Mini Review 
 Creative Commons, CC-BY
Creative Commons, CC-BY
The Effectiveness and Safety of Meshed Skin Transplantation and Postoperative Care
*Corresponding author: Canut Denisa Maria, PhD Student, Faculty of Medicine, University of Medicine and Pharmacy Craiova, Romania, Corp A, 2 Petru Rareș Street, 0773889455.
Received: April 16, 2024; Published: April 18, 2024
DOI: 10.34297/AJBSR.2024.22.002931
Abstract
Aim: The purpose of the research was to evaluate the effectiveness and safety of meshed skin transplant procedures and postoperative care in improving healing and reducing complications in patients with extensive skin injuries. Patients.
Materials and Methods: A retrospective study was conducted at the Clinic of Pediatric Surgery and Orthopedics in the County Clinical Emergency Hospital of Craiova. To carry out this study, a patient was selected who presented cutaneous lesions that cannot be closed by direct suturing and require skin transplantation.
Results: The procedure of meshing skin grafts has demonstrated an excellent ability to cover extensive wounds, allowing a significant expansion of the graft, which is essential in cases with a limited surface area of available donor skin. Meshing improved the flexibility of the graft and facilitated better conformity to the irregular contours of the recipient area. Suturing techniques and graft application are essential for the success of the surgery, and their immediate post-operative appearance is often very different from what it will look like once healing is complete. The procedures had a significant impact on the patient's quality of life, restoring function and physical integrity, and improving aesthetic appearance and self-confidence.
Conclusions: The patient showed an improved rate of healing and integration of the skin graft, suggesting that the techniques used in the study are suitable for optimizing the healing process. The grafting was consistent and presented a low percentage of complications, such as infection or graft necrosis.
Keywords: Burns, Pediatric burns, Meshing, Skin graft, Suturing techniques
Introduction
The practice of skin grafting has a long and fascinating history, beginning with its ancient origins in India. It is believed that the initial technique of skin grafting was developed there about 2,500 years ago. This ancient technique was gradually perfected and became known and practiced in Western medicine [1]. Skin grafting is an essential and frequently used technique in dermatological surgery. It involves transplanting skin from one area of the body to another to cover a defect or wound. The process is vital in cases where direct closure of the wound is not possible due to the size or location of the excision [2]. Skin grafts are a fundamental component in reconstructive surgery, with the main types being full-thickness skin grafts, split-thickness skin grafts, composite grafts, and free cartilage grafts. Full-Thickness Skin Grafts (FTSGs) include both the epidermal and the entire dermal layer of the skin. On the other hand, Split-Thickness Skin Grafts (STSGs) consist of the epidermis and a part of the dermis and are classified as thin, medium, or thick, depending on the dermal portion included [3]. Split-Thickness Skin Grafts (STSGs) include the epidermis and a part of the dermis. STSGs are used to cover large areas and are more likely to be successful in terms of graft 'take' because they are less demanding in terms of blood supply. However, the cosmetic outcome may be less favorable compared to full-thickness grafts, and the chances of contracture are higher [4].
In 1875, a Scottish surgeon named George Lawson Wolfe was the first to describe in detail a Full-Thickness Skin Graft (FTSG), involving the removal of the entire thickness of the skin, including both the epidermis and the entire dermis. These grafts provide a superior aesthetic and functional result, as they are thicker and contain the entire structure of the dermis but require more advanced technique and a well-vascularized recipient site to survive [5]. Full-Thickness Skin Grafts (FTSGs) consist of the epidermis and the entire thickness of the dermis. They are generally used for smaller, more visible areas where a better cosmetic result is desired. FTSGs offer a better match in terms of skin texture and color but require a well-vascularized wound bed due to their thicker nature [6]. Skin grafts are chosen when healing by secondary intention (leaving the wound to heal on its own) or primary closure (direct stitching of the wound) are not viable options. For example, in the case of large wounds or in areas with high skin tension, grafts may be the preferred solution [7]. However, skin grafts are not suitable for all areas of the body. Avascular zones, such as exposed bone, cartilage without perichondrium, tendon, nerve, or fascia, cannot support graft because they lack the blood supply and granulation tissue necessary for graft survival [8]. Flap closures, as an alternative, involve transferring tissue from an adjacent area to the wound, maintaining its blood supply. Flaps are often preferred for their superior cosmetic and functional results, especially in areas with high visibility, such as the face. However, flap operations are generally more complex and require greater surgical skill [9].
Although skin grafting is technically simpler, it requires careful planning. The donor site must be chosen based on the color, texture, and thickness of the skin to achieve the best cosmetic results. The recipient site must be properly prepared to receive the graft, ensuring it is free from infection and has an adequate blood supply to support the new skin [10]. Post-operative care is crucial for the success of a skin graft. This includes ensuring adequate immobilization of the graft, monitoring for signs of infection or rejection, and managing the donor site.
Materials and Methods
The purpose of the research is to evaluate the effectiveness and safety of meshed skin transplant procedures and postoperative care in improving healing and reducing complications in patients with extensive skin injuries. A retrospective study was conducted at the Pediatric Surgery and Orthopedics Clinic of the County Clinical Emergency Hospital of Craiova. This study initially included a total of 80 patients, who were followed from January 1, 2017, to December 31, 2018. The patients presented different degrees of burns and varied characteristics, including their environment of origin, the manner of burn occurrence, affected area, and burn severity. Each case had a different prognosis. Of the 80 patients evaluated for our study on the effectiveness and safety of meshed skin transplantation, each underwent a comprehensive preoperative assessment that included medical analyses, consultations, and evaluations of wound conditions. Our inclusion criteria were strict and well-defined, requiring patients to have skin lesions that could not be closed by direct suturing and that required skin transplantation. Also, they had to be free of any medical conditions that could interfere with wound healing or the integration of skin graft.
The patient selected for this operation met all the inclusion criteria and did not have any of the exclusion conditions, which included active infections, uncontrolled chronic diseases, or a history of smoking, which could compromise wound healing. The patient was informed in detail about the procedure, risks, benefits, and the nature of the study, including the fact that the healing process would be closely monitored and documented for research purposes. After giving informed consent, the patient was scheduled for surgery. The surgical team prepared the patient according to the standard protocol, with special attention given to sterility and preparation of the affected area. The skin transplant was successfully performed, and the patient was monitored postoperatively for any signs of complications. The healing process was documented through a series of photographs and regular clinical evaluations, according to the study's methodology. Emphasis was placed on the clinical evaluation and management of each case, from the time of admission to the time of discharge from the hospital unit.
The materials were as follows:
i. Surgical equipment used for skin transplantation, including instruments for meshing and fixation.
ii. Woven yellow textile compressive dressings and other consumable materials.
iii. Antiseptics are used for preparing and cleaning the surgical area.
iv. A photographic documentation system for visually recording the healing process.
v. Observation charts and data collection forms for recording all relevant information.
Results
Figure 1 depicts a skin grafting process. In skin grafting, a piece of healthy skin is transplanted to another part of the body where skin has been lost. The device shown is a key instrument in this process; it is known as a skin graft mesher. This tool allows surgeons to make small cuts in the harvested skin, creating a mesh-like pattern. This skin grafting pattern has several clinical benefits: the process of placement expands the skin, allowing a smaller piece of donor skin to cover a larger area of the wound. This is particularly important in cases where there is a limited area of healthy skin available for harvesting. The mesh allows the skin graft to be more flexible, which is beneficial when applied to parts of the body that move or flex frequently, such as joints. The mesh pattern can facilitate the drainage of body fluids, which is essential for preventing fluid accumulation under the graft, a condition known as seroma. It also allows new tissue to grow through the mesh, which can improve the graft's integration with the wound bed and enhance healing. With the mesh pattern, it is easier for medical staff to monitor the healing process and identify any potential infections or complications. Skin grafting requires a sterile environment, as seen in the image by the use of gloves and, presumably, a clean operating room, to minimize the risk of infection. The success of the skin graft depends on careful preparation of both the donor and recipient sites, the skills of the medical team, and subsequent patient care, including keeping the area clean, avoiding injuries, and sometimes performing physical therapy to ensure the best functional outcome. This procedure reflects the complex and collaborative nature of surgical interventions, showcasing the blend of human skills and technological advancement in modern medicine (Figure 1).
In Figure 2, a stage of a skin transplant is illustrated. The surgeon is holding with their left hand a part of the patient's body, which is partially covered with surgical drapes. An extensive area of red and exposed skin is observed, representing a donor site for the skin transplant. The skin transplant procedure is essential for patients suffering from extensive injuries, where natural skin regeneration is insufficient. The grafts come from the patient, known as an autograft. In the case of autografts, a healthy portion of skin is taken from one region of the body and transferred to the affected area. This type of transplant has the highest success rate because it reduces the risk of tissue rejection. After applying the graft, careful monitoring of the area is crucial to ensure the attachment and integration of the transplanted tissue. The patient will need to follow postoperative instructions strictly, including resting the affected area, avoiding exposure to the sun or other heat sources, and following a specific hygiene and care regimen to facilitate optimal healing and minimize the risk of infection or complications (Figure 2).
In Figure 3, the ongoing medical procedure is presented, involving interventions on a patient's limbs. The skin on the patient's limb is exposed and is being prepared for a skin transplant. A large incision or an area where the skin has been removed can be observed, leaving the subcutaneous tissue exposed. The red coloration is the application of an antiseptic solution. The procedure requires precision and attention to detail to minimize the risk of infection and to ensure proper healing. The area is well-lit, which is vital for the medical staff to work accurately (Figure 3).
Figure 4 indicates a detail of a specialized surgical procedure, using a skin mesher device. This instrument is essential in reconstructive surgery and wound management, particularly when skin transplants are needed to cover large skin defects, such as those caused by severe burns or extensive surgical interventions. The skin mesher device is used to transform a solid skin graft into a network, creating small slits that allow the graft to expand over a larger area and adapt to the irregular contours of the skin defect. This technique also improves the vascularization and survival of the graft, facilitating its integration with the lesion and allowing efficient drainage, which is crucial for preventing fluid accumulation under the graft and infection. Also, in Figure 4, we see the surgeon's hands carefully controlling the mesher, highlighting the attention to detail required during this process. The skin graft, after being meshed, will be applied to the recipient area and secured in place. The recipient area has been previously prepared through cleaning and debridement, ensuring that it is ready to receive the new skin. The skin mesher is positioned directly over the skin that appears to be harvested for transplant. This device will create regular cuts in the skin, transforming it into a network that can be stretched to cover a larger wound, thereby facilitating the healing process by allowing the drainage of fluids and encouraging the growth of new tissue. The skin around the work area appears to be unaffected, suggesting that this might be the donor area from where the skin graft is extracted. Typically, this skin is harvested from an area that can be hidden by clothing or that has a large surface area of excess skin, such as the inner thigh. The intense light and careful focus on the area of interest indicates the importance given to each step of the procedure. After the graft is applied, healing must be closely monitored. The patient will be instructed to take care of the transplanted area, avoiding trauma, and following a strict care protocol to ensure optimal recovery. This procedure can have a significant impact on the quality of life of patients, not only by restoring function and physical integrity, but also by improving aesthetic appearance and self-confidence, which is often just as important for long-term recovery (Figure 4).
In Figure 5, a post-operative medical procedure specific to reconstructive or plastic surgery is presented. A skin graft that has been applied and secured in place is observed; this is indicated by the presence of sutures and staples following the mesh lines of the graft, a technique that allows the expansion and adaptation of the graft to the size of the skin defect. The skin graft displays a characteristic mesh pattern, with numerous small cuts that facilitate the expansion of the tissue and improve healing by more efficiently integrating into the recipient area. Suturing techniques and the application of graft are essential for the success of the surgery, and their immediate post-operative appearance is often very different from what it will look like once healing is complete. Postoperative care for such a procedure will include monitoring for infection, pain management, and wound care to ensure the best possible healing (Figure 5).
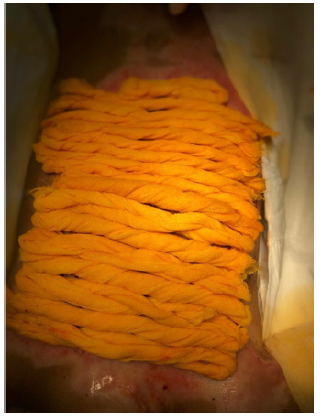
Finally, in Figure 6, the dressing is applied over the area where the recent surgical intervention site is located. The yellow dressing has been used to maintain uniform pressure on the treated tissue, to reduce swelling, and to promote healing. The edges of the area covered by the yellow dressing show small traces of blood, indicating that the surgical intervention was recent. The dressing itself does not show visible signs of bleeding, suggesting that its function is more for compression and stabilization rather than fluid absorption. The surgical procedure has concluded, and the patient is now in the recovery phase. This image reflects a critical and delicate stage in the healing process, emphasizing the importance of postoperative care in reconstructive surgery. Careful attention and regular evaluations are essential to ensure successful integration of the skin graft and to minimize the risk of complications such as infection or graft rejection (Figure 6).
Discussion
The correct technique for applying a Split-Thickness Skin Graft (STSG) includes careful preparation of the recipient site, ensuring that it is clean, free of infection, and well-vascularized. The graft is then harvested from the donor site and applied to the defect. In some cases, other methods may be used, such as full-thickness skin grafts, tissue flaps, or healing by secondary intention. The choice depends on the size and location of the defect, as well as the patient's overall health condition [4]. Meshed skin transplantation has demonstrated high efficiency in covering extensive skin lesions. The meshing technique allowed for the expansion of the graft and facilitated better adaptation to the contours of the wound. The meshed graft technique represents a significant innovation in reconstructive surgery, allowing for the expansion of the coverage area of autografts. Through this method, a special device called a dermatome is used to create uniform incisions in the graft, forming a mesh-like structure. These incisions allow the graft to stretch, so that a small piece of skin can be used to cover an area much larger than its original size [11]. After applying the meshed graft to the recipient area, the open spaces between the incisions are quickly populated through the migration and division of epithelial cells from the surrounding area. This process is called re-epithelialization and is crucial for wound healing. Although the initial spaces may seem large, the remarkable healing capacity of the skin allows these gaps to be covered over time, leaving behind surprisingly little scar tissue [12].
Meshed grafts are particularly useful for covering large surfaces of skin defects, such as those resulting from extensive burns or large excisions of necrotic or infected tissues. Since aesthetics are not paramount in such areas as the trunk or upper thighs, the functionality and effectiveness of the graft are prioritized [13]. One of the major advantages of meshed grafts is their ability to 'take' even on less ideal recipient sites. The free drainage of exudate through the graft incisions reduces the risk of fluid accumulation under the graft, which could otherwise interfere with its adherence and vascularization. Additionally, this technique allows for efficient exchange of oxygen and nutrients, essential for the survival of the graft [14]. However, meshed grafts can also have disadvantages. Their reticular structure may not be aesthetically pleasing, and therefore they are usually avoided in visually exposed areas, such as the face or hands. In addition, while re-epithelialization occurs rapidly, the final quality and texture of the repaired skin may not exactly match the surrounding tissue [15]. Thus, meshed grafts offer a valuable solution for treating extensive skin defects, being an essential component in the surgical arsenal for restoring function and protection in areas with large skin defects. Careful attention and post-operative monitoring are crucial for optimizing outcomes and minimizing complications.
In our study, the patient showed an improved rate of healing and integration of the graft, with consistent 'take' of the graft on the recipient area. The incidence of complications, such as infection or graft necrosis, was low, suggesting a favorable safety profile for this technique. No major adverse events directly related to the meshed skin transplantation procedure were reported. The healing process was accelerated in cases treated with meshed grafts, compared to traditional methods. The patient showed a significant reduction in complications, such as the formation of extensive scars or contractures, which are often associated with extensive skin lesions. Postoperative care protocols, including the application of compressive dressings and pain management, were effective in supporting healing and maintaining the integrity of the graft. The quality of life of the patients improved following the intervention, with a quicker return to normal activities and a decrease in discomfort.
Conclusions
The purpose of the research was to evaluate the effectiveness and safety of meshed skin transplant procedures and postoperative care in improving healing and reducing complications in patients with extensive skin injuries. The procedure of meshing skin grafts demonstrated an excellent ability to cover extensive wounds, allowing a significant expansion of the graft, which is essential in cases with a limited surface area of available donor skin. Meshing improved the flexibility of the graft and facilitated better conformity to the irregular contours of the recipient area. The patient showed an improved rate of healing and integration of the skin graft, suggesting that the techniques used in the study are suitable for optimizing the healing process. The graft 'take' was consistent and presented a low percentage of complications, such as infection or graft necrosis. Postoperative care, including the application of compressive dressings and pain management, was effective in maintaining the integrity of the graft and in patient comfort. The woven yellow textile compressive dressings provided not only adequate compression but also facilitated the visual inspection of the graft without disturbing the healing process. The functionality of the affected area improved following the skin transplant, with patients reporting a quicker return to daily and professional activities. The cost analysis of the treatment indicated that although the initial transplant procedure may be costly, its efficiency in promoting rapid healing and reducing the need for subsequent care made it cost-effective in the long term.
The study demonstrated that the meshed skin transplant procedure, along with a careful postoperative care strategy, represents an effective and safe approach in the management of extensive wounds. This approach should be considered standard practice in reconstructive surgery, with the potential to significantly improve outcomes for patients. The findings of the study contribute to the existing literature and provide a basis for improved practices and refined clinical guidelines. These discoveries and innovations have laid the foundations for modern skin graft surgery and paved the way for the development of the advanced techniques we have today. Skin grafting remains a vital component of reconstructive surgery and is essential in treating wounds, burns, and repairing surgical defects.
Acknowledgements
None.
Conflict of Interests
None.
References
- Petruzzelli GJ, Johnson JT (1994) Skin grafts. Otolaryngol Clin North Am 27(1): 25-37.
- Adams DC, Ramsey ML (2005) Grafts in dermatologic surgery: review and update on full- and split-thickness skin grafts, free cartilage grafts, and composite grafts. Dermatol Surg 31(8 Pt 2): 1055-1067.
- Higgins S, Wysong A (2019) Skin Grafts. In: Alam, M. (eds) Evidence-Based Procedural Dermatology. Springer Cham pp. 109-128.
- Taylor BC, Triplet JJ, Wells M (2021) Split-Thickness Skin Grafting: A Primer for Orthopaedic Surgeons. J Am Acad Orthop Surg 29(20): 855-861.
- Wolfe JR (1875) A new method of performing plastic operations. Br Med J 2(768): 360-361.
- Higgins S, Wysong A (2019) Skin Grafts. Evidence-Based Procedural Dermatology pp. 109-128.
- Cordoro KM, Russell MA (2005) Minimally invasive options for cutaneous defects: secondary intention healing, partial closure, and skin grafts. Facial Plast Surg Clin North Am 13(2): 215-230.
- De Gado F, Chiummariello S, Monarca C, Dessy LA, Rizzo MI, et al. (2008) Skin grafting: comparative evaluation of two dressing techniques in selected body areas. In vivo 22(4): 503-508.
- Greenstein G, Greenstein B, Cavallaro J, Elian N, Tarnow D (2009) Flap advancement: practical techniques to attain tension‐free primary closure. J Periodontol 80(1): 4-15.
- Valencia IC, Falabella AF, Eaglstein WH (2000) Skin grafting. Dermatol Clin 18(3): 521-532.
- Evans AJ (1971) Burns: Treatment of Burns Today. Proc R Soc Med 64(12): 1295-1296.
- Tarar MN, Mehmood F, Riaz A, Khan Z, Khalid K, et al. (2006) Transversely meshed skin grafting for aesthetically sensitive areas. Ann King Edw Med Univ 12(1): 124-126.
- Dai C, Shih S, Khachemoune A (2020) Skin substitutes for acute and chronic wound healing: an updated review. J Dermatolog Treat 31(6): 639-648.
- Chua AWC, Khoo YC, Tan BK, Tan KC, Foo CL, et al. (2016) Skin tissue engineering advances in severe burns: review and therapeutic applications. Burns Trauma 4: 3.
- Leon Villapalos J, Dziewulski P, Colwell AS (2021) Skin autografting.








 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.