Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Utilization of Breast Implant Tissue Expander for Hepatic Venous Outflow Obstruction Post Liver Transplant: A Case Report
*Corresponding author: Atta Nawabi MD, MBA, MPH professor of surgery, division of transplant and HPB The University of Kansas Medical Center, 3901 Rainbow Blvd, Kansas City, Kansas 66160, USA.
Received: June 06, 2024; Published: June 11, 2024
DOI: 10.34297/AJBSR.2024.22.003018
Abstract
Introduction: Liver transplantation is the mainstay treatment for End Stage Liver Disease (ESLD). Many post-operative complications can occur, one being Hepatic Venous Outflow Obstruction (HVOO). Different treatment strategies for HVOO include anastomotic revision, and stenting. We report the use of bio-compatible objects such as breast implants tissue expander in addition to the surgical revision to relieve the HVOO obstruction.
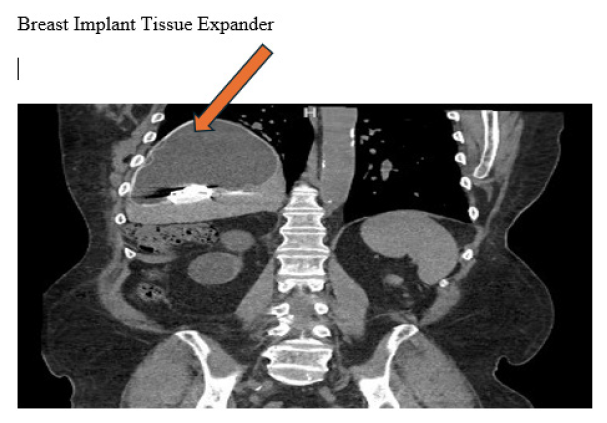
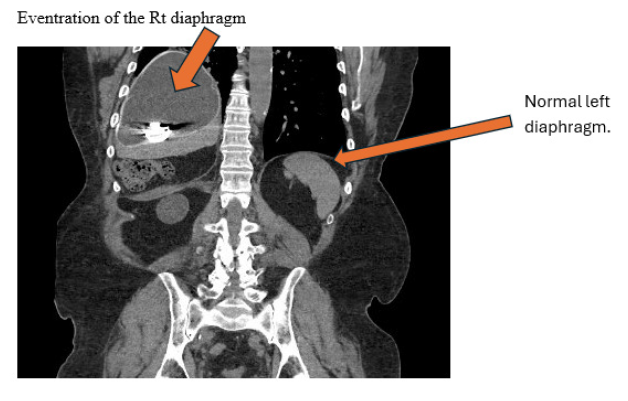
Presentation of Case: This is a 59-year-old male with ESLD secondary due nonalcoholic steatohepatitis, and eventration of right diaphragm due to phrenic nerve palsy figure 3. He underwent a liver transplant with piggyback technique. His post operative course was complicated by HVOO due to allograft rotating laterally, and cephalic toward the eventrated diaphragm figure 3. which required takeback to the operating room, where he underwent anastomotic revision and placement of a breast implant tissue expander to relieve HVOO. Following this he had markedly improved venous outflow. He progressed well and was able to eventually discharge home.
Discussion: The liver’s outflow is via the hepatic veins entering into the IVC and then taken back to the right atrium of the heart. Kinking at any level in this path can lead to outflow obstruction and congestion of the liver causing severe portal hypertension. In a post-transplant patient this poses an imminent threat to the graft lost, and poor outcome. if it occurs, must be addressed promptly. There are multitude of bio-compatible objects that can be used in order to help relieve HVOO.
Conclusions: Liver transplantation can be resulted in HVOO. Different types of tissue expanders, including breast implants, should be considered in post-transplant patients complicated with HVOO. Diligent follow-up is necessary for the diagnosis and treatment of patients following liver transplantation to assess graft viability and adequate blood flow.
Keywords: Breast implant, HVOO, Liver transplant, Eventration of the diaphragm
Introduction
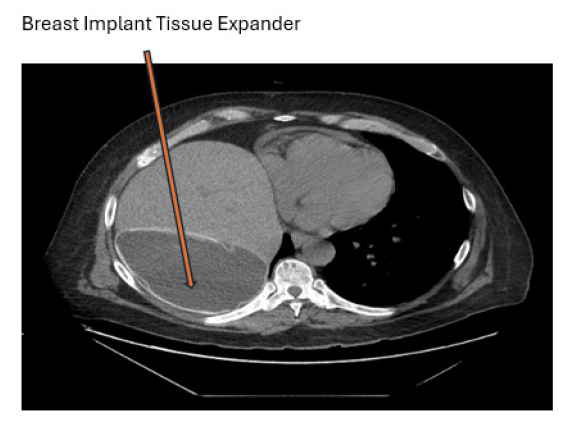
Liver transplantation is commonly used as a treatment for patients with end-stage liver disease due to the improvements in surgical technique, anesthesia, immunosuppression, and imaging [1]. Post-operative complications that could lead to graft failure are categorized into vascular, biliary, parenchymal, and malignant [2]. Malposition of the liver due to incorrect graft size can cause torsion of the venous anastomosis and lead to HVOO [3]. The incidence of HVOO after a standard or cava replacement liver transplant is <2%, but increases to 3-4% after a piggyback technique, and 5-13% when using a partial graft [2]. Although this complication is rare, surgical approach for revision of the anastomosis poses a significant risk for allograft lost and poor patient outcome [2]. Furthermore, literature in stent placement after an HVOO is limited. Several cases in the literature describe the use of bio-inert objects, such as breast implants or abdominal pads to improve anatomical mismatch, as they do not need to be removed [4]. This case describes the incorporation of a breast implant tissue expander to improve positioning and prevent kinking of the allograft (Figures 1-3).
Presentation of Case
A 59-year-old male with a history of ESLD secondary due Non-Alcoholic Steatohepatitis (NASH) was listed for orthotopic liver transplant with a MELD of 19. A donor organ became available. He underwent an orthotopic liver transplant with the ‘piggyback’ technique with duct-to-duct anastomosis. Following the completion of the operation, the patient’s liver enzymes continued to rise, doppler ultrasound was obtained which demonstrated poor flow visualized within the hepatic veins consistent with acute HVOO. He was emergently taken back to the operating room for revision of the supra hepatic vena cava anastomosis. upon entering the abdomen, the allograft appeared severely congested. At that point the hepatic artery and portal vein was excluded with the vascular clamp and the supra hepatic vena cava anastomosis was taken down and then performed side to side cavo-cavostomy anastomosis. Then the allograft was re perfused, good outflow and in flow were noticed. The patient tolerated reperfusion.
It was noticed that the patient has had right diaphragm eventration due to right phrenic palsy, figure 3. when position the allograft back into the right sub diaphragm, it made the allograft to rotate posteriorly and developed HVOO. The decision was made then to place 850cc breast implant tissue expander posterior to the allograft to allow the outflow to remain widely patent, and the allograft remains in normal position. Figure 1,2,3. Post operatively the patient progressed extremely well, and after a short stay in acute care rehab, he was able to discharge home.
He continued to be in excellent health from a liver standpoint even 10 years after his liver transplantation, and the breast implant remains in place.
Discussion
The liver receives 25% of the total cardiac output through the portal vein and hepatic artery. Blood is then drained from the acini via the central veins eventually into the hepatic veins, inferior vena cava, and right atrium. Blockage of blood flow from the liver can result in liver failure. HVOO is a serious complication to liver transplants that could affect the viability of the graft and put the patient in danger. It is divided into three categories based off the location of obstruction – at the level of sinusoids and terminal venules, Budd- Chiari syndrome, and venous obstruction [5]. Kinking of anastomosis due to differences in size between the graft and donor can result in HVOO. In this patient, it led to acute HVOO. The incorporation of bio-inert objects in addition surgical revision of the supra hepatic vena cava anastomosis is increasingly popular. In the context of this case, a breast implant tissue expander was placed posterior to the allograft to prevent kinking due to the patient known history of right phrenic palsy and eventration of the right diaphragm. Other options noticed in the literature include mesh, abdominal pads, inflatable materials, and surgical gloves.
Conclusion
Although the incidence of HVOO post liver transplantation remains low, it is a devastating complication that potentially cause patient and allograft loss. Prompt diagnosis and treatment is required to save the allograft and patient. Surgical revision of the anastomosis remains the main option. Utilization of the Breast implants tissue expander or any other bio medical compatible objects are served as a potential option given their bio-inert nature and known safety in patients. They are readily available at the large hospital systems and should be considered when addressing HVOO that is not improved with anastomotic revision alone. Diligent follow-up is necessary for the diagnosis and treatment of patients following liver transplantation to assess hepatic viability and adequate blood flow.
References
- Mera S, Santoyo J, Suárez MA, Bondía JA, Cabello, et al. (1999) Use of the breast implant for liver graft malposition. Liver Transplantation and Surgery 5(6): 534-535.
- Gastaca M, Valdivieso A, Ruiz P, Gonzalez J, Ventoso A, et al. (2011) Venous outflow obstruction after orthotopic liver transplantation: use of a breast implant to maintain graft position. Clinical Transplantation 25(3): E320-E326.
- Pérez Sánchez LE, Orti Rodríguez RJ, Reyes Correa B, Moneva Arce E, Barrera Gómez MÁ (2020) Breast implant during orthotopic liver transplant to avoid hepatic outflow obstruction. Acta Chir Belg 120(2):146-147.
- Chetana Lim, Michael Osseis, Antonella Tudisco, Eylon Lahat, Dobromir Sotirov, et al. (2018) Hepatic venous outflow obstruction after whole liver transplantation of large-for-size graft: versatile intra-operative management. Ann Hepatobiliary Pancreat Surg 22(4): 321-325.
- Bayraktar UD, Seren S, Bayraktar Y (2007) Hepatic venous outflow obstruction: Three similar syndromes. World J Gastroenterol 13(13): 1912-1927.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.