Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
The Benefits of Choledochoscopy During Laparoscopic Surgery of Bile Duct Exploration for Choledocholithiasis
*Corresponding author: Sotirov DY, MBAL “Sveti Panteleymon” hospital, Yambol, Bulgeria.
Received: May 31, 2024; Published: June 07, 2024
DOI: 10.34297/AJBSR.2024.22.003011
Abstract
Study Aim: The aim of this study is to assess the feasibility of intraoperative cholangioscopy during laparoscopy. Also we need to evaluate the impact of this method in the detection and treatment of common bile duct stones.
Patients and Method: From 2021 to 2024 26 patients [mean age: 73,6 years] with symptomatic, complicated or retained bile duct stones were operated on laparoscopically. lntraoperative cholangioscopy [IOCs]was attempted in all patients and was successful. The technique was combined with intraoperative laparoscopic cholecystectomy for patients with gallbladder. The intraoperative cholangiography was performed with a catheter [diameter: 5 F] introduced through the cystic duct or after laparoscopic choledochotomy. The intraoperative choledochoscopy was attempted by 3mm or 5mm choledochoscope depending on the size of the common bile duct or cystic duct. In case of detection of common bile duct stones [CBDS], we try a laparoscopic approach for extraction of the bile duct stones. There was a failure of this extraction technique for 2 patients.
Results: Intraoperative choledochoscopy was successfully performed in 26/100%/. The mean duration of this examination was 20min [15-55]. It was easier to complete choledochoscopy in patients with uncomplicated cholelithiasis [16 patients], compared to patients with acute cholecystitis [10 patients]. For the first 10 patients we combined intraoperative choledochoscopy with cholangiography. After that because of the better visualization by scope we abandoned IOCs. Extraction of common bile duct stones was executed by laparoscopic approach except in 2 patients where extraction was successful by laparotomy. All laparoscopic intervention was finished by placement of T- tube into the common bile duct. Postexploratory T-tube cholangiography was a routine procedure on the 12th day after procedure for verification of clear CBD.
Conclusions: Routine laparoscopic intraoperative choledochoscopy appears to be very reliable method for the diagnosis and extraction of retained bile duct stones. It is a safe, physiological, cost-effective, and efficient method.
The most common benign pathology of the bile ducts worldwide is choledocholithiasis defined as the presence of stones in the common bile duct (CBD). According to the different authors, CBD stones are present in 10-25% of all patients undergoing cholecystectomy for stones in the gallbladder and in about 10% of patients who undergo cholecystectomy for symptomatic cholelithiasis (gallstones in the gallbladder). On the other hand, 95% of patients with confirmed choledocholithiasis have stones in the gallbladder too. CBD stones can remain silent for a long time, but they can also be associated with recurrent upper abdominal pains, intermittent jaundice, cholangitis, and recurrent pancreatitis. Patient with cholecystolithiasis and bile duct stone has a risk/up to 35% of cases/ for a pancreatitis or cholangitis, if the CBD become obstructed. Numerous treatment algorithms have been proposed for this disease, however, up to 10% of these diagnostic and therapeutic procedures may fail. A retained common bile duct stone after an operation for biliary lithiasis continues to be a problem despite advances in surgical technique. Conventional bile duct surgery for gallstones in the case of jaundice is a common operation but there is a high risk of residual stones after treatment. Exploring the bile ducts by traditional operative technique without clear visibility of the obstruction is the problem that should be overcome. The incidence of missed common bile duct stones, when expressed as a percentage of all conventional bile duct explorations is high. According to different series it is between 14% and 30% [1-3].
Today there are clear indications for CBD exploration that could be applied to routine cholangiography (IOCs) or choledochoscopy.
i. Jaundice (now, in the past).
ii. History of gallstone pancreatitis.
iii. Common bile duct larger than 5 to 7 mm in diameter.
iv. Cystic duct larger than 3 mm in diameter.
v. 5 Unclear bile duct anatomy.
vi. Common bile duct stones visualized on preoperative ultrasound.
vii. Possible bile duct injury.
viii. Derangement of liver tests (AP, g GT, bilirubin).
Nowadays, for the diagnosis and treatment of CBD stones are proposed several techniques.
Intraoperative Cholangiography (IOCs)
Intraoperative cholangiography involves the radiographic imaging of the biliary system during surgery. During the procedure, a surgeon injects a contrast material through the cystic duct to visualize the intrahepatic and extrahepatic bile duct system. Fluoroscopic pictures are taken in real time as the contrast agent passes through the biliary system, allowing a dynamic visualization of cystic duct, common bile duct and duodenum [4].
The first report delineating the anatomy of the biliary tree was published in 1918 by Reich using bismuth and petrolatum as a contrast agent [5]. In 1930, Ginzburg and Benjamin used a lipiodol solution to identify common bile duct stones [6]. Mirizzi in 1932 reported the first series of routine IOCs using lipiodol [7]. Several years later in 1939, Hicken et al. by using IOCs demonstrated that the incidence of retained bile duct stones is up to 12% after “blind old school” bile duct exploration [8].
Introduction of C-arm mobile image intensifier in 1978, provide high-definition images with clear anatomy of the extrahepatic bile ducts [9].
Benefits with the use of IOCs are well known:
i. Clear identification of the anatomy and any aberrant anatomy of the extrahepatic bile ducts
ii. Identification of bile duct stones.
iii. Identification of bile duct injury.
Although there are technological progress and clear benefits by application of this technique in clinical practice it is not became a routine procedure for discovering of bile duct obstruction. Possible explanations for that are prolongation of operative time, obtaining unclear images, technical difficulties during application of the procedure, radiation to the operating room personnel [10].
ERCP
Today endoscopic retrograde cholangiopancreatography (ERCP) is a gold standard for the transoral treatment of common duct stones either alone or combined with cholecystectomy/as two-stage procedure/. The principal drawbacks are: significant failure rate, a morbidity rate of up to 15 per cent and mortality rate of about 1 per cent, depending on the experience of endoscopist. In addition this procedure does not deal with cholecystolithiasis at the same time of the intervention.
ERCP has become the first-line modality for the diagnosis and treatment of pancreatobiliary diseases (mainly biliary obstruction and bile duct stones). Today ERCP can be performed before, during, or after cholecystectomy, and may also be combined with either sphincterotomy (transection) or sphincteroplasty (papillary dilatation) for stone retrieval from the CBD or stent placement.
The indication for ERCP is a distal CBD obstruction with CBD dilation, confirmed by MRCP.
The procedure is usually performed under conscious sedation. Biliary decompression by ERCP, even essential in the management of obstructive jaundice, may provoke also acute obstructive cholangitis (AOC), one of the procedure-related complications related to the ERCP.
The incidence of post-ERCP cholangitis ranges from 0.4 to 10%, carrying a mortality rate of 0.1%. If there is a failure of ERCP for biliary stone removal the risk for postoperative AOC is multiplied. However, endoscopic sphincterotomy for bile duct stones has a disappointing 8-10% rate of long-term biliary complications, including recurrent or residual ductal stones, cholangitis, stenosis of the papilla, and biliary pancreatitis. Goodall and Macadam referred to a 28% rate of late symptoms related to low-grade cholangitis following papillosphincterotomy.
Although ERCP has increasingly become a very popular procedure, post-ERCP complication rates may reach 9.7%, with a mortality rate of 0.7%. The four most common complications are [11-19]:
1. Post-ERCP pancreatitis.
2. Biliary or duodenal perforation.
3. Gastrointestinal bleeding.
4. Acute cholangitis, cholecystitis, liver abscess.
Intraoperative Choledochoscopy
The introduction of choledoscope started back in 1887 when Thornton described two successful cases in which common bile duct stones were removed via a dilated cystic duct [20]. In 1890, Courvoisier described an operation for retrieving a retained stone [21].
In 1937 when Babcock and Hollenberg and Eikner, each working independently, used a cystoscope to remove gallstones through a cholecystotomy [22,23]. The development of the first modern rigid choledochoscope should be accorded to Monroe McIver in 1941 when he modified a 5mm in diameter cystoscope with a right angle 7 cm from the tip [24].
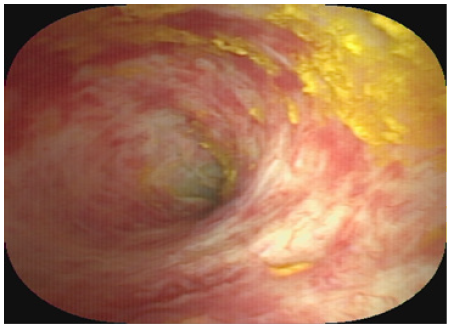
Since that time, no significant work was published until Wildegans reported his experience with his new scope at the Surgical Conference in Berlin in 1953 [25]. With the development of fiberoptics, a first flexible scope with better manoeuvrability and flexibility was introduced by Shore and Lippman in 1965 who reported a series of 100 cases [26]. More recently, Hopkins of England, who developed a special rod lens system, which was integrated into the rigid choledochoscope [27]. In the 1970s Olympus introduced the new series of choledochoscopes with improved fibreoptics and manoeuvrability. These flexible choledochoscopes were gradually improved and modified by Ashby up to now [20] (Figure 1).
According to different series exploration of common bile duct (CBD) for stones is needed in 12 per cent of patients who undergo cholecystectomy. If we apply the traditional “blind” operative technique for bile duct examination without clear visibility of the obstruction there is a high risk of retained bile duct stones after the procedure. During the historical evolution of bile duct surgery for stones there was always a need to find out a reliable visualization technique for inspection of the common bile duct.
In the beginning the incidence of retained stones after ‘blind’ CBD exploration was approximately 10 per cent. Afterwards with the application of rigid choledochoscope in clinical practice this complication had been reduced to approximately 4 per cent. Nowadays with the introduction of flexible choledochoscope in practice that incidence could be lowered to about 2 per cent.
Patients and Methods
Patients
From 2021 to 2024 26 patients (mean age: 73,6 years) with laparoscopic exploration of CBD were undertaken. All the patients were selected for laparoscopic common duct exploration. Laparoscopic exploration of the CBD was indicated by the presence of a bile duct stone on ultrasound or CT. For 10 patients ductal filling defect was confirmed on IOCs. Indications for exploration for all patients was a image of dilated CBD, increased value of liver cholestatic enzymes/AP, g GT/ and bilirubin. All the operations were performed by one surgeon. 18 patients had risk factors for choledocholithiasis (history of jaundice, raised liver enzyme levels or biliopancreatitis). At the time of admission 15 patients had clinical signs of acute cholecystitis, acute biliopanceatitis. For these patients with acute signs duration between admission and operation was about 5 days. Four patients had a previous attempt for bile duct stone extraction.
Technique
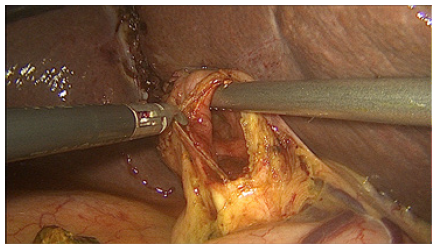
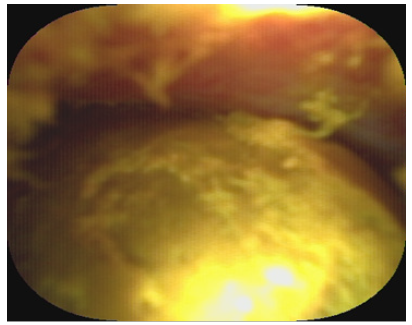
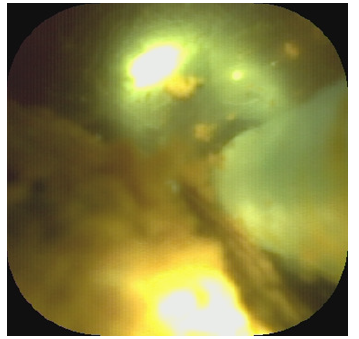
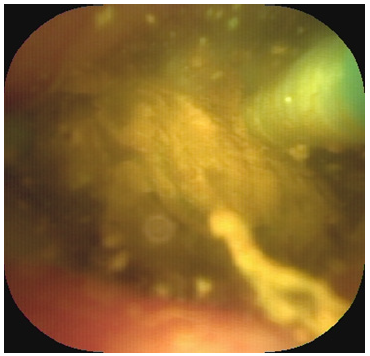
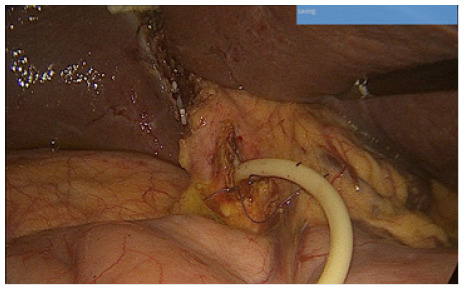
In our serie for laparoscopic exploration of CBD we use two different size of choledochoscope 3mm and 5 mm/Shanghai SeeGen Photoelectric Technology Co.Ltd.-Briview/. The choice depends on the diameter of CBD. The 5mm choledochoscope has a working channel for introduction of Dormia basket. For stone extraction we can utilize also a Fogarty catheter or a larger Dormia basket placed alongside the scope.
The choledochoscope was introduced through a standard choledochotomy incision about 5 mm long on the supraduodinal portion of the common bile duct. If the cystic duct is at least 5 mm in diameter we can use a 3mm choledochoscope for CBD access via transcystic route. Our team applied this approach in 4 patients. The scope for examination of the distal part of CBD, papilla of Vateri and duodenum was passed into the peritoneal cavity through a 5 mm trocar at the right hypochondriac region near the hypohondrium. For examination of proximal CBD, left and right hepatic duct we use different 5 mm port at the level of umbilicus. After the introduction in the abdominal cavity the shaft of the scope is manipulated by the surgeon with the help of two atraumatic forceps. We can use also the tip of the cannula to control the scope. At the same time the assisstants should help this CBD navigation by traction of the stay sutures placed on both sides of the choledochotomy incision. Without active support of the assistant the scope manipulation could be very difficult or impossible. For the first 10 patients before intraoperative choledochoscopy we confirmed retained bile duct stones by 5Fr cholangiographic catheter placed through incision of the cystic duct. The gallbladder was left in situ for the procedure and was used to maintain tension on the cystic duct helping the introduction of the catheter. At the end of the procedure we place 8 Fr T-tube into the CBD for 45 days. The incision of choledochotomy was closed using interrupted 4/0 polyglactin sutures and the absence of leakage is verified by injection of 20ml saline through the T tube. We do not use primary close of CBD after its exploration and manipulation (Figures 2-10).
We always place a large subhepatic drainage tube for 5 days after the procedure.
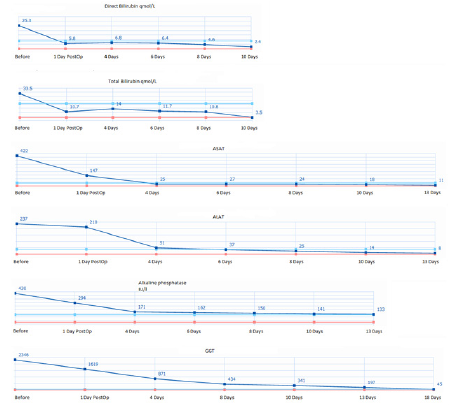
For all operated patients no residual stone in the CBD was confirmed by cholangiography through a placed T- tube on the 12th postoperative day.
Results
Laparoscopic exploration of the CBD was undertaken for 26 patients/100%/. Ten patients had common duct filling defects on cholangiography before exploration. The CBD was dilated between 10-35mm measured on the CT scan. 18 patients had multiple stones in the CBD and 8 patients had single stone. There was a failure of the laparoscopic stone extraction for 2 patients with subsequent successful effect by open approach. The reason for that was a difficult manipulation of the scope.
The mean duration of the laparoscopic BD examination was 20min (15-55). Laparoscopic cholecystectomy was combined with laparoscopic BD exploration and stone extraction in 21 patients. No complications after the procedure and residual CBD lithiasis confirmed on the 12th and 30th day by T-tube cholangiography (Tables 1,2).
Discussion
According to different series exploration of common bile duct (CBD) for stones is needed in 12 per cent of patients who undergo cholecystectomy. If we apply the traditional “old school blind” operative technique for bile duct examination without clear visibility of the obstruction there is a high risk of retained bile duct stones after the procedure. During the historical evolution of bile duct surgery for stones there was always a need to find out a reliable visualization technique for inspection of the common bile duct.
In the beginning the incidence of retained stones after ‘blind’ CBD exploration was approximately 10 per cent. Afterwards with the application of rigid choledochoscope in clinical practice this complication had been reduced to approximately 4 per cent. Nowadays with the introduction of flexible choledochoscope in practice that incidence could be lowered to about 2 per cent depending on the surgeon’s experience.
The technique of laparoscopic cholecystectomy is now a gold standard established for the treatment of cholecystolithiasis. This laparoscopic advancement has brought with it a new perspective on the management of common bile duct (CBD) stones at the same time with cholecystectomy [28-30].
Today different teams use different types of choledochoscope according to the patient’s access and their preference. The endoscopists utilise peroral access, for the interventional radiologist this approach can be percutaneous transhepatic route or percutaneous transenteric via access loop. Each route has advantages and limitations but peroral and percutaneous transhepatic access are the most widely discussed in the literature [29].
Our experience is centred on the laparoscopic surgical access which can be intraoperative transcystic, or intraoperative transcholedochal access.
Why we propose this access for the treatment of CBD? The answer is simple, because it proposes a treatment at the same time with cholecystectomy/one-stage intervention/, there is an acceptable risk compared with the other techniques. This laparoscopic approach is miniinvasive and at the same time it is more physiological than other treatment modalities (e.g.no sphincterotomy).
In this serie of 26 patients there was 100 % retrieval of BD stones. Laparoscopic exploration was successful in all 26 patients and extraction in 24 patients.
Conclusion
The overall success rate of laparoscopic exploration for this serie is 100% and extraction is successful except in two patients. Absence of postinterventional complications and mortality supports this laparoscopic approach as safe, physiological, cost-effective, and efficient method.
References
- Way LW, Admirand WH, Dunphy JE (1972) Management of choledocholithiasis. Ann Surg 176: 347-357.
- Hall RC, Sakiyalak P, Kim SK, L S Rogers, W R Webb, et al. (1973) Failure of operative cholangiography to prevent retained common duct stones. Am J Surg 125(1): 51-63.
- M B Corlette Jr, S Schatzki, F Ackroyd (1978) Operative Cholangiography and Overlooked Stones. Arch Surg 113(6): 729-734.
- Samah Osailan, Muhanad Esailan, Abdulaziz M Alraddadi, Faisal M Almutairi, Zaid Sayedalamin, et al. (2023) The Use of Intraoperative Cholangiography During Cholecystectomy: A Systematic Review. Cureus 15(10): e47646.
- Reich A (1918) Accidental injection of bile ducts with petrolatum and bismuth paste. JAMA 71: 1555.
- Ginzburg L, Benjamin EW (1930) Lipiodol studies of postoperative biliary fistulae. Ann Surg 91(2): 233.
- Mirizzi PL (1932) La Cholangiografia Durante las Operaciones de las Vias Biliares. Bol Soc Cir Buenos Aires 16: 1133.
- Hicken NF, Best RR, Hunt HB (1936) Cholangiography. Ann Surg 103: 210.
- Berci G, Shore JM, Hamlin JA, Morgenstern L (1978) Operative fluoroscopy and cholangiography. The use of modern radiologic technics during surgery. Am Surg 135(1): 32-35.
- BV MacFadyen (2006) Intraoperative cholangiography: past, present, and future. Surg Endosc 20: S436-S440.
- Wada K, Takada T, Kawarada Y, Nimura Y, Miura F, et al. (2007) Diagnostic criteria and severity assessment of acute cholangitis: Tokyo guidelines. Journal of Hepato-Biliary-Pancreatic Surgery 14(1): 52-58.
- Fumihiko Miura, Kohji Okamoto, Tadahiro Takada, Steven M Strasberg, Horacio J Asbun, et al. (2018) Tokyo guidelines 2018: Initial management of acute biliary infection and flow chart for acute cholangitis. Journal of Hepato-Biliary-Pancreatic Sciences 25(1): 31-40.
- Dasari BVM, Tan CJ, Gurusamy KS, Martin DJ, Kirk G, et al. (2013) Surgical versus endoscopic treatment of bile duct stones. Cochrane Database of Systematic Reviews (12): 1-102.
- Traverso LW, Roush TS, Koo K (1995) CBD stones–outcomes and costs. Laparoscopic transcystic techniques other than choledochoscopy. Surgical Endoscopy 9(11): 1242-1244.
- Paganini AM, Guerrieri M, Sarnari J, De Sanctis A, D’Ambrosio G, et al. (2007) Thirteen years’ experience with laparoscopic transcystic common bile duct exploration for stones Effectiveness and long-term results. Surgical Endoscopy 21(1): 34-40.
- Goodall RJR, Macadam RCA (2004) Long-term symptoms following endoscopic sphincterotomy for common bile duct stones. Surgical Endoscopy 18(3): 363-366.
- Helton WS, Ayloo S (2019) Technical aspects of bile duct evaluation and exploration: An update. The Surgical Clinics of North America 99(2): 259-282.
- Lee D-H, Ahn YJ, Lee HW, Chung JK, Jung IM, et al. (2016) Prevalence and characteristics of clinically significant retained common bile duct stones after laparoscopic cholecystectomy for symptomatic cholelithiasis. Annals of Surgery Treatment Research 91(5): 239-246.
- Lee YT, Sung J Barron TH, Kozarek R, Carr-Lock DL (2008) Choledocholithiaisis (First Edition). Elsevier Publications 357-366.
- Ashby BS (1978) Choledochoscopy. Clin Gastroenterol 7: 685-700.
- Courvoisier L (1890) Casuistisch-Staiistische Beitraye zur Patholoyie und Chirurgie der Gallenwenge. Leipzig: Vogel.
- Babcock WW (1937) Management of biliary diseases and their surgical complications. Penn Med J pp. 604.
- Hollenberg HG, Eikner WC (1941) Cholecystoscopy. Surgery 2: 37.
- Mclver MA (1941) Instrument for visualizing interior of the common duct at operation. Surgery 9: 112.
- Wildegans VH (1953) Grenzen der Cholangiographie und Aussichten der Endoskopie der Tiefen Gallenwege. Med K/in 35: 1270.
- Shore JM, Shore E (1970) Operative biliary endoscopy experience with the flexible choledochoscope in 100 consecutive choledocholithotomies. Ann Surg 171(2): 269.
- Shore JM, Morgenstern L, Berci G (1971) An improved rigid choledochoscope. Am JSurg 122(4): 567-568.
- Tsinrong Lee, Thomas Zheng Jie Teng, Vishal G Shelat (2021) Choledochoscopy: An update. World J Gastrointest Endosc 13(12): 571-592.
- Samah Osailan, Muhanad Esailan, Abdulaziz M Alraddadi, Faisal M Almutairi, Zaid Sayedalamin, et al. (2023) The Use of Intraoperative Cholangiography During Cholecystectomy: A Systematic Review. Cureus 15(10): e47646.
- BV MacFadyen (2006) Intraoperative cholangiography: past, present, and future. Surg Endosc 20: S436–S440.








 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.