Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
A Patient-Centred Supportive Care Management Program Reduces Acute Events in Patients with Heart Failure and Diabetes Mellitus: A Sub-Analysis of ‘SupportHeart’ Study
*Corresponding author: Katerina Philippou, Special Teaching Staff, School of Health Sciences, Department of Nursing, Cyprus University of Technology, 15, Vragadinou Str, 3041, Limassol, Cyprus.
Received: June 28, 2024; Published: July 05, 2024
DOI: 10.34297/AJBSR.2024.23.003048
Abstract
Introduction: New effective approaches are necessary for improving the care and complications in patients with Heart Failure (HF) and Diabetes Mellitus (DM) who must deal everyday with various complex factors.
Aim: The aim of the current study was to evaluate the effectiveness of an individualized supportive care management program in patients with HF and DM, in the reduction of acute events and mortality compared to the ‘usual’ care.
Methodology: The current study is a sub-analysis of the Randomized Clinical Trial (RCT) named ‘SupportHeart’ using pragmatic methodology consisted by the Intervention Group (IG) and the Control Group (CG). The study investigated the patients for a period of one year at 5 different time points. Welsch t-test when the variables were continuous and the Fisher’s exact test in the case of categorical variables were used. Linear Mixed Models Effects were performed and adjusted by various factors related to the participants.
Results: The sample consisted of 121 patients with HF and DM. Survival analysis was studied categorizing it, into acute events and death events due to HF. At the period from recruitment to 1 month, there were 3/65 (4.6 %) acute events for the CG and 2/56 (3.6%) acute events for the IG p>0.9. After 1 month and until 3 months’ time point after the intervention, the CG 7/64 (10.9%) had more acute events compared to the IG 3/56 (5.4%) p=0.51. After 3 months and until the 6-month time point after the intervention, the CG 12/61 (19.7%) had more acute events compared to the IG 6/52 (11.5%) p=0.3. Between 6 months and until 1 year time point after the intervention, the IG (0/49) (0.0%) hadn’t any acute event compared to the CG that had 8/58 (13.8%) p=0.007 acute events. There were no significant differences in the mortality across the two groups in all time points; at the period from recruitment to 1 month, there was 1/ 65 (1.5%) death event for the CG and no death for the IG 0/56 (0.0%) p>0.9. After 1 month and until 3 months’ time point after the intervention, the CG had 2/64 (3.1 %) deaths and the IG 3/56 (5.4%) p=0.66. After 3 months and until the 6-month time point after the intervention, the CG had 3/61 (4.9%) deaths compared with the IG that had 1/52 (1.9%) death p=0.62. Between 6 months and until 1 year time point after the intervention, the CG had 1/58 (1.7%) death event and the IG had 1/49 (2.0%) with p>0.9.
Conclusions: Supportive care seems to be a promising concept for HF-DM management programs. The pragmatic methodology that was used in the ‘SupportHeart’ study had an intensive intervention, started rapidly in early stages on a person-centred basis, reduced acute events and deaths in patients with HF and DM.
Keywords: Supportive care, heart failure, diabetes mellitus, person-centred care, acute events, heart failure-diabetes mellitus management programs
Introduction
There are more than 415 million people with DM globally nowadays and is expected that, more than 592 million people will develop diabetes by the year 2035 [1]. It is considered that between HF patients, the prevalence of DM is 2 to 2.5 times higher than in the general population [2]. Many clinical studies show that Diabetes Mellitus type II (DM2) breed HF and vice versa [3]. Observational studies in HF with DM found that there is a strong relationship between glycemic control and clinical outcomes that affect negatively the Health-Related Quality Of Life (HR-QoL) of these patients [4-6]. Despite the progress in the treatment and in the various programs which are applied for the management of HF, HF deteriorations lead to readmissions and the morbidity and mortality of HF patients are increased, especially in older patients with the comorbidity of DM [7]. Adherence and management of the two conditions by patients with HF and DM to follow a low- sodium diet, monitor weight, daily fluid volume, breath more effectively such as follow coughing techniques, quit smoking, manage fatigue, manage normal glucose levels, coping with stress, follow medication adherence, be physical active, socialize, manage relax and early detection of decompensation signs, are difficult [8]. Most of the times, patients’ education only is not effective for the development of self-care skills in patients with HF and DM in order to manage their condition in their everyday living and more effective ways of coping are fundamental to be applied and learned in the management programs [9,10]. ‘SupportHeart’ study is a management program based on supportive care and focused on a patient-centred approach using the pragmatic methodology, that integrates patient preferences and needs into the goals of care, manages symptoms to the level of comfort desired, and attempts to reduce the burden of the diseases [8]. Supportive care is a multidisciplinary holistic care provided in both the patient and his family, since the time of the diagnosis along with the treatment aiming to prolong life and into the end of life with palliative care [11-13].
Methods
Study Design
The purpose of the current study was to evaluate the effectiveness of an individualized supportive care management program in patients with HF and DM, in order to improve acute events (readmissions and emergency room visits) and mortality of the patients, compared to the ‘usual’ care. This study is a sub-analysis of the Randomized Clinical Trial (RCT) –‘SupportHeart’ (Trial ID: NCT04415723) using pragmatic methodology. It was consisted by two groups: 1. The IG and 2. The CG. The study investigated the patients for a period of 1 year at 5 time points (in baseline, 1 month, 3 months, 6 months, and 1 year). The CG received the ‘usual care.’ ‘Usual care’ was defined as the actions that each hospital or health care setting follows for all patients before their discharge from the hospital/their personal doctor that includes general advice on managing HF and DM. The IG received the supportive care management program developed, according to the themes arrived from the qualitative analysis of the focus groups which preceded for the design of the intervention (e.g monthly meetings, education, self-management techniques, telephone support, SMS, etc.). The follow up period was twelve months as this was considered a sufficient timeframe to observe the effectiveness of the supportive program to achieve the goals of the ‘SupportHeart’ research program.
Study Population
The sample of the study consisted of patients from hospitals, patients who are included and receive services from the new National Health System of Cyprus and patients from the Pancyprian Federation of Heart Diseases, diagnosed with HF established by a cardiologist with the comorbidity of DM. In the RCT ‘SupportHeart’ the sample size consisted of 202 patients in total, from which the 121 patients were those with HF and DM.
Inclusion Criteria were as Follows: patients over 18 years old diagnosed with HF and DM based on systolic or diastolic dysfunction as diagnosed by a cardiologist, patients with New York Heart Association (NYHA) classification stages I-IV and patients able to understand write and read the Greek language. The patients who excluded from the study were patients who refused to take part in the research, patients diagnosed with any kind of mental illness including dementia, patients under hemodialysis, patients with whom telephone communication is not applicable, patients not speaking the Greek language and patients transfer to a nursing home after discharge.
Randomization and Blinding
All participants of the RCT ‘SupportHeart’ were randomized to receive either the intervention care or the usual care, with a ration 2:1 using the sealed envelope technique by using random number generator. A member of the research team who did not participated in the recruitment of the sample did the random distribution for the ‘SupportHeart’ of the participants in the two groups. The random allocation was developed with the use of a software program. The researcher was blinded regarding the group allocation of the next patient so the prediction of the selection bias achieved by using closed envelops for the recruitment because the researcher opened the envelops after the patient agreed to participate in the research and signed the informed consent form. ‘Double blinding’ could not be achieved because patients informed before signing the consent form to participate in the research. So, after opening the envelope, both; the patient and the researcher were aware in which group the patient were.
Sample Size
The method of power analysis is used to determine the sample size. Power analysis is the ability to find a statistically significant difference when the null hypothesis is in fact false. In other words, power is the ability to find a difference when a real difference exists. It is determined by three factors: the sample size, the alpha level, and the effect size [14]. In the current study, researchers wanted to determine the appropriate sample size or justify a proposed sample size. To answer this question, researchers found out the other two parts of the equation: alpha level and effect size [14]. In the RCT with the acronym, ‘SupportHeart’ the sample size consisted of 202 patients in total from which the 121 patients were those with HF and DM.
Ethics Approval
The participants signed an informed consent form where a detail description of the study was presented. It included the aim of the study, what was expected of them and the reasons why this study is important. Written informed consent was obtained from the participants at the beginning of the study ensuring anonymity and confidentiality. The study had a voluntary nature that allowed the patients to withdraw at any time. The anonymity of the participants was respected throughout the study. The study granted approval by the Cyprus Bioethics Committee and by the Data Protection Office. In addition, license was sought and granted, by the Scientific Committee for the Promotion of Research and the Ministry of Health of Cyprus.
The Intervention
Patients with HF and DM were invited to participate in the study by a member of the research team, just before their discharge or from the outpatients’ clinics. Patients were informed for the context of the research and if they agreed to participate in the study, they signed a consent form. Data collection was conducted by the researchers of the ‘SupportHeart’ team, during the monthly meetings or by phone. They used questionnaires and a guide that were pre-decided by the research team. The monthly meeting points and the main topic were determined by the research team. Beyond that, questions from the patients were resolved and there was also a discussion on other topics patients wanted to discuss and according to their needs. The current intervention program was based in pragmatic research methodology as referred above and it was not standardized and the same for all the patients but was planned and delivered according to patients’ needs at the meetings. In pragmatic studies an intensive intervention and treatment strategy of rapid-titration and close follow up is rapidly accepted by patients [15].
The patients in the IG received an educational booklet material and a brief educational session by the researcher in the bedside before their discharge for hospitalized patients and right from the beginning for non - hospitalized patients. Then, the researcher was contacting via telephone the patients 48 hours after the first meeting, to find out how they were getting along and resolved any possible queries on HF and DM self-management. The first monthly meeting was arranged within a month post discharge/post the first meeting and patients were educated with the main themes regarding HF and DM. Then the meetings were arranged monthly and the content of the educational sessions included: pharmacological and non- pharmacological treatment/self-management actions (low- sodium diet, monitor weight, daily fluid volume, breathing more effectively, coughing techniques, quitting smoking, managing fatigue, coping with stress, medication adherence, physical activity, socializing, relaxation, early detection of decompensation signs, management of diabetes, glucose control).Phone call conducts were also conducted once a month and patients were empowered and discussed various issues that concerned them and they could call the researchers when needed. There was continuing communication and assessment and the ‘SupportHeart’ team tried to find possible solutions and there was referral to available services when needed.
Regular communication supported patients to know how and when they should get help from Health Professionals (HPs) and follow-up check-up. In addition, they were educated how they should make changes regarding their lifestyle modification to reduce the risk of an acute event, build on their own strengths so they can increase their self-efficacy and self-confidence, understand the educational program and benefits of following it, self-manage themselves in a way that reduces the risk of decompensation and understand early signs of decompensation.
Measurements
Survival analysis was studied categorizing it, into acute events and death events due to HF. The acute events were the readmissions, and the Emergency Room visits due to HF. The acute and death events were measured at the period from recruitment to 1 month, after 1 month and until 3 months’ time point after the intervention, after 3 months and until the 6-month time point after the intervention and between 6 months and until 1 year time point after the intervention.
Statistical Analysis
Descriptive statistics were used to present the results. Baseline characteristics were compared using independent samples Welsch t-test when the variables were continuous [(i.e. age, hemoglobin levels (HbA1c)] and the Fisher’s exact test in the case of categorical variables (i.e. sex, comorbidity, etc.). Comparisons between IG and CG at each time point were assessed using a Welsch t-test. Comparisons of lost to follow- up between the two groups, as well as the comparisons of the numbers of acute events between the two groups, were assessed using the Fisher’s exact test.
Results
Demographic and Clinical Characteristics
The sample consisted of 121 patients with HF and DM: 80 (66%) male and 41 (34%) female patients. The mean age of the patients was =73.9 (SD=9.1) years old. Most of the patients were married (55%) and 33% were widowers. Regarding the educational level 56 (46%), 45 (37%) and 11 (9.1%) patients had elementary, secondary and higher education, respectively. Thirty-two patients (26%) had a history of myocardial infarction. All patients had DM2. All demographic characteristics of the participants are shown in Table 1.
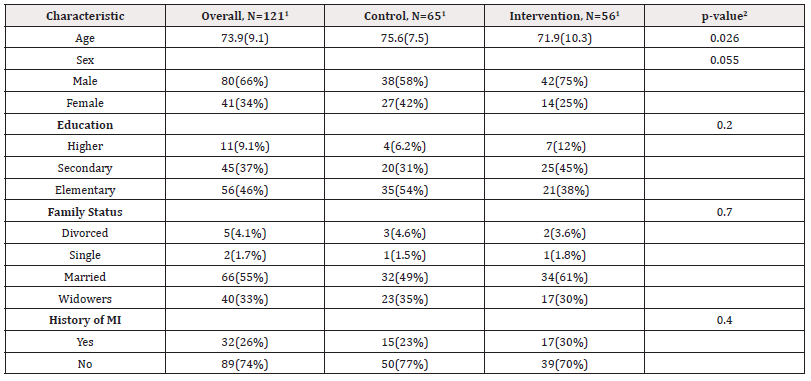
Table 1: Demographic characteristics of the participants (1Mean (SD); n (%), 2Welch Two Sample test; Pearson’s Chi-squared test; Fisher’s exact test).
Many of the participants (N=91-75%) had the underlying disease of Coronary Artery Disease (CAD), 35 (29%) had acute arrythmias, and 22 (18%) had chronic atrial fibrillation. Forty-six (71%) participants who had CAD were found in the CG and forty-five (80%) was found in the IG (p=0.2). Seventeen participants (26%) in the CG had acute arrhythmias and 18 (32%) with acute arrhythmias were in the IG (p=0.5). Twelve (21%) of the participants in the IG had chronic atrial fibrillation and 10 (15%) were found in the CG (p=0.4). The most frequent risk factor from the clinical characteristics was hypertension [94 (78%)], with higher incidence in the CG[56(86%)] compared with the IG[38(68%)] (p=0.016). Similarly, the second more frequent co-existing risk factor was hyperlipidemia which was present in 74 patients with the higher incidence in the IG [37 (66%)] compared with the CG [37 (57%)] (p=0.3). The third risk factor was obesity [19 (16%)] with higher incidence in the CG[11 (17%)] compared with the IG [8 (14%)] (p=0.7). Most of the patients 97(80%) were not active smokers. There were no patients at NYHA I in the current study. Most of the patients were at NYHA stage III [69 (57%)] [CG 35 (54%) and IG 34 (61%)] (p=0.2). HbA1c levels were 7.5 % (0.7) in the CG and 7.1% (0.5) in the IG (p=0.005). All clinical characteristics are presented in Table 2.

Table 2: Clinical characteristics of the participants (1Mean (SD); n (%) 2Welch Two Sample test; Pearson’s Chi-squared test; Fisher’s exact test).
Survival Analysis
Acute Events: Survival analysis was studied categorizing it, into acute events and death events due to HF. At the period from recruitment to 1 month, there were 3/65 (4.6%) acute events for the CG and 2/56 (3.6%) acute events for the IG p>0.9. After 1 month and until 3 months’ time point after the intervention, the CG 7/64 (10.9%) had more acute events compared to the IG 3/56 (5.4%) p=0.51. After 3 months and until the 6-month time point after the intervention, the CG 12/61 (19.7%) had more acute events compared to the IG 6/52 (11.5%) p=0.3. Between 6 months and until 1 year time point after the intervention, the IG (0/49 (0.0%) hadn’t any acute events compared to the CG that had 8/58 (13.8%) p=0.007 acute events (Table 3).
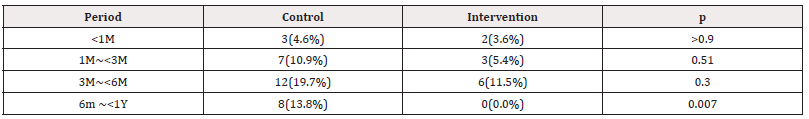
Table 3: Acute Events.
Note*: Proportion at each time-point according to the patients in the study after the dropouts Control: 65, 64, 61, 58 at < M, 1M~3M, 3M~6M, and 6M~1Y respectively, Intervention: 56, 56, 52, 49 at < M, 1M~3M, 3M~6M, and 6M~1Y respectively.
Death Events
There were no significant differences in the mortality across the two groups in all time points; at the period from recruitment to 1 month, there was 1/65 (1.5%) death event for the CG and no death for the IG 0/56 (0.0%) p >0.9. After 1 month and until 3 months’ time point after the intervention, the CG had 2/64 (3.1 %) deaths and the IG 3/56 (5.4%) p=0.66. After 3 months and until the 6-month time point after the intervention, the CG had 3/61 (4.9%) deaths compared with the IG that had 1/52 (1.9%) death p=0.62. Between 6 months and until 1 year time point after the intervention, the CG had 1/58 (1.7%) death event and the IG had 1/49 (2.0%) with p>0.9 (Table 4).

Table 4: Death events.
Note*: Proportion at each time-point according to the patients in the study after the dropouts Control: 65, 64, 61, 58 at < M, 1M~3M, 3M~6M, and 6M~1Y respectively, Intervention: 56, 56, 52, 49 at < M, 1M~3M, 3M~6M, and 6M~1Y respectively.
All Events (Acute Events and Death Events)
When considering both; acute and death events after 6 months and until 1 year time point, the CG [9/58 (15.5%)] showed more acute events compared to the IG [1/49 (2%)] (p=0.02) (Table 5).
Discussion
Previous studies have shown a reduction of 50% in HF re-admissions and 20% in mortality in HF patients who were involved in HF management programs, but results are controversial [16,17]. Mortality reached 10% and 25% of patients after an acute event and patients will be readmitted within the first month after discharge [18]. Some reports support that various factors are responsible for the increased one-month readmission rates, including elevated NYHA classification and treatment with beta-blockers, loop diuretics, thiazide, or nitrates [19]. Retired and/or disabled patients had one or more emergency room visits in the last 3 months and stay in hospital more than 5 days at discharge [20]. In the current study, acute events had lower rate in the IG. Acute events were either readmissions due to fluid overload or emergency room visits. In fact, at the period of recruitment to one month, there were 3/65 (4.6%) acute events in the CG and 2/56 (3.6%) in the IG. After a month and until three months’ time point, in the CG more acute events were observed [7/61(10.9%)] compared to the IG [3/52 (11.5%)]. After three months and until the sixth month time point, in the CG were observed more acute events [12/61(19.7%)] compared to the IG [6/52 (11.5%)]. Between six months to one year was observed 8/58 (13.8%) acute events in the CG and no acute event in the IG [0/49 (0.0%)].
There were no significant differences in the mortality across the two groups (p>0.05) at all time points and the largest different observed between three to six months after the intervention, where 3/61 (4.9%) deaths were observed in the CG and only 1/52 (1.9%) death in the IG. When considering both acute events and mortality after three months and until six-month time point, in the CG [9/58 (15.5 %)] were observed more acute events and deaths compared to the IG [1/49 (2%)] (p=0.02)]. The fact that no patient had any acute event (readmission or emergency room visit) at the time between 6 months to one year in the IG, perhaps was due to the close monitoring during the program and the knowledge patients had about the early recognition of decompensated symptoms [21]. Kalogirou F, et al., support that important issues that a management program should contain, include the knowledge and understanding of HF, self-care, self-efficacy, family and caregiver involvement, psychosocial well-being, HPs support, and technology use. All the above components were involved in the current program for patients with HF and DM and more results are expected from the involvement of family/caregivers and smart watches usage, in the RCT program ‘SupportHeart’. The current supportive management program for HF patients with DM- part of the RCT ‘SupportHeart’-was the only program that was running during the two years of the pandemic of COVID-19 where the communication with the patients continued through digital health technology (phone calls or via viper) so the patients and the members from the ‘SupportHeart’ team, could ‘see’ each other and the communication and the interaction was more effective.
Limitations
The current study has some limitations that need to be considered. This study is a secondary analysis of the RCT ‘SupportHeart’ that studied patients with HF, so the randomization could not be achieved for the particular group of patients (HF patients with DM); therefore, some differences that exist between the IG and the CG at baseline are justified. None of the patients in the study had NYHA I since most of the participants recruited from hospitals and this proves that patients with NYHA I are mostly misdiagnosed and this should be considered in future studies since the ‘SupportHeart’ program can improve the HR-QoL from the early stages of the HF trajectory. This shows the need for new RCTs with a sample exclusively with patients with HF-DM considering more clinical characteristics that may affect the HR-QoL of HF patients with DM. The study sample did not represent all patients with HF-DM due to the exclusion criteria that were set, since patients with dementia or any kind of mental illness, patients under hemodialysis and patients transferred to nursing homes after discharge, were not included in the current study. Also, patients from rural areas were not considered to the sample. Finally, this study was based in pragmatic methodology and pragmatic trials do not most of the times have constraints on patients and clinicians; between patients and HPs from the research team created a ‘bond’ and a relationship since they focused on patients’ needs and was patient-centred; but this may lead to inconsistent or missing data [22].
Conclusions
The current study is the first study that studied the HF-DM population and introduce supportive care in the management of HF patients with the comorbidity of DM. Supportive care was found to be an important factor for HF-DM management programs. The study was effective regarding the reduction of morbidity and mortality for the population of HF-DM patients. The current study is a sub analysis of the ‘SupportHeart’ program, based in pragmatic methodology design, on the ‘real world’ and on the ‘real needs’ of HF patients with DM focused on a patient-centred approach that was missing from previous studies and previous management programs. Future studies should be focused on the population of HF-DM patients and access and apply supportive care management programs in a long-term duration for HF-DM population with the scope to increase their HR-QoL, reduce acute events and make patients actively participants in the management of their chronic conditions, in a continues and long-term support.
Acknowledgements
None.
Conflict of Interest
None.
References
- Guha K, McDonagh T (2013) Heart Failure Epidemiology: European Perspective. Curr Cardiol Rev 9 (2): 123-127.
- EunSeok Cha, Patricia C Clark, Carolyn Miller Reilly, Melinda Higgins, Maureen Lobb, et al. (2012) Educational Needs for Improving Self-Care in Heart Failure Patients with Diabetes. Diabetes Educ 38(5): 673-684.
- Aroor AR, Mandavia CH, Sowers JR (2012) Insulin resistance and heart failure: molecular mechanisms. Heart Fail Clin 8(4): 609-617.
- Ahmed A, Aronow WS, Fleg, JL (2006) Higher New York Heart Association classes and increased mortality and hospitalizations in heart failure patients with preserved left ventricular function. Am Heart J 151(2): 444-450.
- MacDonald MR, Petrie MC, Varyani F, Ostyergren J, Michelson EL, et al. (2008) Impact of diabetes on outcomes in patients with low and preserved ejection fraction heart failure: an analysis of the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) programme. Eur Heart J 29(11): 1377-1385.
- Aquilar D, Deswal A, Ramasubbu K, Mann DL, Bozkurt B (2010) Comparison of patients with heart failure and preserved ejection fraction among those with versus without diabetes mellitus. Am J Cardiol 105(3): 373-377.
- Lambrinou E, Protopapas A, Christoforou N, Vouri N, Malaktou A, et al. (2020) Diabetes and female gender are found to increase the hazard of deterioration? Results from the MEETinCY trial. European Heart Journal.
- Philippou K (2023) Supportive care in the management of patients with heart failure and diabetes mellitus (PhD Thesis).
- Clark A, Freydberg C, McAlister F, Tsuyuki R, Armstrong P, et al. (2009) Patient and informal caregivers’ knowledge of heart failure: necessary but insufficient for effective self-care. European J Heart Fail 11(6): 617-621.
- Gallagher R, Luttik M, Jaarsma T (2011) Social Support and self-care in Heart Failure. J Cardiovasc Nurs 26 (6): 439-445.
- Ahmedzai SH, Muers MF (2005) The nature of palliation and its contribution to supportive care. In: Supportive care in respiratory disease.
- Kyriakou M, Deaton C, Samara A, Philippou K, Lakatamitou I, et al. (2019) What HF patients really need? A systematic review and meta-synthesis. European J Heart Fail 21(Sup1): 470.
- Philippou K (2024) Could Pragmatic Clinical Trials be Effective in the Management of Patients with Heart Failure? Am J Biomed Sci & Res 22(3): 335-336.
- McHugh M (2008) Power analysis in research, Biochemia Medical 18(3): 263-274.
- Giuseppe M, Rosano C Gianluigi S (2023) Implementing an earlier and more intensive follow-up in acute heart failure: the STRONG-HF and COACH trials. Nat Rev Cardiol 20(4): 213-214.
- Lambrinou E, Kalogirou F, Lamnisos D, Sourtzi P (2012) Effectiveness of heart failure management programmes with nurse-led discharge planning in reducing re-admissions: A systematic review and meta-analysis. Int J Nurs Stud 49(5): 610-624.
- McDonald JH (2014) Handbook of Biological Statistics (3rd ed.) 77-85.
- Driscoll A, Meagher S, Kennedy R, Melanie Hay, Jayant Banerji, et al. (2016) What is the impact of systems of care for heart failure on patients diagnosed with heart failure: a systematic review. BMC Cardiovasc Disord 16(1): 195.
- Aizawa H, Imai S, Fushimi K (2015) Factors associated with 30-day readmission of patients with heart failure from a Japanese administrative database. BMC Cardiovasc Disord 15(1): 134.
- Bradford C, Shah BM, Shane P, Wachi N, Sahota K (2017) Patient and clinical characteristics that heighten risk for heart failure readmission. Res Social Adm Pharm 13(6): 1070-1081.
- Kalogirou F, Forsyth F, Kyriakou M, Mantle R, Deaton C (2020) Heart failure disease management: a systematic review of effectiveness in heart failure with preserved ejection fraction. ESC Heart Fail 7(1): 194-212.
- Sox H, Lewis R (2016) Pragmatic trials: practical answers to ‘‘Real World’’ questions. JAMA 316(11): 1205-1206.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.