Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Surgical Treatment for High-Grade Spondylolisthesis in Adolescents and Young Adults - A Safe and Reliable Option
*Corresponding author: Jorge Mineiro, Spine Surgeon, Hospital CUF Descobertas, Head of Department, Department of Orthopaedics and Traumatology, Spinal Unit Lisbon, Portugal.
Received: June 03, 2024; Published: June 07, 2024
DOI: 10.34297/AJBSR.2024.22.003010
Abstract
Conservative treatment of High-Grade Spondylolisthesis in adolescents and young adults is prone to fail according to the literature and there are still many questions to be answered regarding what is the best technic and is it necessary to include L4L5 in the fusion at the index procedure. This retrospective study was designed to assess the outcome of ten consecutive patients diagnosed with HGS and operated on over a period of 8 years, submitted to surgical treatment between 2013 and 2021 by the same spine team. All patients underwent posterior decompression and fusion using the Spinal Deformity Study Group classification and guidelines for treatment. The mean follow-up was 4,3 years and patients were assessed clinically and radiologically. All patients showed signs of radiological fusion and remain asymptomatic clinically. Posterior only approach with circumferential instrumented L5S1 fusion with autologous bone graft and a transdiscal L5-S1 screw is a safe and reliable option for the treatment of HGS in this age group, preserving the L4L5 disc and achieving good clinical and radiologic outcomes.
Keywords: High grade spondylolisthesis in adolescents and young adults, Surgical treatment, Lumbar-sacral deformity
Introduction
Herbiniaux first described spondylolisthesis in 1782; this term derives from the combination of spondylos - spine - and olisthesis - slippage and refers to the anterior displacement of a vertebra on its next caudal vertebra [1]. Based on Newman’s work it was Wiltse [2] who proposed the physiopathology classification most used nowadays - Type I dysplastic; type II isthmic spondylolisthesis; type III degenerative; type IV traumatic; type V pathologic; type VI iatrogenic. Meyerding’s classification [3] categorizes the amount of sagittal slippage in 5 grades (I 0-25%, II 25-50%, III 50-75%, IV 75-100%, and V is spondyloptosis) - the term High-Grade Spondylolisthesis (HGS) refers to a slippage over 50% (1% of spondylolisthesis patients). [4] The highest rate of spondylolisthesis slippage is found in Wiltse’s type I (incidence of 32%), hence most of the HGS cases are dysplastic. Spondylolisthesis is one of the most frequent causes of lumbar pain in adolescents (sensitivity of 81% and specificity of 39.7%) [5,6]. In HGS significant changes in sagittal balance may occur - patients might present with kyphotic deformity and compensatory mechanisms above (lordosis increase in the remaining lumbar levels) and below (pelvic retroversion, flexion of the hips and knees) [7].
Non-surgical treatment will suffice in the majority of spondylolisthesis cases, [8] but in high-grade patients there’s a higher tendency to progression, it may present earlier in childhood, and is more commonly associated with neurologic impairment due to the compression of the nerve roots by the intact elongated pars - therefore is most likely to be treated with surgery [9] There are many different procedures proposed for the treatment of HGS patients, but still no consensus in the literature. This paper aims to review the results of the HGS patients surgically treated at our institution and try to define the rationale behind the choice of the surgical procedure.
Methods
The study design was a retrospective evaluation of systematically followed-up patients, analyzing both clinical and image results, done by the same author using validated software, conducted during 2022 and 2023. Ten consecutive patients diagnosed with HGS, submitted to surgical treatment between 2013 and 2021 by the same spine team were enrolled in the study. Patients with previous surgery, other musculoskeletal conditions, or lower extremity abnormalities were excluded. Preoperative and postoperative clinical data were collected from the medical records; lumbar pain, irradiated pain, neurologic deficits, posture, and gait abnormalities were registered. Standard standing posterior-anterior and lateral radiographs of the spine were obtained preoperatively and during the follow-up period. Lumbopelvic parameters were obtained - pelvic incidence (angle between a line connecting the center of the upper endplate of S1 to the center of the femoral heads and a line perpendicular to the endplate of S1), sacral slope (angle between a horizontal reference line and the endplate of S1) and pelvic tilt (angle between a vertical line and a line connecting the center of the upper endplate of S1 to the center of the femoral heads). Slip magnitude was classified according to Meyerding’s3; Slip Angle was defined as the angle subtended by the S1 endplate and the inferior endplate of L5 [10]; SDSG Classification of HGS [11] was applied to every case. Besides clinical improvement, fusion achievement was also a major outcome - it was defined as the radiological maintenance of the correction throughout follow-up time.
Results
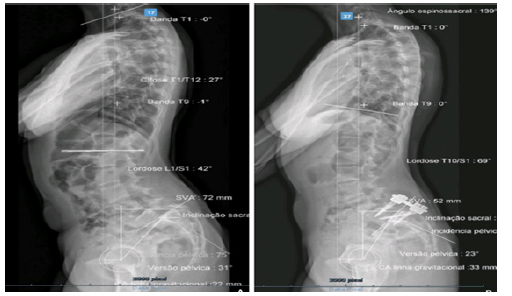
Ten patients, nine females, all diagnosed with high grade L5-S1 spondylolisthesis, with an average age of 19,70 ± 3,10 years old (60% between 13 and 17years old) at the time of surgery. Lumbar pain was the main symptom and present in all cases, and half also complained of irradiated pain; there were no cases of gait abnormalities nor neurologic deficit. Pre-operatively 3 patients were Meyerding’s grade III and 7 patients were Meyerding’s IV; no spondyloptosis case was included. According to SDGS’s classification, 2 patients were grade IV, 5 patients were grade V, and 3 were grade VI. The mean slip angle was 24,90° ± 5,12. Pelvic Incidence had a mean value of 74,80 ± 2,82, sacral slope 44,50 ± 2,75, pelvic tilt 29,20 ± 2,53 and lumbar lordosis 59 ± 15,27.
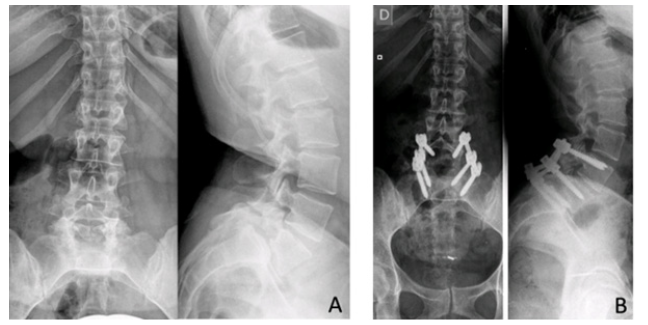
All patients were operated on by the same surgical team and submitted to a single-stage posterior-only approach. The prone positioning on the surgical table with hyperextended hips allows some reduction of the translation and the slip angle. Decompression by L5 laminectomy was performed in all cases - this gesture enables the adequate visualization and protection of L5 nerve roots during the reduction maneuver (the most commonly injured) and allows the harvesting of autologous bone graft to promote the interbody fusion. L5S1 discectomy was performed, and in highly dysplastic cases, an S1 dome osteotomy was also performed to allow better disk access and ease the reduction. Pedicular screws placed on S1 and L5 (and in some cases L4) enable the reduction process, end-plate preparation, the interposition of the autologous bone graft, and posterior lordotic compression. Four cases were instrumented with bilateral pedicular screws (three cases L4-L5-S1 and one monosegmental L5-S1). In the latter 6 cases, the surgical technique was improved - the reduction was performed with a unilateral screw in S1, which was temporarily fixed with a unilateral rod with posterior lordotic compression; then a pedicular entry-point was drilled in S1, but with a trajectory oriented upwards and medially, to transfix the S1L5 disk space and gain tricortical fixation (Figure 1). As the final step of definitive fixation, bilateral rods were placed. The procedure was performed under intra-operative neurophysiologic monitoring. No cast immobilization or orthosis was used in the post-operative period.
Post-operatively significant imaging improvement was observed - only one patient remained with a high-grade spondylolisthesis (but improved from Meyerding’s IV to III and reduced the slip angle in 20°), five achieved grade I and four achieved grade II. The mean slip angle was improved by 18,20° (p 0,005) resulting in an average follow-up absolute value of 6,70° ± 1,995; sacral slope improved from 44,50 ± 2,754 to 52,90 ± 3,734 (p 0,012) at last follow-up. In order to assess Lumbar Lordosis pre and post-operative we used as a reference, distally, the perpendicular to the posterior wall of S1 in those with a dysplastic dome format [12] and there was an overall increase of lordosis (mean 4,5°± 3,24) from 60,40° ± 5,09 to 64,90° ± 3,16, which can be explained by the increase of the sacral slope as consequence of the manoeuvres performed to reduce the slip angle and to facilitate reduction of the slipped vertebra, although it was not statistically significant (p 0,199).
Fusion was achieved systematically, without correction loss. Two patients, with pedicular screws only (without the transdiscal S1L5 screw), presented implant failure, with a break of S1 screws (Figure 2); this was asymptomatic and not associated with correction loss, hence no specific treatment was performed. There were no cases of re-operation and no other complications. The mean follow-up time was 4,3 years (51,63 ± 9,05 months).
Discussion
Although HGS is commonly diagnosed during childhood or adolescence, conservative treatment is often the first treatment option, and it is known that the need for surgical treatment is rarer in younger ages [13], explaining the average age of our population at the time of surgery of 19 years old. Treating pain-free patients is still a matter of debate - some authors propose surgical treatment for chronic postural anomaly associated with hamstring tightness [13], and others suggest considering the risk of slip progression, which is greater in high-grade patients compared to minor listhesis [14], as a relative indication for surgery. In our series all patients were symptomatic - persistent back pain and postural deformity were the main reasons to proceed to surgery; radicular symptoms were less frequent.
The objective of the surgical procedure should be to decompress neurologic structures and to promote fusion with a normal sagittal alignment [15,16] although, there is still no consensus on the optimal surgical option. HGS surgical treatment used to be no different from the lower-grade cases - as a matter of fact, in situ posterior fusions remain the most frequently performed procedure [17,18] but considering the higher risk of non-fusion and slip progression in these patients, more complex surgeries have been proposed [19] With a wide range of surgical options available, the question of utmost importance is what is the ideal type of surgery for each patient and which is the subjacent rationale for that choice.
The Spinal Deformity Study Group suggests a classification system based on sagittal alignment and the requirement of compensation mechanisms [11,20]. According to these authors, low-grade spondylolisthesis cases are included in the I-II-III types; high-grade spondylolisthesis is subdivided in type IV to VI accordingly: type IV is HGS with a balanced pelvis, type V is HGS with unbalanced pelvis (following the definition of Hresko, et al, [11] but sagittal aligned spine; and type VI, a sagittal unbalanced spine. This grading aims to guide the surgical procedure correspondingly - the more unbalanced the spine, the higher the need for reduction to achieve sagittal balance and a solid interbody fusion. All our HGS surgically treated patients were submitted to decompression and posterior instrumentation and achieved circumferential fusion; reduction maneuvers were attempted accordingly to the spinopelvic balance.
In SDSG type IV forceful reductions were not endeavored, as these patients are considered to have a balanced pelvis and normal sagittal alignment therefore they present without compensatory mechanisms, and surgical reduction of the listhesis is not mandatory - although the term “in situ” fixation is used, it is known that intra-operatively under general anesthesia and with the surgical positioning (prone with hips hyperextension and knee flexion), the elasticity of the intervertebral disk allows some degree of slippage reduction even without the aid of specific reduction efforts [21]. The patients with SDSG type VI (unbalanced spine) are the ones that need more investment in the slippage reduction attempt. Laminectomy allows access to the L5-S1 disk to perform a complete discectomy, allowing the realignment process. Another obstacle to the reduction is the presence of significant S1 dysplasia, usually characterized by a dome-shaped endplate, that hardens the translation of the L5 body over S1 - this can be overpassed by performing an osteotomy that flattens the S1 endplate perpendicular to the body posterior wall; the S1 osteotomy also enlarges the bony contact area, optimizing the odds to achieve arthrodesis18. Extending the instrumentation to L4 and placing temporary rods will allow further distraction and add an anchoring point to persuade the L5 pedicular screws posteriorly to perform the slippage reduction; the L4 screws can then be removed allowing the L4-L5 to keep its mobility, or be maintained to extend the fusion further to the L4-L5 - extending fusion to L4 should be considered when reduction is not satisfactory, in the presence of L4-L5 listhesis, severely degenerated L4-L5 disk, the integrity of L4-L5 facets after decompression, and the quality of L5 pedicles which can be indirectly measured by the surface area of the L5 transverse processes (higher risk of non-union when <2cm2) [22].
In some cases anatomic reduction cannot be achieved, nor is imposed - according to Labelle, et al. [23], in type VI subjects reduction should be preferred, but in difficult cases partial reduction (to grade II Meyerding) could suffice to achieve adequate sagittal alignment. Also, it is known that the slippage angle improvement is more important to gaining spinopelvic balance than the magnitude of the translation [24], and that the lumbosacral angle (particularly when left kyphotic) is an identified risk factor for non-union [17].
There are many instrumentation options described in the literature for treating HGS patients. Omidi-Khashani, et al. [25] performed posterior instrumentation from L4 to S1 without interbody graft, with no cases of non-union. First reported in 1982, the classic Bohlman technique [26], describes the creation of a hole through the center of S1 and L5 bodies which is filled by a fibula strut graft that promotes fusion. This technique was later modified [27] using a threaded titanium cage packed with morselized autologous bone, instead of the fibular graft, providing more rigid immobilization and eliminating the associated comorbidities. Grob, et al. [28] first described the usage of two cancellous bone screws inserted bilaterally through the pedicles of the lower vertebra into the body of the upper slipped vertebra, in a trans-discal fashion, also reporting 100% fusion rates. Moreau, et al. [17], reported a review of their technique extending the fusion proximally to L4 and applying two convergent screws in S1, one parallel to the plate and the other trans-discal, resulting in 14% of non-unions. In a biomechanical comparison of types of transdiscal fixation implants for HGS, the transdiscal screws were superior to transdiscal fibular strut and transdiscal titanium mesh cage in reducing segmental range-of-motion under mechanical stress [29]. In our series, posterior approach alone was performed, with decompression and circumferential fusion with posterolateral instrumentation and interbody autologous bone graft - fusion was achieved in all patients, without any cases of non-union.
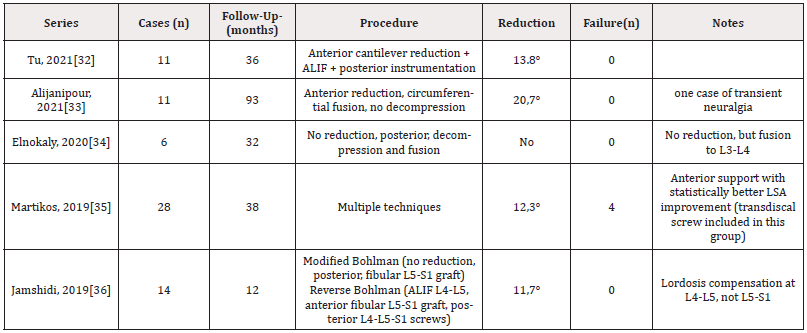
However, for the type VI in our series, although we were able to improve the slip angle by 18,2° and the spinal sagittal alignment, PT remained within normal values (26,1°) for this high PI (77,6°) group of patients [30], but we were not able to change the SDSG grade. These findings have been pointed out earlier by Labelle, et al. [31], where the postoperative improvement in slip angle, in spinal sagittal alignment and lumbar lordosis was correlated with a better outcome. At 4,3y follow up, all our patients are asymptomatic but if we aimed to achieve a more significant lumbar lordosis we believe that we would have to fuse up to L4 and in order to gain more lordosis at the suprajacent L4L5 disc. Looking at the literature (Table 1) on the surgical treatment of high grade spondylolisthesis, most of the published series have a similar number of patients and reduction was also within the same figures as in the one presented in this series.
Being a retrospective study, there are some intrinsic limitations to this analysis - we have to consider the possible weaknesses of the previously registered medical records, which can be biased, insufficient, or lacking homogeneity between different patients. There were no consistent scores registered pre-operatively, making it impossible to solidly compare clinical results. Being an infrequent condition, the relatively low number of HGS cases was expected, but limitative for a thorough analysis; the lack of a control group of untreated patients is also a statistical drawback. These limitations are reflected in the available literature - existing publications are quite limited, and well-designed strong evidence studies to evaluate operative and nonsurgical interventions for high-grade spondylolisthesis are very rare [37].
Conclusion
There is still no consensus on the surgical treatment of HGS. The most commonly applied strategy, in situ fusion, can be performed in patients with good spinopelvic balance, but reduction should be preferable in sagittal unbalanced cases. Posterior only approach with circumferential fusion with autologous bone graft and transdiscal L5-S1 screw is a safe and reliable option for the treatment of HGS in adolescents and young adults, preserving the L4L5 disc and achieving good clinical and radiologic outcomes.
Acknowledgment
Andre Barros, Jorge Mineiro, Nuno Lança, Luis Barroso, Kalina Hristova and Joao Cannas as authors of the paper.
Conflict of Interest
We have no conflict of interests related to this particular work.
References
- Herbiniaux G (1782) Traite sur divers accouchement laborieux, et sur polypes de la matrice. Brussels, JL DeBoubers.
- Wiltse LL, Newman PH, Macnab I (1976) Classification of spondylolisis and spondylolisthesis. Clin Orthop Relat Res (117): 23-29.
- Koslosky E, Gendelberg D (2020) Classification in Brief: The Meyerding Classification System of Spondylolisthesis. Clin Orthop Relat Res 478(5): 1125-1130.
- Fredrickson BE, Baker D, McHolick WJ, Yuan HA, Lubicky JP, et al. (1984) The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am 66(5): 699-707.
- Ebraheim N, Elgafy H, Gagnet P, Andrews K, Kern K, et al. (2018) Spondylolysis and spondylolisthesis: A review of the literature. J Orthop 15(2): 404-407.
- Hirano A, Takebayashi T, Yoshimoto M, Ida K, Yamashita T, et al. (2012) Characteristics of Clinical and Imaging Findings in Adolescent Lumbar Spondylolysis Associated with Sports Activities. J Spine 01(05): 1-3.
- Hu SS, Tribus CB, Diab M, Ghanayem AJ (2008) Spondylolisthesis and spondylolysis. Instr Course Lect 57: 431-445.
- Wiltse LL, Jackson DW (1976) Treatment of spondylolisthesis and spondylolysis in children. Clin Orthop Relat Res (117): 92-100.
- Randall RM, Silverstein M, Goodwin R (2016) Review of Pediatric Spondylolysis and Spondylolisthesis. Sports Med Arthrosc Rev 24(4): 184-187.
- Brien MF (2004) Group SDS. Radiographic Measurement Manual. Medtronic Sofamor Danek USA.
- Hresko MT, Labelle H, Roussouly P, Berthonnaud E (1976) Classification of High-Grade Spondylolistheses Based on pelvic version and spine balance. Spine 32(20): 2208-2213.
- Brien MF, Kuklo TR, Blanke M (2004) Radiographic Measurement Manual, Spinal Deformity Study Group (SDSG), Medtronic Sofamor Danek.
- Jalanko T, Helenius I, Remes V, Lamberg T, Tervahartiala P, et al. (2011) Operative treatment of isthmic spondylolisthesis in children: A long-term, retrospective comparative study with matched cohorts. European Spine Journal 20(5): 766-775.
- JE L (1999) Spondylolisthesis in children. Spine (Phila Pa 1976) 24(24): 2640-2648.
- Lian XF, Hou TS, Xu JG, Zeng BF, Zhao J, et al. (2014) Single segment of posterior lumbar interbody fusion for adult isthmic spondylolisthesis: reduction or fusion in situ. European Spine Journal 23(1): 172-179.
- Kwon BK, Berta S, Daffner SD, Vaccaro AR, Hilibrand AS, et al. (2003) Radiographic Analysis of Transforaminal Lumbar Interbody Fusion for the Treatment of Adult Isthmic Spondylolisthesis. J Spinal Disord Tech 16(5): 469-476.
- Moreau S, Lonjon G, Guigui P, Lenoir T, Garreau de Loubresse C, et al. (2016) Reduction and fusion in high-grade L5-S1 spondylolisthesis by a single posterior approach. Results in 50 patients. Orthopaedics and Traumatology: Surgery and Research 102(2): 233-237.
- Longo UG, Loppini M, Romeo G, Maffulli N, Denaro V (2014) Evidence-based surgical management of spondylolisthesis: reduction or arthrodesis in situ. J Bone Joint Surg Am 96(1): 53-58.
- Pizzutillo PD, Mirenda W, MacEwen GD (1986) Posterolateral fusion for spondylolisthesis in adolescence. J Pediatr Orthop [Internet] J Pediatr Orthop 6(3): 311-336.
- Labelle H, Mac Thiong JM, Roussouly P (2011) Spino-pelvic sagittal balance of spondylolisthesis - a review and classification. European Spine Journal 20(S5): 641-646.
- Violas P, Lucas G (2016) L5S1 spondylolisthesis in children and adolescents. Orthopaedics and Traumatology: Surgery and Research [Internet] Elsevier Masson SAS 102(1): S141-S147.
- Molinari MRW, Bridwell KH, Lenke LG, Ungacta FF, Riew KD, et al. (1999) Complications in the Surgical Treatment of Pediatric High-Grade , Isthmic Dysplastic Spondylolisthesis A Comparison of Three Surgical Approaches 24(16): 1701-1711.
- Labelle H, Mac Thiong JM, Roussouly P (2011) Spino-pelvic sagittal balance of spondylolisthesis: a review and classification. European Spine Journal 20: 641-646.
- Bradford DS, Boachie Adjei O (1990) Treatment of severe spondylolisthesis by anterior and posterior reduction and stabilization. A long-term follow-up study. J Bone Joint Surg Am 72(7): 1060-1066.
- Omidi Kashani F, Hootkani A, Jarahi L, Rezvan M, Moayedpour A, et al. (2015) Radiologic and Clinical Outcomes of Surgery in High Grade Spondylolisthesis Treated with Temporary Distraction Rod. Clin Orthop Surg 7(1): 85-90.
- Bohlman HH, Cook SS (1982) One-stage decompression and posterolateral and interbody fusion for lumbosacral spondyloptosis through a posterior approach. Report of two cases. J Bone Joint Surg Am 64(3): 415-418.
- Slosar PJ, Reynolds JB, Koestler M (2001) The axial cage. a pilot study for interbody fusion in higher-grade spondylolisthesis. Spine J 1(2): 115-120.
- Grob D, Humke T, Dvorak J (1996) Direct pediculo-body fixation in cases of spondylolisthesis with advanced intervertebral disc degeneration. Eur Spine J [Internet] Eur Spine J 5(4): 281-285.
- Kerr HL, Gee A, Fernandes RJR, Kanawati AJ, Jin W, et al. (2021) Biomechanical comparison of 3 types of transdiscal fixation implants for fixing high-grade L5/S1 spine spondylolisthesis. Spine Journal 21(9): 1587-1593.
- Le Huec JC, Hasegawa K (2016) Normative values for the spine shape parameters using 3D standing analysis from a database of 268 asymptomatic Caucasian and japonese subjects. Eur Spine J 25(11): 3630-3637.
- Labelle H, Roussouly P, Berthonnaud E, Dimnet J, O Brien M, et al. (2005) The importance of spino-pelvic balance in L5S1 developmental spondylolisthesis. Spine 6S: S27-S33.
- Tu KC, Shih CM, Chen KH, Pan CC, Jiang FC, et al. (2021) Direct reduction of high-grade lumbosacral spondylolisthesis with anterior cantilever technique - surgical technique note and preliminary results. BMC Musculoskelet Disord BMC Musculoskeletal Disorders 22(1): 1-10.
- Alijanipour P, Heffernan MJ, King AGS (2021) Single-level fusion without decompression for high-grade spondylolithesis in adolescents: a novel surgical strategy. Spine Deform [Internet] Springer International Publishing 9(5): 1457-1464.
- Elnokaly MA, Adawi MM, Nabeel AM (2020) Pedicular lumbosacral spine fusion for adult/adolescent lumbar developmental high-grade spondylolisthesis. Surg Neurol Int 11: 416.
- Martikos K, Greggi T, Faldini C (2019) High grade isthmic spondylolisthesis; Can reduction always re-align the unbalanced pelvis? BMC Musculoskelet Disord BMC Musculoskeletal Disorders 20(1): 1-5.
- Jamshidi A, Levi AD (2019) Reverse Bohlman technique for treatment of high-grade spondylolisthesis in an adult population. Journal of Clinical Neuroscience 69: 230-236.
- Xue X, Wei X, Li L (2016) Surgical versus nonsurgical treatment for high-grade spondylolisthesis in children and adolescents: A systematic review and meta-analysis. Medicine (United States) 95(11): 1-6.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.