Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
A-55-Years-Old Chronic Smoker Presented with Right Upper Limb Ischemia, Septicemia, Acute Kidney Injury, Acute Liver Injury, Acute Superior Mesenteric Artery Occlusion and Colonic Ischemia: Rare Case Report
*Corresponding author: Khin Phyu Pyar, Professor and Head/ Senior Consultant Physician, Department of Medicine/Department of Nephrology, Defence Services Medical Academy/No. (1) Defence Services General Hospital (1000-Bedded), Myanmar.
Received: July 11, 2024; Published: July 16, 2024
DOI: 10.34297/AJBSR.2024.23.003059
Summary
55-years-old chronic smoker had acute, severe pain in the right forearm for one week. He underwent below elbow amputation of left upper limb for acute limb ischemia one year ago. Axillary, brachial and radial pulses were not palpable. The skin was cold discolored and tender up to mid-arm on right side. Weakness of movement of elbow joint and sensation were noted. CT angiogram revealed complete occlusion of subclavian artery downwards on both sides. Parenteral heparin and antibiotics were given. Above elbow amputation was done; there was no active bleeding at brachial artery. Thrombosis was noted along brachial artery. Moreover, the color of muscle was brownish and consistency was soft and flabby. It was complicated by sepsis, DIC, acute kidney injury and acute liver injury. Bone shortening of amputated stump was done on Day ‘6’. The patient had sudden onset of severe chest pain during hemodialysis on Day ‘12’; it was briefly followed by sudden death. Autopsy revealed acute thrombus in superior mesenteric artery with acute gangrene of colon; coronary ostia were patent. Pain from acute superior mesenteric artery occlusion was referred to precordium and it mimicked acute coronary syndrome.
Keywords: Chronic smoker, Upper limb ischemia, Septicemia, Acute kidney injury, Acute liver injury, Superior mesenteric artery occlusion, Colonic ischemia
Introduction
Acute arterial occlusion is same as acute limb ischemia. It is one of vascular emergency. Acute limb ischemia is a sudden loss of limb perfusion for up to 2 weeks after an inciting event. Acute arterial occlusion can occur in any peripheral artery of the upper and lower extremities; it may occur in carotids, coronary and visceral arteries. The incidence of acute peripheral arterial occlusion causing acute lower extremity ischemia is approximately 1.5 cases per 10,000 persons per year [1]; the prevalence rises with age. Epidemiological studies indicate that up to 5% of men and 2.5% of women 60 years of age or older have symptoms of intermittent claudication [2]. Risk factors include age, smoking, diabetes, obesity, sedentary lifestyle, family history of vascular disease, high cholesterol, and high blood pressure. Non-traumatic ischemia of the lower extremities is more common than the upper extremities and is more likely to result in limb loss. The management of acute ischemia includes surgical or catheter-based thromboembolectomy, bypass grafting, thrombolytic therapy, endovascular revascularization and percutaneous transluminal angioplasty [3-8]. The morbidity, mortality, and limb loss rates from acute lower extremity ischemia remain high [9]. Therefore, early diagnosis and rapid initiation of therapy are essential to provide the best chance for limb salvage [10]. There were several reports on arterial thromboembolic events; some were related with COVID-19 infection [11,12] (Unexpected Arterial Thrombosis and Acute Limb Ischemia in a Young Male Patient with COVID-19: A Case Report, n.d.) [13]. This case report was not related with COVID-19 infection.
Case Presentation
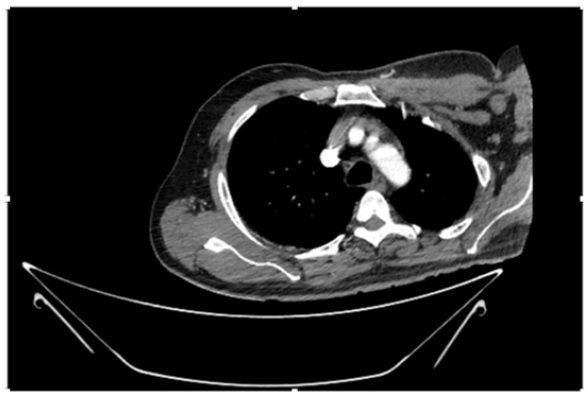
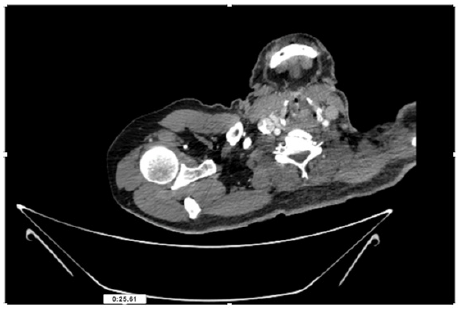
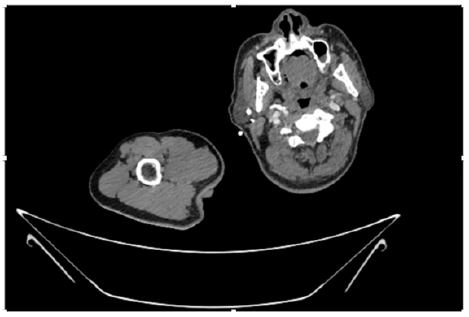
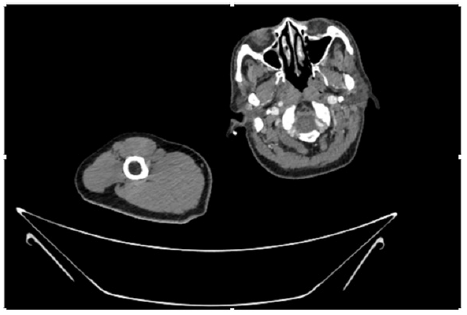
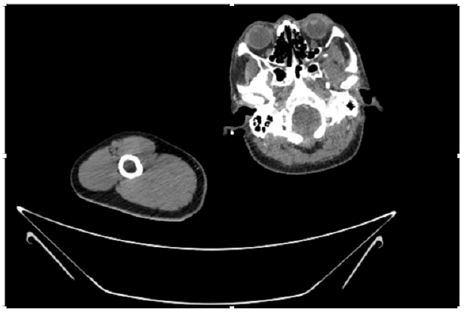
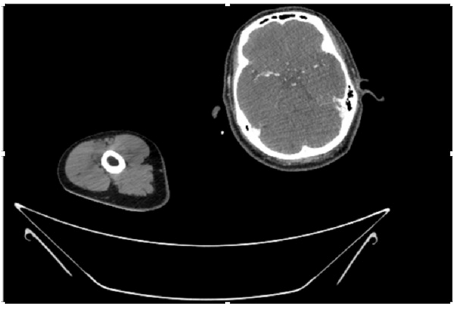
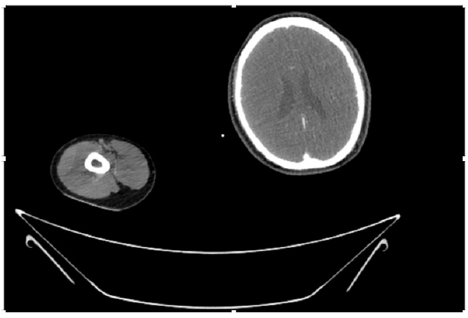
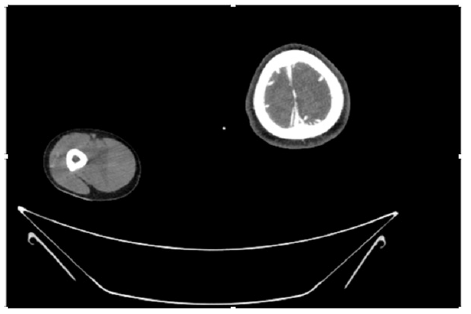
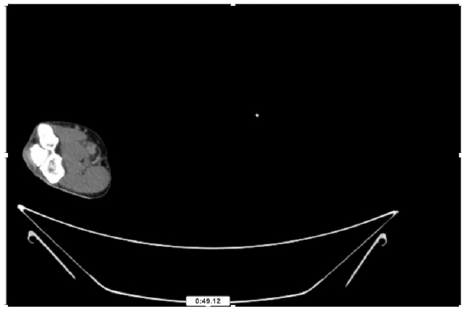
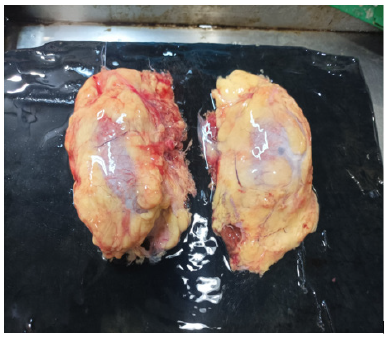
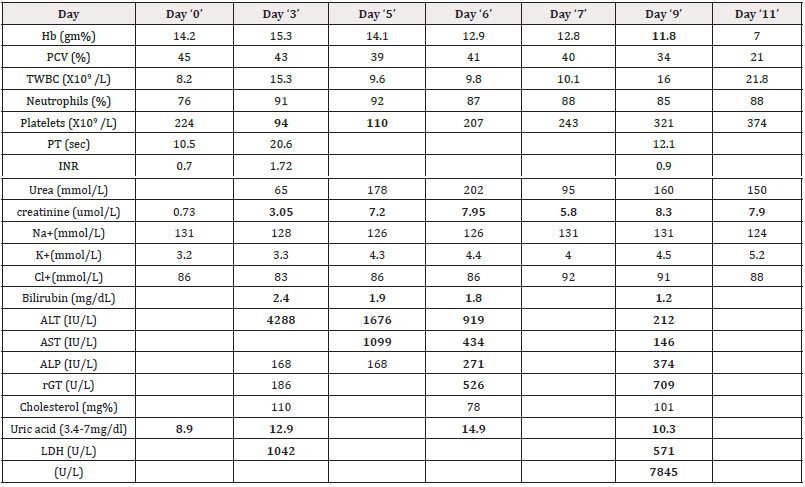
55-years-old chronic smoker had acute, severe pain in the right upper limb for one week; it was cold upto mid arm with skin discoloration. He also noticed numbness and weakness of movement of elbow joint. He underwent below elbow amputation in February 2023 for acute ischemia of left upper limb. He was a current chronic smoker; 15 pack year. General condition was weak; temperature was normal; blood pressure was 100/60mmHg; heart rate was 92/minutes with sinus rhythm; SpO2 was 97% on air; heart was normal. In lower extremities, all peripheral pulses were intact. Local Examination of right upper limb revealed as follows: tenderness; coldness; discoloration; decreased motor function and sensory modalities. Axillary, brachial and radial pulses were not palpable. Hand-held Doppler failed to detect any signal in arterial system; therefore, we arranged for emergency embolectomy. complete occlusion of right upper limb arterial system Full blood count showed high hemoglobin (14.6gm%); normal total WBC and platelet count. Coagulation profile was normal. Parenteral unfractionated heparin, antibiotics, tramadol, proton-pump inhibitors, anti-platelets and HMG CoA reductase inhibitors were given. Doppler ultrasound demonstrated complete occlusion of right upper limb arterial system. CT Angiogram illustrated occlusion of subclavian artery downwards on both sides. Figures 1-14 shows complete occlusion of right subclavian artery without collaterals. On Day ‘2’ of admission, the patient passed black tarry stool for 3 times. However, the vital signs were stable; blood pressure was 100/60mmHg; heart rate was 92/min; SpO2 was 97% on air; the abdomen was soft and not tender. Above elbow amputation was done on Day ‘2’ of admission. Intra-operative findings were as follows: (1) no active bleeding at brachial artery; (2) thrombosis along brachial artery; (3) muscle color and consistency were not healthy.
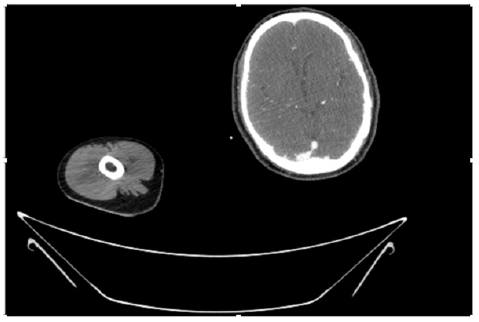
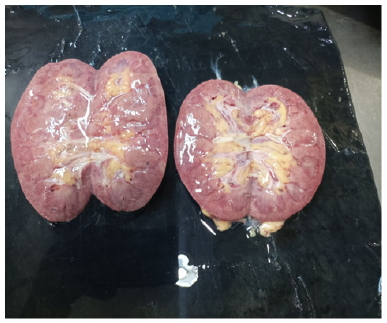
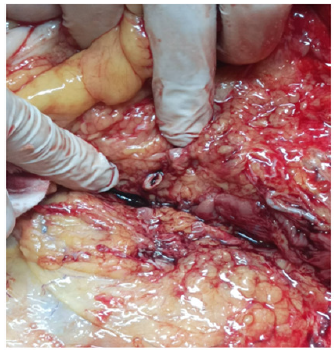
Then, the condition deteriorated rapidly; temperature 100˚F; the patient became oliguric; and, serum creatinine rose. Nephrologist opinion was Stage III AKI with sepsis and DIC; the renal team arranged for hemodialysis. Moreover, the patient had acute liver injury; he became jaundiced; serum bilirubin rose; and, ALT was more than 100 times normal (4289IU/L). Evidence of sepsis, DIC and acute kidney injury became more evident; neutrophil leukocytosis (total WBC 15x109/L); platelets dropped to 94x109/L; and, serum creatinine was 3.2mg%. Furthermore, the amputated wound was unhealthy; the color changed to brownish; it was having foul smelling discharge without active bleeding. Transthoracic echocardiogram showed dilated left atrium and left ventricle; LVEF was 48%; mild mitral regurgitation; and, no clot. Blood culture revealed Staphyloccus Capitis; sensitive to Gentamycin, oxacillin, ciprofloxacin, ceftriaxone, meropenum. Therefore, on Day ‘6’ bone shortening of amputated stump was done by orthopedic surgeon; escalation of antibiotics was done. The overall condition was poor. On Day ‘12’, during 4th time hemodialysis, the patient had severe chest pain, dyspnea and sweeting; BP was 170/149mmHg; pulse rate was 120/minutes; SpO2 was not measurable; sudden cardiac arrest. There was no response to active resuscitation. As it happened suddenly within 5 minutes, ECG recording was not done. The clinical impression was either acute coronary syndrome or pulmonary embolism. In autopsy, coronary ostia were normal; no occlusion. It is shown in Figures 15-17 reveal acute kidney injury, normal size kidneys with normal cortex and medulla. Figure 18 demonstrates occlusion of superior mesenteric artery with thrombus; Figure 19 illustrates dis-colored caecum as a result of ischemia. Figure 20 reveals slightly enlarged liver with congestion compatible with acute liver injury. Figure 21 shows tar staining of both lungs. Figure 22 is the amputated stamp on right mid-arm; the color of muscle is brownish. There was no evidence of pulmonary embolism (Figures 23-28) (Table 1).
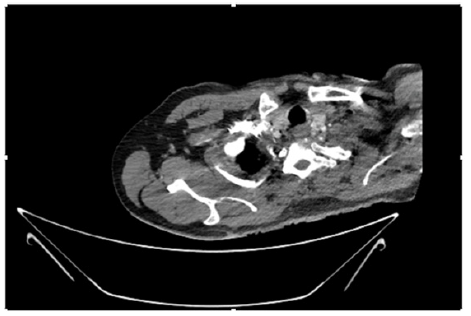
Figure 4: CT Angiogram at neck showing normal brachio-cephalic trunk, common carotid artery, and narrow right subclavian artery.
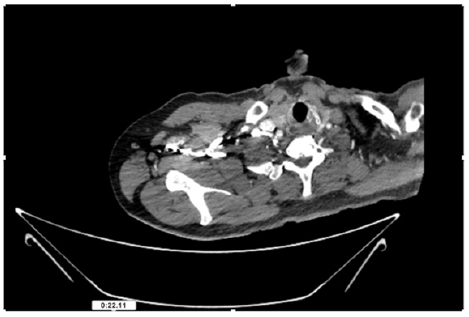
Figure 5: CT Angiogram at neck showing normal brachio-cephalic trunk, common carotid artery, and narrow right subclavian artery.
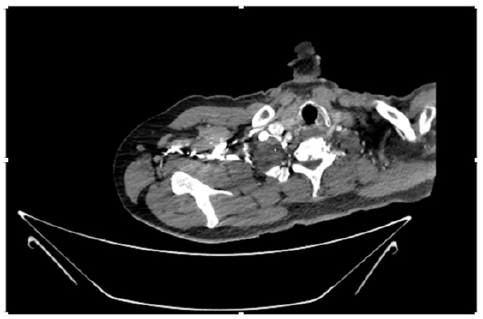
Figure 6: CT Angiogram at neck showing brachio-cephalic trunk, common carotid artery and narrow right subclavian artery.
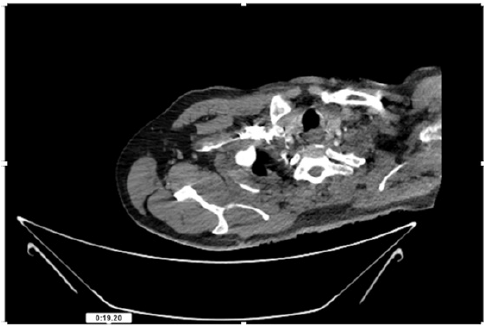
Figure 7: CT Angiogram at neck showing brachio-cephalic trunk, common carotid artery and narrow right subclavian artery.
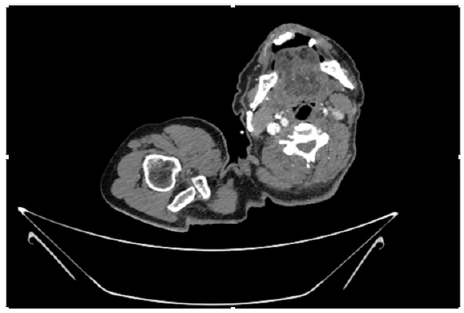
Figure 10: CT Angiogram at upper arm showing totally occluded right axillary artery; normal internal carotid artery and external carotid artery.

Figure 24: Autopsy of lower abdomen showing discoloration of caecum, sequelae of occlusion of superior mesenteric artery.
Discussion
This patient had history of acute limb ischemia of left upper limb for which he underwent below elbow amputation one year ago. Present problem was again for acute limb ischemia of right upper limb. The risk factor for thrombosis was chronic heavy smoking and the old age-55 years. His blood pressure was normal; blood cholesterol level was normal too. This patient had modifiable risk factor i.e smoking. If the patient quit smoking, he would not face the problem of ischemia on right upper limb. It indicates that we need to upgrade ‘smoking cessation program’. Non-traumatic ischemia of the lower extremities is more common than the upper extremities and is more likely to result in limb loss [14,2]. In this patient, the reverse was happening; there was no history of trauma. This is one reason for case reporting. The incidence of acute peripheral arterial occlusion causing acute lower extremity ischemia is approximately 1.5 cases per 10,000 persons per year [1]; the prevalence rises with age [2]. This patient was only 55 years old; the median age prevalence of atherosclerosis in UK was 75 years. We should aware of prevalence of premature atherosclerosis in Myanmar.
The management of acute limb ischemia is advancing; it includes surgical or catheter-based thromboembolectomy, bypass grafting, thrombolytic therapy, endovascular revascularization and percutaneous transluminal angioplasty [3-8]. Nonetheless, the morbidity, mortality, and limb loss rates remain high [9]. For limb salvage, early diagnosis and rapid initiation of therapy are essential [10]. This patient had early diagnosis and received medical treatment (heparin, antiplatelets and lipid lowering agents) as well as surgery timely. Because of ongoing ischemia even after above elbow amputation, the wound was not healthy. And it was added by infection and multi-organ failure; sepsis, DIC, acute kidney injury, and, acute liver injury. The subclavian artery was totally thrombosed; however, we did not have facility for endovascular revascularization. He would have survived if we had done disarticulation of shoulder joint. Takeuchi et al mentioned one case where they did disarticulation of hip joint in view of severity of ischemia and irreversible limb paralysis in acute ischemia of lower limb in patient with COVID-19 infection [15]. The patient had sudden onset of severe chest pain during hemodialysis followed by sudden death. Patency of coronary ostia, normal myocardium and having thrombus in superior mesenteric artery in autopsy indicated that the pain from acute superior mesenteric artery occlusion was referred to precordium as chest pain; mimicking either acute coronary syndrome or massive pulmonary embolism. There were features of acute gangrene of colon in autopsy. Blood supply of colon was from superior mesenteric artery; therefore, it was the sequelae of occlusion of superior mesenteric artery. Atherosclerosis is a multisystem disorder; there may be simultaneous involvement of median and small arteries. It is important to have awareness on multiorgan involvement in atherosclerosis. This case highlighted generalized atherosclerosis; limb and viscera.
COVID-19 is associated with high risk of thrombotic complications. There were several reports on patients with COVID-19 infection having arterial thromboembolic events [11,12] (Unexpected Arterial Thrombosis and Acute Limb Ischemia in a Young Male Patient with COVID-19: A Case Report, n.d.) [13]. In the study by [16], patients with COVID-19 infection were diagnosed by doing IgG and IgM level by immunochromatographic method; their patients had combined ischemia of limb, intercostal arteries and superior mesenteric artery. Blood IgG or IgM of SARSCov-2 indicate chronic infection and acute infection respectively. This patient did not show nasopharyngeal swab for PCR of SARSCov-2; therefore, he did not have acute COVID-19 infection. However, we could not test blood level of IgG or IgM of SARSCov-2. In COVID-19 era, he might have positive IgG of SARSCov-2 which could aggravate thrombosis. Acute mesenteric ischemia is a group of diseases characterized by an interruption of the blood supply to varying portions of the intestine, leading to ischemia and secondary inflammatory changes. If untreated, this process may progress to life-threatening intestinal necrosis. The incidence of acute mesenteric ischemia is low; 0.09-0.2% of all acute surgical admissions. However, its prevalence increases with age. This patient was not old; 55 years. It is one reasons for case reporting. Although acute mesenteric ischemia is an uncommon cause of abdominal pain, awareness is extremely important. Because the mortality is 50% if untreated [17] (Trends in Population-Based Incidence, Diagnostics, and Mortality of Acute Superior Mesenteric Artery Occlusion, n.d.) [18-24]. Physicians should consider acute mesenteric ischemia if the patient has severe abdominal pain particularly in those with COVID-19 infection [25]. Therefore, we should have awareness on mesenteric ischemia in COVID-19 era. In this patient, acute severe chest pain was referred pain from mesenteric artery occlusion; and, cardiac arrest was within very short period. This case report was a good example for causes of severe chest pain referred from abdomen [26-28].
Conclusion
Acute ischemia of upper limb is not uncommon particularly in COVID-19 era and it is surgical emergency. It has very high morbidity and mortality. It should be managed by multidisciplinary team including vascular surgeon, orthopedic surgeon, interventional radiologist, general physicians, nephrologist, hematologist, intensive care physician and hepatologist. Simultaneous ischemia of other median size and small arteries causing chest pain or acute abdomen may give rise to another medical or surgical emergency. Smoking is a modifiable risk factor for atherosclerosis and smoking cessation program should be encouraged.
Statement of Informed Consent
Informed consent was also taken from the relatives of patient.
Acknowledgments
The authors would like to thank the patient and family members for giving informed consent. The authors also acknowledged Prof. Ko Ko Lwin, Prof. Kyaw Zay Ya, Prof. Myint Zaw and Prof. Thet Naing for administrative support, Prof. Yu Aye Latt for intensive care, Prof. Tin Moe Mya for laboratory support and Prof. Kyaw Zin Nyunt for orthopedic care.
Disclosure of Conflict of Interest
The authors declared no potential conflicts of interests with respect to authorship and publication of this article.
References
- Creager MA, Kaufman JA, Conte MS (2012) Clinical practice. Acute limb ischemia. N Eng J Med 366(23): 2198-2206.
- Weitz JI, Byrne J, Clagett GP, Farkouh ME, Porter JM, et al. (1996) Diagnosis and Treatment of Chronic Arterial Insufficiency of the Lower Extremities: A Critical Review. Circulation 94(11): 3026-3049.
- Shoji K, Zen K, Yanishi K, Wakana N, Nakanishi N, et al. (2020) Two effective cases of additional pedal artery angioplasty for severe lower limb ischemia following acute thrombotic artery occlusion with hypercoagulable state diseases. CVIR Endovasc 3(1): 71.
- Kokkinidis DG, Schizas D, Pargaonkar S, Karamanis D, Mylonas KS, et al. (2023) Differences between Lower Extremity Arterial Occlusion vs. Stenosis and Predictors of Successful Endovascular Interventions. Medicina 59(11): 2029.
- Simon E, Kovacs M (2015) Acute bilateral lower extremity arterial occlusion without risk factors or embolic source. Am J Emerg Med 34(4): 762.e3-4.
- Olinic DM, Stanek A, Tătaru DA, Homorodean C, Olinic M (2019) Acute Limb Ischemia: An Update on Diagnosis and Management. J Clin Med 8(8): 1215.
- Hynes BG, Margey RJ, Ruggiero N, Kiernan TJ, Rosenfield K, Jaff M, et al. (2012) Endovascular management of acute limb ischemia. Annals of Vascular Surgery 26(1): 110-124.
- Kashyap VS, Gilani R, Bena JF, Bannazadeh M, Sarac TP (2011) Endovascular therapy for acute limb ischemia. Journal of Vascular Surgery, 53(2): 340-346.
- Baril DT, Patel VI, Judelson DR, Goodney PP, McPhee JT, et al. (2013) Outcomes of lower extremity bypass performed for acute limb ischemia. J Vasc Surg 58(4): 949-956.
- Obara H, Matsubara K, Kitagawa Y (2018) Acute Limb Ischemia. Annals of Vascular Diseases 11(4): 443-448.
- Nguyen A, Al Hage A, Yu H, Gunaga S (2022) Arterial Occlusion and Acute Deep Vein Thrombosis-Induced Acute Limb Ischemia in a COVID-19 Patient. Cureus 14(7): e26689.
- Costa V de O, de Almeida GBC, Nicolini EM, Rodrigues G de A, da Costa BMA, et al. (2020) Acute arterial occlusion of the lower limb as the main clinical manifestation in a patient with Covid-19–Case Report. Int J Surg Case Rep 77: 454-458.
- Nowroozpoor A, Bank MA, Jafari D (2021) Limb Ischemia due to Extensive Arterial Thrombosis in the Absence of Venous Occlusion as an Unusual Complication of Critical Illness from COVID-19. Case Reports in Acute Medicine 4(1): 23-31.
- AlMadhwahi N, Al Hanash S, Barat A, Alshujaa M, Najran M, et al. (2024) Acute limb ischemia due to left brachial artery occlusion in a 40-year-old female patient: A case report. Emergency Care Journal, 20(1).
- Takeuchi H, Tsukamoto Y, Kato R, Mitsuzawa S, Yamashita S, et al. (2024) Acute total occlusion of the common femoral artery as a consequence of COVID-19 pneumonia resulting in hip joint disarticulation: Report of an unusual case. JOS Case Reports 3(1): 1-5.
- Costa V de O, de Almeida GBC, Nicolini EM, Rodrigues G de A, da Costa BMA, et al. (2020) Acute arterial occlusion of the lower limb as the main clinical manifestation in a patient with Covid-19-Case Report. Int J Surg Case Rep 77: 454-458.
- Bala M, Catena F, Kashuk J, De Simone B, Gomes CA, et al. (2022) Acute mesenteric ischemia: Updated guidelines of the World Society of Emergency Surgery. World J Emerg Surg 17(1): 54.
- Liao G, Chen S, Cao H, Wang W, Gao Q (2019) Review: Acute superior mesenteric artery embolism: A vascular emergency cannot be ignored by physicians. Medicine 98(6): e14446.
- Jagielski M, Piątkowski J, Jackowski M (2020) Challenges Encountered during the Treatment of Acute Mesenteric Ischemia. Gastroenterol Res Pract 2020: 5316849.
- Kadri Tamme, Annika Reintam Blaser, Kaja Triin Laisaar, Merli Mändul, Jaak Kals, et al. (2022) Incidence and outcomes of acute mesenteric ischaemia: A systematic review and meta-analysis. BMJ Open 12(10): e062846.
- Bala M, Kashuk J, Moore EE, Kluger Y, Biffl W, et al. (2017) Acute mesenteric ischemia: Guidelines of the World Society of Emergency Surgery. World J Emerg Surg 12(1): 38.
- Björnsson S, Björck M, Block T, Resch T, Acosta S (2011) Thrombolysis for acute occlusion of the superior mesenteric artery. J Vasc Surg 54(6): 1734–1742.
- Wu MY, Lee LC, Chen YL, Chien YC, Ni BY, Hou YT, et al. (2018) Ischemic Bowel Disease Due to Superior Mesenteric Artery Occlusion: A Case Report. Reports 1(1).
- Agrawal S, Singh K, Dhruv K, Kanwar K (2019) Superior Mesenteric Artery Occlusion: A case report and mini Review. International Journal of Medical Reviews and Case Reports 3(7): 1.
- Sukegawa M, Nishiwada S, Terai T, Kuge H, Koyama F, et al. (2022) Acute superior mesenteric artery occlusion associated with COVID-19 pneumonia: A case report. Surg Case Rep 8(1): 6.
- Y Soltanzadeh Naderi, S Acosta (2024) Trends in population-based incidence, diagnostics, and mortality of acute superior mesenteric artery occlusion. Front Surg 10: 1334655.
- Badr Aljabri, Mohammed Yousef Aldossary (2023) Unexpected arterial thrombosis and acute limb ischemia in a young male patient with COVID-19: A case report. Front Surg 10: 1092287.
- Weitz JI, Byrne J, Clagett GP, Farkouh ME, Porter JM, et al. (1996) Diagnosis and Treatment of Chronic Arterial Insufficiency of the Lower Extremities: A Critical Review. Circulation 94(11): 3026-3049.





.png)
.png)
.png)
.png)
.png)
.png)




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.