potentially limiting the accuracy of the results. Additionally, the study did not collect information on vitamin D supplementation, which may be a significant confounding factor in the association between vitamin D levels and diabetic foot ulcers. Future studies with larger sample sizes, control groups, longitudinal designs, and comprehensive data collection are needed.
Conclusion
In conclusion, this study reveals a high prevalence of vitamin D deficiency and inadequacy among individuals with type 2 diabetes, particularly those with diabetic foot ulcers. Lower vitamin D levels are linked to foot ulcers in this population. However, the study's limitations include a cross-sectional design, small sample size, and convenience sampling method. Larger, controlled studies with longitudinal designs are needed to investigate the relationship between vitamin D levels and diabetic foot ulcers. The study emphasizes the importance of assessing and addressing vitamin D status in individuals with type 2 diabetes and the need for further research to explore the therapeutic benefits of vitamin D supplementation in managing diabetic foot ulcers.
Conflict of Interest Declaration
There are no conflicts of interest to declare.
Acknowledgments
None.
References
- World Health Organization. World Health Statistics 2016 [OP]: Monitoring Health for the Sustainable Development Goals (SDGs). World Health Organization.
- Tracey ML, Gilmartin M, O Neill K, Fitzgerald AP, McHugh SM, et al. (2015) Epidemiology of diabetes and complications among adults in the Republic of Ireland 1998-2015: a systematic review and meta-analysis. BMC public health 16:132.
- Federation ID, Atlas ID (2013) International diabetes federation. IDF diabetes atlas, 6th edn Brussels, Belgium: International Diabetes Federation.
- Tuttolomondo A, Maida C, Pinto A (2015) Diabetic foot syndrome: Immune-inflammatory features as possible cardiovascular markers in diabetes. World J Orthop 6(1): 62-76.
- Reiber GE, Boyko EJ, Smith DG (1995) Lower extremity foot ulcers and amputations in diabetes. Diabet Amer 2: 409-427.
- Zhang P, Lu J, Jing Y, Tang S, Zhu D, et al. (2017) Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Ann Med 49(2): 106-116.
- Walsh JW, Hoffstad OJ, Sullivan MO, Margolis DJ (2016) Association of diabetic foot ulcer and death in a population‐based cohort from the United Kingdom. Diabet Med 33(11): 1493-1498.
- Armstrong DG, Boulton AJ, Bus SA (2017) Diabetic foot ulcers and their recurrence. N Engl J Med 376(24): 2367-2375.
- Barshes NR, Sigireddi M, Wrobel JS, Mahankali A, Robbins JM, et al. (2013) The system of care for the diabetic foot: objectives, outcomes, and opportunities. Diabet Foot Ankle 10: 21847.
- Nolan JJ, O Halloran D, McKenna TJ, Firth R, Redmond S (2006) The cost of treating type 2 diabetes (CODEIRE). Ir Medi J 99(10): 307-310.
- AlSadrah SA (2019) Impaired quality of life and diabetic foot disease in Saudi patients with type 2 diabetes: A cross-sectional analysis. SAGE Open Med 7: 2050312119832092.
- DeLuca HF (2004) Overview of general physiologic features and functions of vitamin D. Am J Clin Nutr 80(6): 1689S-1696S.
- Hollis BW, Wagner CL (2005) Normal serum vitamin D levels. N Engl J Med 352(5): 515-516.
- Sullivan F, Laird E, Kelly D, van Geffen J, van Weele M, et al. (2017) Ambient UVB dose and sun enjoyment are important predictors of vitamin D status in an older population. J Nutr 147(5): 858-868.
- Holick MF (2006) High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc 81(3): 353-373.
- Laird E, O Halloran AM, Carey D, Healy M, O Connor D, et al. (2018) The prevalence of vitamin D deficiency and the determinants of 25 (OH) D concentration in older Irish adults: data from The Irish Longitudinal Study on Ageing (TILDA). J Gerontol A Bio Sci Med Sci 73(4): 519-525.
- Ozfirat Z, Chowdhury TA (2010) Vitamin D deficiency and type 2 diabetes. Postgrad Med J 86(1011): 18-25.
- Macido A (2018) Diabetic foot ulcers and vitamin D status: a literature review. SAGE Open Nurs 4: 2377960818789027.
- Afarideh M, Ghanbari P, Noshad S, Ghajar A, Nakhjavani M, et al. (2016) Raised serum 25-hydroxyvitamin D levels in patients with active diabetic foot ulcers. Br J Nutr 115(11): 1938-1946.
- Dai J, Jiang C, Chen H, Chai Y (2019) Vitamin D and diabetic foot ulcer: a systematic review and meta-analysis. Nutr Diabetes 9(1): 8.
- Alvin M, Lundin F. A comparative study of Tosoh G11 and Bio-Rad D-100 analyzers for HbA1c analysis.
- Geistanger, A., Arends, S., Berding, C., Hoshino, T., Jeppsson, J.O., et al. and IFCC Working Group on Standardization of Hemoglobin A1c (2008) Statistical methods for monitoring the relationship between the IFCC reference measurement procedure for hemoglobin A1c and the designated comparison methods in the United States, Japan, and Sweden. Clin Chem 54(8): 1379-1385.
- Del Valle HB, Yaktine AL, Taylor CL, Ross AC. Dietary reference intakes for calcium and vitamin D.
- Lin J, Mo X, Yang Y, Tang C, Chen J (2023) Association between vitamin D deficiency and diabetic foot ulcer wound in diabetic subjects: A meta‐analysis. Int Wound J 20(1): 55-62.
- Li X, Kou S, Chen G, Zhao B, Xue J, et al. (2023) The relationship between vitamin D deficiency and diabetic foot ulcer: A meta‐analysis. Int Wound J 20(8): 3015-3022.
- Halschou-Jensen PM, Sauer J, Bouchelouche P, Fabrin J, Brorson S, et al. (2023) Improved healing of diabetic foot ulcers after high-dose vitamin D: a randomized double-blinded clinical trial. Int J Low Extrem Wounds 22(3): 466-474.
- Wang S, Wen J, Miao D, Sun Z, Li D, et al. (2023) Mediating effect of BMI on the relation of dietary patterns and glycemic control inT2DM patients: results from China community-based cross-sectional study. BMC Public Health 23(1): 468.
- Hara K, Hirase T, Pathadka S, Cai Z, Sato M, et al. (2024) Trends of HbA1c and BMI in People with Type 2 Diabetes: A Japanese Claims-Based Study. Diabetes Ther 4: 801-817.
- Sebastian-Valles F, Martínez-Alfonso J, Arranz Martin JA, Jiménez-Díaz J, Hernando Alday I, et al. (2024) Impact of socioeconomic status on chronic control and complications of type 1 diabetes mellitus in users of glucose flash systems: a follow-up study. BMC Med 22(1): 37.
- Noor N, Akturk HK, Desimone M, Basina M, Rioles N, et al. (2022) The effect of obesity on HbA1c among adults with type 1 diabetes: a US based multicenter study. Diabet 71(Supplement_1).



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.